Abstract
Multidisciplinary treatment approaches are common for chronic diseases like cardiovascular disease, but obesity treatment remains largely siloed. Increasing efficiency in obesity treatment is crucial to improving financial and clinical outcomes. The Allegheny Health Network established a metabolic center consisting of bariatric surgeons, specialists in bariatric medicine, and endocrinologists specializing in diabetes care, who together developed an obesity treatment algorithm to address this need and to improve clinical outcomes through research, continuing education, and primary care outreach. This correspondence provides insights into the development and implementation of the metabolic center and presents the algorithm used to select a patient’s obesity treatment based on their individual phenotype, characteristics, and contraindications. The Alleghany Health Network may be used as a model for the necessary development of similar comprehensive, multidisciplinary obesity specialty centers.
Keywords: Algorithms, Health systems, Obesity, Weight management program
While chronic diseases such as cardiovascular disease are treated with a multidisciplinary approach, obesity treatment remains largely siloed and inefficient [1]. There is an unmet clinical and financial need for comprehensive, multidisciplinary weight management centers to decrease inefficiency in spending and improve health care for patients with obesity. The goals of a specialty metabolic center should include establishing excellence in clinical care, serving as a resource to primary care, conducting research into innovative and efficient treatment, and providing continuing education.
The Allegheny Health Network established a metabolic center and developed an obesity treatment algorithm to address this unmet need. A pilot program was initiated prior to the development of the full metabolic center. A small team of specialists demonstrated proof of concept, and the program demonstrated financial viability. In the pilot, 25% of patients initially opposed to bariatric surgery eventually converted to surgery after other treatment modalities (18% of patients did not respond well to medication), generating enough income from bariatric surgery and other treatments to provide financial stability. Generally, patients who eventually converted to bariatric surgery were older and had a higher body mass index (BMI), suggesting that this population has a particular need to be seen at a specialty metabolic center.
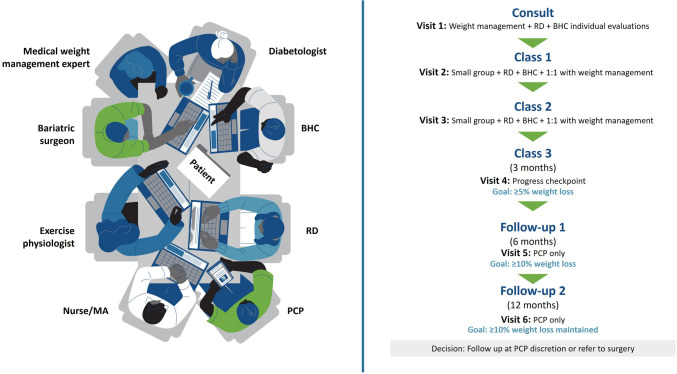
Management of obesity at the Allegheny Health Network metabolic center is focused on the four pillars of obesity treatment: nutrition, physical activity, behavioral modification, and medical management [2]. A team of specialists is established to effectively address this broad range of topics. Within this multidisciplinary team, a “care path” is established and followed using tools built into the medical records software Epic to support patients in reaching their goals (Fig. 1). First, a weight management specialist evaluates the patient, reviewing family history, medications, and lifestyle factors; identifies and assesses the severity of co-occurring conditions; excludes common causes of weight gain (e.g., thyroid dysfunction, diabetes, metabolic syndrome); and discusses all available treatment options (medical and surgical). Patients are then recommended to classes in small groups focused on addressing their specific needs (e.g., nutrition, physical activity, and behavior modification). Throughout the care path, integration of medical records and laboratory results enables efficient coordination of care among the various health care specialists participating in each patient’s care.
Fig. 1.
Care path for patients with obesity. BHC, behavioral health consultant; MA, medical assistant; PCP, primary care professional; RD, registered dietitian
Efficiency and quality of care are maintained through the use of a center-specific obesity treatment algorithm (Fig. 2). As part of their treatment, all patients undergoing weight-loss care receive referrals to behavioral health and dietary teams and are given behavioral health, nutritional, and physical activity homework in their after-visit summaries. During the 1 to 3 months following treatment initiation, routine follow-up appointments are required. The course of treatment is altered if patients on injectable obesity management medication (OMM) do not achieve 5% total body weight loss after 3 months of treatment or 10% by 6 months.
Fig. 2.
Treatment algorithm for patients with obesity. The treatment algorithm represented here is used at a single metabolic center and contains off-label use of lisdexamfetamine, topiramate, naltrexone monotherapy, and bupropion monotherapy, which are not approved by the FDA for the treatment of obesity [2–5]. BMI, body mass index; CVD, cardiovascular disease; FDA, US Food and Drug Administration; GIP, glucose-dependent insulinotropic peptide; GLP-1R, glucagon-like peptide-1 receptor agonists; NB-ER, fixed-dose extended-release combination of naltrexone and bupropion; OMM, obesity management medication
In the treatment algorithm, injectable medications, a combination of surgery and an OMM, or 2 OMMs may be considered for patients with a BMI ≥ 35 kg/m2. Injectable OMMs or surgery are also considered for patients with cardiovascular disease, type 2 diabetes mellitus, or high-risk atherosclerotic cardiovascular disease. Similarly, if oral OMMs are contraindicated or if the patient has reported adverse effects or a history of inefficacy (< 5% body weight loss at 3 months) with oral OMMs, injectable OMMs may be considered. Patients on injectable OMMs, such as glucagon-like peptide-1 (GLP-1) receptor agonists, who do not achieve their weight-loss goals are referred for bariatric surgery. The use of alternative injectable OMMs is discouraged in patients who have not previously responded to injectable medications, due to the unlikelihood of a treatment response.
In general, oral OMMs are underutilized, and they are encouraged as first-line treatment for patients with a BMI ≥ 30 kg/m2 and < 35 kg/m2 at the metabolic center. In the treatment algorithm, OMMs are selected based on individual patient characteristics and specific contraindications (Table 1). Phentermine, lisdexamfetamine, phentermine-topiramate, or topiramate are recommended by the Allegheny Health Network metabolic center for patients with a large appetite, lack of satiety, or binge eating [2]. Fixed-dose extended-release combination of naltrexone and bupropion (NB-ER), bupropion, naltrexone, and topiramate are recommended for patients with emotional eating, cravings, co-occurring smoking or depression, night eating, snacking, or grazing [6–8]. Patients with metabolic dysfunction–associated steatohepatitis also start on oral OMMs unless they have contraindications, a history of inefficacy, or a BMI > 35 kg/m2.
Table 1.
Contraindications and alternative OMMs for patients with obesity
| Phentermine-topiramate | Phentermine | Lisdexamfetamine | Topiramate | NB-ER | Bupropion | |
|---|---|---|---|---|---|---|
| Contraindications |
• Kidney stones [2] • Planning pregnancy/lack of reliable contraception [2] • Uncontrolled hypertension, history of intracranial hypertension, stroke, or CVD [2] • Glaucoma [2] |
• ADHD treatment • Uncontrolled hypertension, history of intracranial hypertension, stroke, or CVD [2] • Glaucoma [2] • Treatment for anxiety or bipolar disorder (except SSRIs) |
• ADHD treatment • Uncontrolled hypertension, history of intracranial hypertension, stroke, or CVD [2] • Glaucoma [2] |
• Planning pregnancy/lack of reliable contraception [2] • Treatment for some psychological conditions, such as MAOIs |
• Tamoxifen [4] • Uncontrolled hypertension, history of intracranial hypertension, stroke, or CVD [9] • Treatment for some psychological conditions, such as MAOIs [9] |
• Tamoxifen [4] • Uncontrolled hypertension, history of intracranial hypertension, stroke, or CVD [4] • Treatment for some psychological conditions, such as MAOIs [4] |
| Instead prescribe |
• Phentermine • Topiramate • NB-ER • Naltrexone • Bupropion |
• Topiramate • NB-ER • Naltrexone • Bupropion |
• Topiramate • NB-ER • Naltrexone • Bupropion |
• Phentermine • Naltrexone |
• Topiramate • Naltrexone |
• Topiramate • Naltrexone |
The treatment algorithm represented here is used at a single metabolic center and contains off-label use of lisdexamfetamine, topiramate, naltrexone monotherapy, and bupropion monotherapy, which are not approved by the FDA for the treatment of obesity [2–5]
ADHD, attention deficit/hyperactivity disorder; CVD, cardiovascular disease; FDA, Food and Drug Administration; MAOI, monoamine oxidase inhibitor; NB-ER, the fixed-dose extended-release combination of naltrexone and bupropion; OMM, obesity management medication; SSRI, selective serotonin reuptake inhibitor
It is important to note that this algorithm includes the use of lisdexamfetamine and monotherapy with topiramate, naltrexone, and bupropion, which have not been approved by the US Food and Drug Administration for the treatment of obesity [2–5], and phentermine has only been approved for short-term use [2]. Moreover, monotherapy with naltrexone or bupropion is associated with low efficacy for the management of obesity [10].
Future goals for the Allegheny Health Network specialty metabolic center include increasing efficiency in providing patients with effective and standardized care. The multidisciplinary approach and the use of a treatment algorithm described here may serve as a model for the development of other metabolic specialty centers to more widely improve treatment for patients with obesity.
Acknowledgements
Medical writing support was provided by Breanne E. Pirino, PhD, of Red Nucleus, and funded by Currax Pharmaceuticals, LLC.
Author Contribution
All authors contributed to the development of the treatment algorithm described and reviewed and approved the submitted manuscript.
Funding
The authors were not compensated for their participation in this project. Medical writing and editorial support were provided by Breanne E. Pirino, PhD, of Red Nucleus, and were funded by Currax Pharmaceuticals, LLC.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Competing Interests
GME reports receiving payments or honoraria from Gore, Lilly, Medtronic, and Novo Nordisk. MS and FZ report no conflict of interest.
Footnotes
The original version of this article was revised due to a retrospective Open Access order.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
4/4/2025
A Correction to this paper has been published: 10.1007/s11695-025-07849-x
References
- 1.Batchelor WB, Anwaruddin S, Wang DD, et al. The multidisciplinary heart team in cardiovascular medicine: current role and future challenges. JACC Adv. 2023;2(1):1–13. 10.1016/j.jacadv.2022.100160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tondt J, Freshwater M, Benson-Davies S, et al. Obesity algorithm. Obesity Medicine Association; 2024. Accessed July 30, 2024. https://obesitymedicine.org/resources/obesity-algorithm/
- 3.Revia (naltrexone HCl). Package insert. Duramed Pharmaceuticals, Inc.; 2013.
- 4.Zyban (bupropion HCl). Package insert. GSK; 2021.
- 5.Topamax (topiramate). Package insert. Janssen; 2017.
- 6.Acosta A, Camilleri M, Abu Dayyeh B, et al. Selection of antiobesity medications based on phenotypes enhances weight loss: a pragmatic trial in an obesity clinic. Obesity (Silver Spring). 2021;29(4):662–71. 10.1002/oby.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilcox CS, Oskooilar N, Erickson JS, et al. An open-label study of naltrexone and bupropion combination therapy for smoking cessation in overweight and obese subjects. Addict Behav. 2010;35(3):229–34. 10.1016/j.addbeh.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Winkelman JW, Wipper B, Purks J, Mei L, Schoerning L. Topiramate reduces nocturnal eating in sleep-related eating disorder. Sleep. 2020;43(9):1–7. 10.1093/sleep/zsaa060. [DOI] [PubMed] [Google Scholar]
- 9.Contrave (naltrexone bupropion ER). Package insert. Currax; 2023.
- 10.Greenway FL, Whitehouse MJ, Guttadauria M, et al. Rational design of a combination medication for the treatment of obesity. Obesity (Silver Spring). 2009;17(1):30–9. 10.1038/oby.2008.461. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.