Abstract
Recombinant human metapneumovirus (HMPV) in which the SH, G, or M2 gene or open reading frame was deleted by reverse genetics was evaluated for replication and vaccine efficacy following topical administration to the respiratory tract of African green monkeys, a permissive primate host. Replication of the ΔSH virus was only marginally less efficient than that of wild-type HMPV, whereas the ΔG and ΔM2-2 viruses were reduced sixfold and 160-fold in the upper respiratory tract and 3,200-fold and 4,000-fold in the lower respiratory tract, respectively. Even with the highly attenuated mutants, there was unequivocal HMPV replication at each anatomical site in each animal. Thus, none of these three proteins is essential for HMPV replication in a primate host, although G and M2-2 increased the efficiency of replication. Each gene-deletion virus was highly immunogenic and protective against wild-type HMPV challenge. The ΔG and ΔM2-2 viruses are promising vaccine candidates that are based on independent mechanisms of attenuation and are appropriate for clinical evaluation.
Since it was first reported in 2001 (29), human metapneumovirus (HMPV) has been isolated in patients throughout the world and has quickly come to be recognized as a major etiologic agent for respiratory disease primarily in very young, elderly, and immunocompromised individuals (10, 12, 30). HMPV accounts for roughly 5 to 15% of respiratory disease in hospitalized young children, with children under 2 years of age being most at risk for serious HMPV infections (1, 7, 11, 18, 20, 33). Clinical symptoms resemble those caused by human respiratory syncytial virus (HRSV) (15, 31). The disease burden associated with HMPV remains to be fully defined but appears to be sufficient to warrant the development of a vaccine, especially for the pediatric population.
HMPV is an enveloped virus belonging to the Metapneumovirus genus of the subfamily Pneumovirinae, family Paramyxoviridae, order Mononegavirales (16). Its genome is a negative-strand RNA of 13 kb that contains eight genes in the order 3′-N-P-M-F-M2-1/M2-2-SH-G-L-5′ and encodes nine proteins (3, 28). The HMPV proteins are the following: N, nucleoprotein; P, phosphoprotein; M, matrix protein; F, fusion protein; M2-1, product of the first open reading frame (ORF) in the M2 mRNA; M2-2, product of the second ORF in the M2 mRNA; SH, small hydrophobic glycoprotein of unknown function; G, putative attachment glycoprotein; and L, viral polymerase. In most cases, the assignments of protein functions are tentative and based on extrapolation from HRSV.
We previously developed a reverse genetic system for generating complete infectious recombinant HMPV (rHMPV) from cDNA based on a clinical isolate, CAN97-83, that is a member of subgroup A (4). The cDNA-derived rHMPV was designed to differ from CAN97-83 only by four nucleotide substitutions involved in creating an NheI site in the M-F intergenic region. The consensus sequence of recovered rHMPV was confirmed in its entirety, verifying the fidelity of the system. Mutant viruses were previously constructed in which the SH and G genes were deleted individually or in combination (ΔSH, ΔG, and ΔSH/G viruses) (5) or in which the M2-1 and M2-2 ORFs—which overlap in the M2 gene and encode independent protein products—were silenced individually (ΔM2-1 and ΔM2-2) or in which the complete M2 gene was deleted (ΔM2[1+2]) (8). The ΔSH, ΔG, and ΔM2-2 viruses are illustrated in Fig. 1. In the hamster model, deletion of the SH gene had no apparent effect on the efficiency of replication, whereas deletion of the G gene reduced replication in the upper and lower respiratory tract 900- and 50-fold, respectively (5). Viruses lacking either or both the SH and G genes induced a high level of HMPV-neutralizing antibodies and a high level of protection against challenge with wild-type HMPV. The effects of deletions involving the M2 gene were more dramatic. Replication of virus lacking the M2-2 ORF was detected only in the upper respiratory tract in one out of 12 hamsters and at very low titer. Nonetheless, this virus induced a high level of HMPV-neutralizing serum antibodies in each animal and a high level of protection against HMPV challenge, confirming that a low level of replication had occurred. In contrast, virus lacking the M2-1 ORF, either alone or in combination with the M2-2 deletion, did not replicate detectably and did not induce significant levels of HMPV-neutralizing antibodies or protection.
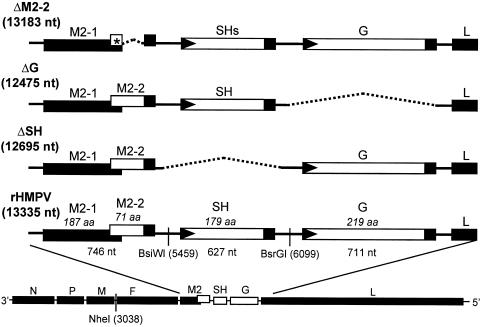
FIG. 1.
Structures of the genomes of rHMPV and the ΔSH, ΔG, and ΔM2-2 gene deletion mutants. The wild-type rHMPV genome is shown at the bottom, drawn approximately to scale. The expanded view (not to scale) shows the M2-SH-G genome region. The genes are shown as open rectangles flanked on the upstream and downstream ends by the gene start (filled triangles) and gene end (filled boxes) transcription signals, respectively. The nucleotide length of each gene is listed underneath, and the calculated amino acid length of its encoded protein is given in italics above. Intergenic regions are shown as horizontal lines. The deletions in the ΔSH and ΔG viruses are indicated by dotted lines and involved 640 and 860 nucleotides, respectively (5). The M2-2 ORF was silenced by deleting 152 nucleotides and introducing stop codons (star) in the remnant ORF (8). Also shown are the NheI, BsiWI, and BsrGI sites together with their nucleotide positions in the antigenomic RNA sequence. The genome lengths of the recombinant viruses are indicated to the left.
In the present study, we evaluated three of these viruses, ΔSH, ΔG, and ΔM2-2 (Fig. 1), for the ability to replicate in a permissive nonhuman primate host, the African green monkey (AGM; Chlorocebus aethiops). One purpose was to determine the status of each protein as essential or nonessential in a host that is anatomically and phylogenetically more closely related to humans than hamsters. In addition, we evaluated the immunogenicity and protective efficacy of these viruses as intranasal vaccine candidates. The ΔSH and ΔG viruses were from the same preparations as used in a previous hamster study (5). The ΔM2-2 virus was a new version that was prepared in an HMPV backbone in which the naturally occurring SH gene was replaced by a modified version called “stabilized SH” (SHs). Specifically, a number of naturally occurring A and T homooligomer tracts in the SH gene were modified so that individual A or T residues were replaced by C or G (not shown). These substitutions interrupted these tracts with no change in amino acid coding. This was done because we recently realized that some virus preparations appear to contain subpopulations with one or more small insertions in these tracts within the SH gene, perhaps due to stuttering by the viral polymerase. This phenomenon is being studied and will be reported in detail in the future, but in the meantime we are incorporating SHs into each new recombinant HMPV to preclude this problem. We found that wild-type rHMPV bearing the SHs gene replicated with the same efficiency as unmodified rHMPV in vitro and in the respiratory tract of hamsters (not shown), indicating a lack of effect of SHs on these biological properties, as might be expected. We confirmed the complete genomic consensus sequence of the ΔM2-2 virus bearing the SHs gene, noting both the correct sequence as well as a lack of detectable mutant subpopulations. Furthermore, in all of the final virus preparations that were used in this study, we confirmed the sequence and lack of detectable subpopulations for the region from position 4656 (downstream end of the F gene) to 7499 (upstream end of the L gene).
Replication in AGMs.
Replication of rHMPV and the deletion mutants was evaluated in the respiratory tract of AGMs, a primate host in which HMPV replicates efficiently (24). Indeed, captive cohorts of these animals frequently have a high seroprevalence for HMPV, which likely reflects infection from their human handlers and perhaps transmission between animals. AGMs that were identified as being negative for HMPV-neutralizing serum antibodies (<2.8 log2) were inoculated intranasally and intratracheally with 106.0 50% tissue culture infective doses (TCID50) of virus per site (Table 1). To monitor virus replication in the upper and lower respiratory tracts, nasopharyngeal swabs and tracheal lavage samples were collected at intervals over 12 days postinfection and were subsequently assayed for virus titer (Table 1). The AGMs were monitored daily for clinical symptoms.
TABLE 1.
Level of replication of gene-deletion rHMPVs in the upper and lower respiratory tracts of AGMs
| Virusa | Nasopharyngeal swab
|
Tracheal lavage
|
||||
|---|---|---|---|---|---|---|
| Mean peak titer (log10 PFU/ml ± SE)b and statistical groupingc | Reduction of mean peak titerd (log10 PFU/ml) | Duration of shedding (day ± SE)e | Mean peak titer (log10 PFU/ml ± SE)b and statistical groupingc | Reduction of mean peak titerd (log10 PFU/ml) | Duration of shedding (day ± SE)e | |
| CAN97-83 | 4.1 ± 0.1 A | 9.0 ± 0.0 | 5.4 ± 0.7 A | 7.0 ± 0.0 | ||
| rHMPV | 3.9 ± 0.2 A | 9.0 ± 0.4 | 5.7 ± 0.3 A | 10.0 ± 1.0 | ||
| ΔSH | 3.5 ± 0.4 A | 0.4 | 8.0 ± 0.9 | 4.9 ± 0.3 A | 0.8 | 8.0 ± 1.0 |
| ΔG | 3.1 ± 0.1 A | 0.8 | 9.0 ± 0.0 | 2.2 ± 0.6 B | 3.5 | 5.0 ± 1.4 |
| ΔM2-2 | 1.7 ± 0.2 B | 2.2 | 6.8 ± 0.5 | 2.1 ± 0.2 B | 3.6 | 4.0 ± 1.0 |
HMPV-seronegative AGMs in groups of four, except for the CAN97-83 group that comprised two animals, were inoculated on day 0 by the combined intranasal and intratracheal routes with 106.0 TCID50 of the indicated virus in 1 ml per site. Nasopharyngeal swabs were collected daily on days 1-10 and 12 and tracheal lavages were collected on days 2, 4, 6, 8, 10, and 12.
Virus titers were determined by plaque assays on Vero cells under methylcellulose overlay containing 5 μg/ml trypsin. The cultures were incubated at 32°C for 6 days, and plaques were visualized by immunostaining with a rabbit antiserum raised against gradient-purified CAN97-83 (4). The level of virus replication is expressed as the geometric mean of the peak virus titers (log10 PFU/ml ± standard error) for the animals in each group irrespective of sampling day. The lower limit of detection is 0.7 log10 PFU/ml. A value of 0.7 log10 PFU/ml was assigned to samples with no detectable virus for the purpose of calculating means.
Mean peak virus titers were assigned to statistically similar groups by the Tukey-Kramer post hoc test. Values within a column that share a common letter are not significantly different, whereas those that do not are significantly different (P < 0.05).
Reduction of mean peak titer compared to rHMPV.
The period of days from the first to the last day on which virus was recovered, including negative days (if any) in between.
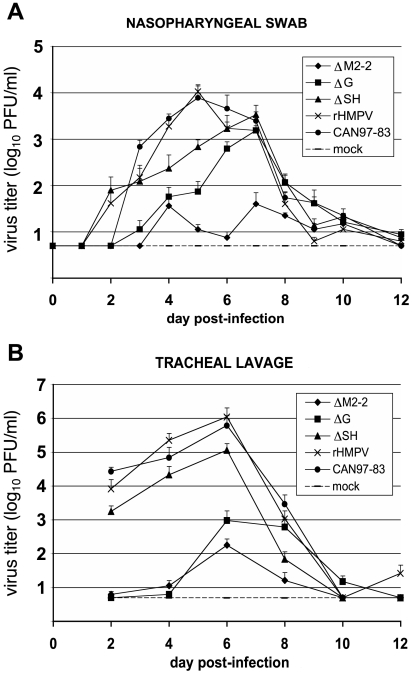
Biologically derived CAN97-83 virus and rHMPV were essentially equivalent in their kinetics of replication (Fig. 2) and mean peak titer (4.1 ± 0.1 versus 3.9 ± 0.2 in the upper and 5.4 ± 0.7 versus 5.7 ± 0.3 in the lower respiratory tracts, respectively) (Table 1). This indicated that rHMPV replicated with wild-type-like efficiency in this primate host, functionally confirming the HMPV consensus sequence as that of a wild-type virus. The ΔSH mutant replicated to a mean peak titer comparable to that of CAN97-83 and rHMPV in the upper and lower respiratory tracts, with a similar duration of shedding (Table 1). However, there appeared to be a shift in the kinetics of virus replication in the upper respiratory tract, with the peak of viral shedding reached on day 7 postinfection by ΔSH compared to day 5 for the wild-type viruses (Fig. 2A). Replication of the ΔG virus in the upper respiratory tract was reduced sixfold compared to rHMPV and that of the ΔM2-2 virus was reduced 160-fold (2.2 log10). In each case, the kinetics of replication in the upper respiratory tract were retarded slightly as described above for the ΔSH virus, with the peak at day 7 rather than day 5. The duration of shedding was reduced only for the ΔM2-2 virus (6.8 days versus 8 to 9 days). In the lower respiratory tract, the replication of the ΔG and ΔM2-2 viruses was reduced 3,200-fold and 4,000-fold, respectively, compared to rHMPV (Table 1 and Fig. 2B), and the duration of shedding was reduced for both viruses (4 to 5 days) compared to the others (7 to 10 days). Overall, the ΔM2-2 virus appeared to be somewhat more attenuated than ΔG. Each animal that was infected with the ΔG or ΔM2-2 virus shed virus from both the upper and lower respiratory tracts, indicating that virus replication occurred in each animal despite the high level of attenuation. None of the 20 AGMs showed any signs of illness during the experiment with regard to body temperature, weight loss, and nasal discharge, although a small loss of appetite measured by biscuit consumption was evident in monkeys infected with CAN97-83 or rHMPV on the days of the peak virus titer (not shown).
FIG. 2.
Kinetics of replication of biologically derived HMPV CAN97-83, rHMPV, and the gene deletion mutants in the upper and lower respiratory tracts of African green monkeys. Four animals per group, except for the CAN97-83 and control (mock) groups composed of two animals, were inoculated by the combined intranasal and intratracheal routes by using a 1-ml inoculum per site containing 106.0 TCID50 of the indicated virus on day 0. The nasopharyngeal swab (A) and tracheal lavage (B) specimens were taken on the indicated days, and the titers of shed virus were quantified by plaque assay. The detection limit was 0.7 log10 PFU/ml.
Immunogenicity and protective efficacy.
Serum samples were taken on day 0 prior to the immunizing infection and on days 21, 28, and 35 postimmunization. The data for days 0 and 28 are shown in Table 2; the data for days 21 and 35 were consistent with those of day 28 and are not shown. Each immunized animal developed a high titer of HMPV-neutralizing serum antibodies, ranging from 8.1 ± 0.8 log2 for CAN97-83 to 6.8 ± 0.4 log2 for ΔM2-2 (Table 2). There was a trend toward lower antibody titers for the more attenuated ΔG and ΔM2-2 viruses, but the differences compared to CAN97-83 and rHMPV were not statistically significant (Table 2).
TABLE 2.
Immunogenicity and protective efficiency of gene-deletion rHMPVs in AGMs
| Immunizing virusa | Mean serum neutralizing antibody titer (log2 ± SE)b
|
Challenge virus replication
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre- immunization | 28 days postimmunization and statistical groupingc | 28 days postchallenge | Nasopharyngeal swab
|
Tracheal lavage
|
|||||
| Mean peak titer (log10 PFU/ml ± SE)d | Duration of shedding (day ± SE)e | % of shedding | Mean peak titer (log10 PFU/ml ± SE)d | Duration of shedding (day ± SE)e | % of shedding | ||||
| Mock | <2.8 | <2.8 | 8.0 ± 0.3 | 4.8 ± 0.1 | 7.0 ± 0.0 | 100 | 5.2 ± 0.3 | 5.0 ± 0.0 | 100 |
| CAN97-83 | <2.8 | 8.1 ± 0.8 A | 8.3 ± 0.8 | 1.2 ± 0.2 | 3.0 ± 0.0 | 100 | <0.7 | 0.0 ± 0.0 | 0 |
| rHMPV | <2.8 | 7.9 ± 0.5 A | 7.6 ± 0.3 | 1.3 ± 0.1 | 5.0 ± 0.8 | 100 | <0.7 | 0.0 ± 0.0 | 0 |
| ΔSH | <2.8 | 7.7 ± 0.4 A | 8.7 ± 0.6 | 1.2 ± 0.1 | 4.5 ± 0.5 | 100 | <0.7 | 0.0 ± 0.0 | 0 |
| ΔG | <2.8 | 7.3 ± 0.2 A | 8.5 ± 0.2 | 1.5 ± 0.1 | 6.5 ± 0.5 | 100 | 0.7 | 0.3 ± 0.3 | 25 |
| ΔM2-2 | <2.8 | 6.8 ± 0.4 A | 7.5 ± 0.3 | 1.7 ± 0.1 | 7.0 ± 0.0 | 100 | 0.7 | 0.5 ± 0.3 | 50 |
The groups of AGMs are identified by the virus used in the initial immunizing infection as described in Table 1. The mock group is an additional group of 2 animals that were shown in Figure 2 and had been mock infected in parallel with the other groups.
Sera were collected on days 0 and 28 following the first infection, and the neutralizing antibody titer against HMPV was determined using an endpoint dilution assay based on neutralization of an HMPV recombinant expressing green fluorescent protein (6). The neutralization titer was calculated as the highest dilution of antibody at which half of the cultures were negative for infection (no GFP expression) as defined by Reed and Muench (21). The pre-infection anti-HMPV serum titers were <2.8 (reciprocal log2) for all animals in the study.
Mean antibody titers were assigned to statistically similar groups by the Tukey-Kramer post hoc test. Values within a column that share a common letter are not significantly different (P < 0.05).
On day 35, AGMs from each group were challenged intranasally and intratracheally with 106.0 TCID50 of CAN97-83 in 1 ml per site. Nasopharyngeal swabs and tracheal lavages were collected on days 2, 4, 6, and 8 postchallenge. The level of virus replication is expressed as the geometric mean of the peak virus titers (log10 PFU/ml ± standard error) for the animals in each group irrespective of sampling day. The lower limit of detection is 0.7 log10 PFU/ml. A value of 0.7 log10 PFU/ml is assigned to samples with no detectable virus.
The period of days from the first to the last day on which virus was recovered, including negative days (if any) in between.
To evaluate protective efficacy, the AGMs were challenged on day 35 postimmunization by the combined intranasal and intratracheal routes with 106.0 TCID50 of CAN97-83 per site. Challenge virus replication was monitored by collecting nasopharyngeal swabs and tracheal lavage fluids on days 2, 4, 6, and 8 postchallenge (Table 2). The animals that had been mock immunized shed challenge virus with mean peak titers comparable to those observed for CAN97-83 and rHMPV after the initial immunization, as expected. Also as expected, challenge virus replication was highly restricted in the upper and lower respiratory tract of AGMs previously immunized with CAN97-83 or rHMPV, with only trace amounts of shedding detected in the upper respiratory tract and no shedding detected in the lower respiratory tract. Animals that had been infected with the ΔSH virus also had only a trace amount of virus shedding in the upper respiratory tract and none in the lower tract. This high degree of protection is consistent with the efficient replication of the ΔSH virus during the initial immunization.
Immunization with ΔG and ΔM2-2 viruses also was highly protective. In both groups, traces of challenge virus replication were detected in the lower respiratory tract in only one or two of the four immunized animals of each group, respectively. These animals had a very short duration of shedding (mean duration of shedding, 0.3 days for ΔM2-2 or 0.5 days for ΔG, compared to 5 days for the control group) and a low mean peak titer of 0.7 log10 PFU/ml, just above the detection limit, corresponding to a 32,000-fold reduction in replication. Challenge virus replication also was highly restricted in the upper respiratory tract, with a 2,000-fold (ΔG) or 1,250-fold (ΔM2-2) reduction compared to challenge virus replication in the mock immunized group, i.e., not significantly different from protection afforded by immunization with rHMPV. However, the duration of shedding was longer than that observed for the rHMPV- or rHMPVΔSH-immunized animals, and shedding was detected in every animal in each group.
Serum samples were collected 28 days following the challenge, and the titer of HMPV-neutralizing antibodies was determined (Table 2). In the mock-infected control group, the mean postchallenge titer of HMPV-neutralizing serum antibodies was comparable to that induced by immunization with CAN97-83 during the initial immunization (8.1 ± 0.3 for the mock group on day 28 postchallenge versus 8.1 ± 0.8 for CAN97-83 on day 28 postimmunization), as would be expected. For animals that had been immunized with any of the viruses, including the highly attenuated ones, there was no significant increase in the HMPV-neutralizing serum antibody titers following the HMPV challenge. This might mean that immunization with any of the recombinants used in this study induced immunity to HMPV that was strong enough to control HMPV challenge infection below the level of replication that is necessary for boosting the humoral immune response.
For any virus, the identification of the viral genes and gene products that are not essential for virus replication in vivo is an important consideration. In this regard, it is particularly important to assess these effects in a host that is permissive to virus replication and is closely related anatomically and phylogenetically to the natural host. The present study shows that the SH, G, and M2-2 genes and ORFs and their encoded proteins are dispensable for HMPV replication in a primate host, although G and M2-2 contributed substantially to the efficiency of replication. The finding that deletion of the SH gene had little effect on virus replication in vivo is similar to results with HRSV, where the deletion of SH reduced virus replication approximately 10-fold in seronegative chimpanzees (32), whereas in seronegative children the SH deletion did not have a significant attenuating effect in the context of a backbone containing attenuating point mutations (13, 14). It is remarkable that this pneumoviral protein of unknown function appears to be completely dispensable for efficient replication in vivo. In hamsters, replication of the ΔM2-2 virus was not detectable in most of the animals (8), but the present study in AGMs showed that M2-2 augments replication in vivo but is not essential for replication. As is the case with HRSV, the HMPV M2-2 protein appears to play a regulatory role in shifting the balance of RNA synthesis from transcription to RNA replication (2, 8); in any case, its function(s) clearly is not essential for virus replication in vivo. Finally, the HMPV G protein is also dispensable for replication in a primate host. In the cases of HRSV and bovine RSV, it was not clear whether ΔG virus could replicate in primate and bovine hosts, respectively (13, 22, 26, 27), but in the present study replication of the HMPV ΔG virus was unequivocal. It seems remarkable that replication in vivo by HMPV lacking the G protein was sufficiently robust to be detected over a 9-day period. This strongly suggests that viral attachment function can be supplied by another viral protein, which presumably is F since SH and G are dispensable.
Gene-deletion viruses also represent potential vaccine candidates that, in particular, should have the highly desirable property of genetic stability. The G and M2-2 deletions each provided a high degree of attenuation with little or no decrease in immunogenicity or protective efficacy compared to wild-type HMPV, and ΔM2-2 appeared to be somewhat more attenuated than ΔG. The fact that we now have two highly attenuated and immunogenic vaccine candidates that differ somewhat in their degree of attenuation increases the likelihood that one of them will prove to be appropriately attenuated in clinical trials. We previously showed that deletion of the HMPV M2-2 protein resulted in a decrease in RNA replication and an increase in gene expression in cell culture (8), which also was the case with HRSV (2). This has the potential to provide greater antigen synthesis and immunogenicity in vivo. In the present study, the ΔM2-2 mutant was significantly more attenuated than the other viruses and yet did not differ significantly in its immunogenicity or protective efficacy. While this might be indicative of increased immunogenicity—which also was suggested from the results of the previous hamster study—additional data will be needed to substantiate this point. In the case of the ΔG virus, it might seem counterproductive to base attenuation on the deletion of a major viral surface protein, since surface proteins frequently are important antigens for neutralization and protection. Indeed, in the case of HRSV, the G protein is an important independent neutralization and protective antigen (9, 19, 25, 34). However, this does not appear to be the case for HMPV, based on the finding that intranasal immunization of hamsters with a recombinant human parainfluenza virus vector expressing the F protein induced a high level of HMPV-neutralizing serum antibodies and protective efficacy, whereas vectors expressing SH or G were not effective in inducing HMPV-neutralizing antibodies, and, at best, very weakly protective against challenge (23). Thus, the F protein appears to be the major HMPV neutralization and protective antigen, with SH and G playing minor or insignificant roles. While HMPV appears to exist in two genetic subgroups, immunization with vectored F protein of a single HMPV subgroup induced a high titer of neutralizing antibody and effective protection against both subgroups (17, 23, 24). This suggests that a single HMPV vaccine virus should be effective against both genetic subgroups. In summary, we have identified two promising vaccine candidates, ΔG and ΔM2-2, that are appropriate to be moved forward to clinical trials.
Acknowledgments
We thank Guy Boivin (Laval University, Quebec, Canada) and Teresa Peret, Dean Erdman, and Larry Anderson (Centers for Disease Control and Prevention, Atlanta, Georgia) for providing an initial inoculum of CAN97-83. We also thank Marisa St. Claire, William R. Elkins, Vanessa Davis, and Bradley Finneyfrock for excellent contributions to the primate study.
REFERENCES
- 1.Bastien, N., D. Ward, P. Van Caeseele, K. Brandt, S. H. Lee, G. McNabb, B. Klisko, E. Chan, and Y. Li. 2003. Human metapneumovirus infection in the Canadian population. J. Clin. Microbiol. 41:4642-4646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bermingham, A., and P. L. Collins. 1999. The M2-2 protein of human respiratory syncytial virus is a regulatory factor involved in the balance between RNA replication and transcription. Proc. Natl. Acad. Sci. USA 96:11259-11264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biacchesi, S., M. H. Skiadopoulos, G. Boivin, C. T. Hanson, B. R. Murphy, P. L. Collins, and U. J. Buchholz. 2003. Genetic diversity between human metapneumovirus subgroups. Virology 315:1-9. [DOI] [PubMed] [Google Scholar]
- 4.Biacchesi, S., M. H. Skiadopoulos, K. C. Tran, B. R. Murphy, P. L. Collins, and U. J. Buchholz. 2004. Recovery of human metapneumovirus from cDNA: optimization of growth in vitro and expression of additional genes. Virology 321:247-259. [DOI] [PubMed] [Google Scholar]
- 5.Biacchesi, S., M. H. Skiadopoulos, L. Yang, E. W. Lamirande, K. C. Tran, B. R. Murphy, P. L. Collins, and U. J. Buchholz. 2004. Recombinant human Metapneumovirus lacking the small hydrophobic SH and/or attachment G glycoprotein: deletion of G yields a promising vaccine candidate. J. Virol. 78:12877-12887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biacchesi, S., M. H. Skiadopoulos, L. Yang, B. R. Murphy, P. L. Collins, and U. J. Buchholz. 2005. Rapid human metapneumovirus microneutralization assay based on green fluorescent protein expression. J. Virol. Methods 128:192-197. [DOI] [PubMed] [Google Scholar]
- 7.Boivin, G., Y. Abed, G. Pelletier, L. Ruel, D. Moisan, S. Cote, T. C. Peret, D. D. Erdman, and L. J. Anderson. 2002. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J. Infect. Dis. 186:1330-1334. [DOI] [PubMed] [Google Scholar]
- 8.Buchholz, U. J., S. Biacchesi, Q. N. Pham, K. C. Tran, L. Yang, C. L. Luongo, M. H. Skiadopoulos, B. R. Murphy, and P. L. Collins. 2005. Deletion of M2 gene open reading frames 1 and 2 of human metapneumovirus: effects on RNA synthesis, attenuation, and immunogenicity. J. Virol. 79:6588-6597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connors, M., A. B. Kulkarni, P. L. Collins, C. Y. Firestone, K. L. Holmes, H. C. Morse III, and B. R. Murphy. 1992. Resistance to respiratory syncytial virus (RSV) challenge induced by infection with a vaccinia virus recombinant expressing the RSV M2 protein (Vac-M2) is mediated by CD8+ T cells, while that induced by Vac-F or Vac-G recombinants is mediated by antibodies. J. Virol. 66:1277-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crowe, J. E., Jr. 2004. Human metapneumovirus as a major cause of human respiratory tract disease. Pediatr. Infect. Dis. J. 23:S215-S221. [DOI] [PubMed] [Google Scholar]
- 11.Falsey, A. R., D. Erdman, L. J. Anderson, and E. E. Walsh. 2003. Human metapneumovirus infections in young and elderly adults. J. Infect. Dis. 187:785-790. [DOI] [PubMed] [Google Scholar]
- 12.Hamelin, M. E., Y. Abed, and G. Boivin. 2004. Human metapneumovirus: a new player among respiratory viruses. Clin. Infect. Dis. 38:983-990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karron, R. A., D. A. Buonagurio, A. G. Georgiu, S. S. Whitehead, J. E. Adamus, M. L. Clements-Mann, D. O. Harris, V. B. Randolph, S. A. Udem, B. R. Murphy, and M. S. Sidhu. 1997. Respiratory syncytial virus (RSV) SH and G proteins are not essential for viral replication in vitro: clinical evaluation and molecular characterisation of a cold-passaged, attenuated RSV subgroup B mutant. Proc. Natl. Acad. Sci. USA 94:13961-13966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karron, R. A., P. F. Wright, R. B. Belshe, B. Thumar, R. Casey, F. Newman, F. P. Polack, V. B. Randolph, A. Deatly, J. Hackell, W. Gruber, B. R. Murphy, and P. L. Collins. 2005. Identification of a recombinant live attenuated respiratory syncytial virus vaccine candidate that is highly attenuated in infants. J. Infect. Dis. 191:1093-1104. [DOI] [PubMed] [Google Scholar]
- 15.Konig, B., W. Konig, R. Arnold, H. Werchau, G. Ihorst, and J. Forster. 2004. Prospective study of human metapneumovirus infection in children less than 3 years of age. J. Clin. Microbiol. 42:4632-4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackie, P. L. 2003. The classification of viruses infecting the respiratory tract. Paediatr. Respir. Rev. 4:84-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacPhail, M., J. H. Schickli, R. S. Tang, J. Kaur, C. Robinson, R. A. Fouchier, A. D. Osterhaus, R. R. Spaete, and A. A. Haller. 2004. Identification of small-animal and primate models for evaluation of vaccine candidates for human metapneumovirus (hMPV) and implications for hMPV vaccine design. J. Gen. Virol. 85:1655-1663. [DOI] [PubMed] [Google Scholar]
- 18.McAdam, A. J., M. E. Hasenbein, H. A. Feldman, S. E. Cole, J. T. Offermann, A. M. Riley, and T. A. Lieu. 2004. Human metapneumovirus in children tested at a tertiary-care hospital. J. Infect. Dis. 190:20-26. [DOI] [PubMed] [Google Scholar]
- 19.Olmsted, R. A., N. Elango, G. A. Prince, B. R. Murphy, P. R. Johnson, B. Moss, R. M. Chanock, and P. L. Collins. 1986. Expression of the F glycoprotein of respiratory syncytial virus by a recombinant vaccinia virus: comparison of the individual contributions of the F and G glycoproteins to host immunity. Proc. Natl. Acad. Sci. USA 83:7462-7466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osterhaus, A., and R. Fouchier. 2003. Human metapneumovirus in the community. Lancet 361:890-891. [DOI] [PubMed] [Google Scholar]
- 21.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoint. Am. J. Hyg. 27:493-497. [Google Scholar]
- 22.Schmidt, U., J. Beyer, U. Polster, L. J. Gershwin, and U. J. Buchholz. 2002. Mucosal immunization with live recombinant bovine respiratory syncytial virus (BRSV) and recombinant BRSV lacking the envelope glycoprotein G protects against challenge with wild-type BRSV. J. Virol. 76:12355-12359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skiadopoulos, M. H., S. Biacchesi, U. J. Buchholz, E. Amaro-Carambot, S. R. Surman, P. L. Collins, and B. R. Murphy. Unpublished data. [DOI] [PubMed]
- 24.Skiadopoulos, M. H., S. Biacchesi, U. J. Buchholz, J. M. Riggs, S. R. Surman, E. Amaro-Carambot, J. M. McAuliffe, W. R. Elkins, M. St Claire, P. L. Collins, and B. R. Murphy. 2004. The two major human metapneumovirus genetic lineages are highly related antigenically, and the fusion (F) protein is a major contributor to this antigenic relatedness. J. Virol. 78:6927-6937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor, G., L. H. Thomas, J. M. Furze, R. S. Cook, S. G. Wyld, R. Lerch, R. Hardy, and G. W. Wertz. 1997. Recombinant vaccinia viruses expressing the F, G or N, but not the M2, protein of bovine respiratory syncytial virus (BRSV) induce resistance to BRSV challenge in the calf and protect against the development of pneumonic lesions. J. Gen. Virol. 78:3195-3206. [DOI] [PubMed] [Google Scholar]
- 26.Teng, M. N., and P. L. Collins. 2002. The central conserved cystine noose of the attachment G protein of human respiratory syncytial virus is not required for efficient viral infection in vitro or in vivo. J. Virol. 76:6164-6171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teng, M. N., S. S. Whitehead, and P. L. Collins. 2001. Contribution of the respiratory syncytial virus G glycoprotein and its secreted and membrane-bound forms to virus replication in vitro and in vivo. Virology 289:283-296. [DOI] [PubMed] [Google Scholar]
- 28.van den Hoogen, B. G., T. M. Bestebroer, A. D. Osterhaus, and R. A. Fouchier. 2002. Analysis of the genomic sequence of a human metapneumovirus. Virology 295:119-132. [DOI] [PubMed] [Google Scholar]
- 29.van den Hoogen, B. G., J. C. de Jong, J. Groen, T. Kuiken, R. de Groot, R. A. Fouchier, and A. D. Osterhaus. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat. Med. 7:719-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van den Hoogen, B. G., D. M. Osterhaus, and R. A. Fouchier. 2004. Clinical impact and diagnosis of human metapneumovirus infection. Pediatr. Infect. Dis. J. 23:S25-32. [DOI] [PubMed] [Google Scholar]
- 31.Viazov, S., F. Ratjen, R. Scheidhauer, M. Fiedler, and M. Roggendorf. 2003. High prevalence of human metapneumovirus infection in young children and genetic heterogeneity of the viral isolates. J. Clin. Microbiol. 41:3043-3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitehead, S. S., A. Bukreyev, M. N. Teng, C. Y. Firestone, M. St Claire, W. R. Elkins, P. L. Collins, and B. R. Murphy. 1999. Recombinant respiratory syncytial virus bearing a deletion of either the NS2 or SH gene is attenuated in chimpanzees. J. Virol. 73:3438-3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams, J. V., P. A. Harris, S. J. Tollefson, L. L. Halburnt-Rush, J. M. Pingsterhaus, K. M. Edwards, P. F. Wright, and J. E. Crowe, Jr. 2004. Hum. metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N. Engl. J. Med. 350:443-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright, P. F., R. A. Karron, R. B. Belshe, J. Thompson, J. E. Crowe, Jr., T. G. Boyce, L. L. Halburnt, G. W. Reed, S. S. Whitehead, E. L. Anderson, A. E. Wittek, R. Casey, M. Eichelberger, B. Thumar, V. B. Randolph, S. A. Udem, R. M. Chanock, and B. R. Murphy. 2000. Evaluation of a live, cold-passaged, temperature-sensitive, respiratory syncytial virus vaccine candidate in infancy. J. Infect. Dis. 182:1331-1342. [DOI] [PubMed] [Google Scholar]