Abstract
This study examines the factors influencing the quality of operating theatres in Indian multispeciality hospitals, focusing on key managerial and infrastructural components. The study investigates the influence of automated doors and scrub stations, HEPA filters, medical waste management, operating theatre management, pathology services in the operating theatre, and unidirectional workflow on the quality of the operating theatre, as well as the moderating role of operating theatre management between medical waste management and the quality of the operating theatre. This study employed the Donabedian quality of care framework, combined with partial least squares structural equation modeling (PLS-SEM), to analyze data from 483 respondents, including theatre staff, nurses, and surgeons. The findings reveal that all factors significantly influence the quality of operating theatres, with operating theatre management having the strongest effect. This study offers critical insights for healthcare policymakers and hospital administrators seeking to optimize workflow and surgical infrastructure. Therefore, this study contributes to the growing literature on the quality of surgical environments in emerging economies.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-025-13202-w.
Keywords: Quality operating theatre, Medical waste management, Donabedian quality of care framework, Healthcare infrastructure, Surgical safety
Introduction
In recent times, the reputation of multispecialty hospitals has depended on the performance of the operating theatre and its quality, which is in line with the quality of care. At the same time, the quality operating theatre serves as a critical environment for efficiency, coverage, precision, and patient safety [1]. Due to the evolving demand in healthcare, continuous improvement in operating theatre management and infrastructure is essential [2]. Furthermore, to meet the changing expectations of patients, technological advancements become inevitable for fulfilling adaptive, reliable, and sophisticated operating theatre environments [3]. Moreover, excellence, patient health outcomes, high standards, and the quality of operating theatre play crucial roles that substantially contribute to hospital revenue [4]. Thus, this study aims to identify the factors (automated doors and scrub stations, HEPA filters, medical waste management, operating theatre management, pathology services in the operating theatre, and unidirectional workflow) that influence the quality of the operating theatre.
The quality of the operating theatre, management system, and innovative design elements enhances the operating theatre efficiency, which includes automated doors and scrub stations, HEPA filters, and advanced waste management to minimize contamination risks and promote seamless surgical workflows [5–7]. At the same time, operating theatre management aligns with the integration of pathology services to support timely diagnostics, optimize resource utilization, and improve patient outcomes [8–11]. Additionally, in terms of quality, operating theatres adhere to universal infection control protocols, maintain sterile environments, and minimize cross-contamination [12–14]. Hence, this study elucidates the mediating role of operating theatre management in the relationship between medical waste management and the quality of the operating theatre.
Additionally, the Donabedian quality of care framework [15] focuses on structure, process, and outcome in healthcare quality assessment, which explores the key managerial and infrastructural components that impact the quality of operating theatre [16]. Therefore, based on the Donabedian quality of care framework, this study focused on the factors that influence the quality of the operating theatre on key components. Furthermore, operating theatre management serves as a moderator between medical waste management and the quality of the operating theatre, highlighting the role of managerial effectiveness in enhancing the relationship between medical waste management practices and the overall performance of the operating theatre in terms of quality care.
Although studies related to the private healthcare sector in India exist, research on the quality of operating theatres remains fragmented, and limited studies have explored the collective influence of quality factors on the quality of operating theatres. There are prior studies primarily focused on specific elements like automated hygiene doors reducing contamination risks [17], HEPA filters lowering infection rates [18], recycling programs reducing health risks [19], real-time data trancing on resource allocation [20], frozen section biopsies aiding surgical decisions [21], minimizing contamination risks through workflows [22], and reducing waste through operating theatre management [23]. Also, there are region-specific challenges, including evolving healthcare expectations, staffing constraints, and high patient load. Therefore, this study provides a comprehensive examination of the role that infrastructural and managerial components play in influencing the quality of operating theatre.
The study aims to investigate the combined factors of quality operating theatre on critical healthcare outcomes, focusing on key components related to operational efficiency, infection control, and patient safety. Also, the research approach assesses the collective impact rather than isolated influences. Moreover, the study offers valuable insights for hospital administrators and policymakers to improve standards in line with India’s healthcare objectives and international benchmarks. Additionally, this study bridges the existing research gap and provides strategic guidance for optimizing statistical environments to achieve better patient outcomes and improved institutional performance.
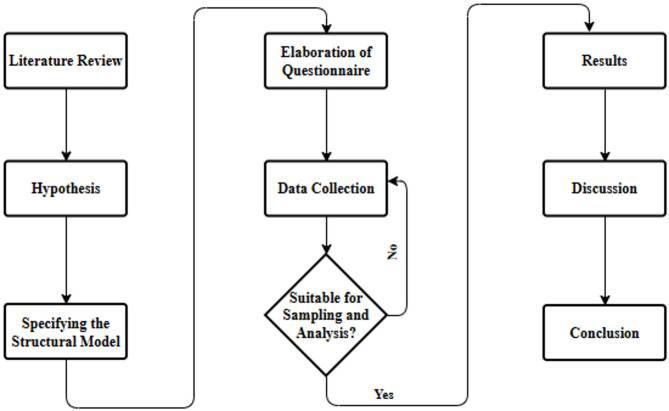
Figure 1 outlines the methodology steps used in the structured research process for empirical studies. First, a literature review will be conducted to identify the research gap. Second, it leads to the development of hypotheses based on theoretical insights. Third, specifying the structural mode to illustrate hypothesized relationships. Fourth, a questionnaire. Fifth is data collection. Sixth, the decision point to assess whether data is suitable for analysis; it does not loop back for further data collection. If yes, the sixth results are analyzed. Seventh, a discussion to interpret findings. Finally, the conclusion summarizes key insights, implications, limitations, and suggestions for future research.
Fig. 1.
The methodology steps.
Source: Developed by the author
Theoretical background and hypothesis development
Donabedian quality of care framework
In healthcare facilities, the quality of the operating theatre is a crucial determinant in infection control, patient safety, and surgical efficiency. Therefore, this study employed the Donabedian quality of care framework [15] to provide the theoretical foundation for examining the influence of managerial and structural components on quality in operating theatres. Also, the Donabedian quality of care framework categorizes healthcare quality into structure, process, and outcome, where the management and infrastructure play vital roles in operating theatre efficiency and optimal patient care. Additionally, based on the Donabedian quality of care framework this study categorizes the influencing factors like; automated doors, scrub stations, and HEPA filters are considered as structure, medical waste management, pathology services in the operating theatre and unidirectional workflow are regarded as process, and quality of operating theatre is the targeted outcome. There are several studies based on the Donabedian quality of care framework were used to evaluate healthcare quality in the educational sector (nursing education) [24], neonatal and maternal health [25], integrated chronic disease management [26], acute care surgery, emergency general surgery, and hospital quality assessment [16], primary healthcare quality [27], patient safety protocol adherence [28], and maternal and perinatal care in obstetric triage in lower-middle countries [29]. Thus, the Donabedian quality of care framework has proven effective in assessing the quality of operating theatres, which is the basis for total quality management [30]. Therefore, the Donabedian quality of care framework is applied to measure the factors influencing the quality of operating theatres in private multispecialty hospitals in India. Moreover, this study offers new insights by focusing on the specific sector that explores previously underexamined interactions within the Donabedian quality of care framework, presenting a fresh perspective on the applicability of the model. Additionally, this study extends empirical understanding by introducing novel contexts and variables that were not fully explored in prior studies. Hence, this study addresses gaps in the literature and provides a detailed examination of factors in the quality of operating theatre for both theoretical advancement and practical application.
Automated doors and scrub stations
Automated doors are motion sensor-based entry systems that automatically open and close the door when a person approaches or leaves. Scrub stations are specialized cleaning areas designed for thorough decontamination to ensure strict hygiene and safety in sterile environments [31]. According to a study by Glowicz et al., the integration of automated hygiene doors and well-designed scrub stations is crucial for reducing the risk of contamination [17]. In addition, Reddy et al. stated that automated doors not only minimize physical contact, thereby enhancing safety, but also improve operational efficiency and user convenience [32]. Moreover, Gould et al. indicated that scrub stations designed with features such as hands-free operation and proper materials have been shown to improve compliance with hand hygiene protocols, a critical factor in preventing surgical site infections [33]. Furthermore, Lansing et al. highlighted the influence of airborne bacterial load and surface contamination in the operating theatre [34]. Notably, Camera et al. mentioned that door opening affects contamination, a crucial factor in the quality of operating theatres and infection control [35]. Empirical studies consistently highlight the connection between automated doors and scrub stations and the quality of operating theatres. Given that it represents the combined role of preventing contamination, reducing contact, and enhancing hygiene, it is rational to expect that this technology will significantly affect the quality of the operating theatre. Thus, the following hypothesis was developed.
H1:
Automated doors and scrub stations significantly influence the quality of the operating theatre.
HEPA filters
Air quality management is crucial in operating theatres, with high-efficiency particulate air (HEPA) filters playing a central role in pathogen control [6]. As highlighted by Li et al., the reduction of airborne contaminants by HEPA filters will lower infection rates in the operating theatre [18]. Likewise, Lans et al. noted that HEPA filtration is a crucial factor in ensuring quality air and infection control, thereby improving the quality of operating theatres [36]. Similarly, Soleha et al. demonstrated that HEPA filters are related to the quality of operating theatres and have a positive impact on key metrics, such as air cleanliness and reduced infection control [37]. Additionally, Ereth et al. found that air purification technologies, such as HEPA filters, improve the air quality of operating theatres [38]. Correspondingly, Spagnolo et al. noted that HEPA filters align with guidelines for preventing surgical site infections as a critical component of high-quality operating theatres and controlling the risk of infections [5]. Additionally, Sadrizadeh et al. suggested that the ventilation system and air quality are closely linked to infection control in the operating theatre [39]. Empirical studies consistently highlight the connection between HEPA filters and the quality of operating theatres, which reduces the risk of infection and improves air quality. Hence, the following hypothesis was developed.
H2:
HEPA filters significantly influence the quality of operating theatre.
Medical waste management
Medical waste management is a priority in a safe operating theatre environment. Effective medical waste management, which involves adequately identifying, segregating, and treating waste scientifically, reduces contamination and environmental risks [40]. According to a study by Ramos et al., a significant portion of medical-related waste is produced within operating theatres, highlighting the critical need for comprehensive waste segregation and sterilization [41]. In addition, Moya et al. explained that recycling programs for operating theatre waste are integral to medical waste management, aiming to reduce health risks and enhance sustainability [19]. Moreover, Ong et al. confirmed the importance of segregation and recycling the waste produced in operating theatres to minimize both environmental and financial implications [42]. Further, Selvy et al. proposed actionable recommendations to reduce the environmental impact of the operating theatre, focusing on the use of anesthetic agents, energy consumption, and waste management, thereby improving the overall quality of the operating theatre [43]. Notably, Lorenzon et al. emphasized the need for strategies to reduce operating theatre waste, thereby enhancing efficiency and sustainability in surgical environments [44]. Empirical studies consistently highlight the connection between medical waste management and the quality of operating theatres, which is essential for safety, sustainability, and infection prevention. Therefore, the following hypothesis was developed.
H3:
Medical waste management significantly influences the quality of operating theatre.
Operating theatre management
Resource allocation and surgical workflows can be improved through operating theatre management across hospital settings [7]. According to Agnoletti et al., real-time data tracking in the operating theatre enhances team communication, reduces delays, and improves resource allocation [20]. In addition, Morri et al. demonstrated that operating theatre management in terms of care pathways and healthcare staff is linked to the overall quality and performance of the operating theatre [45]. Moreover, Slim et al. found that intraoperative processes, such as anesthesia and medical devices, improve the eco-responsibilities that enhance the quality of the operating theatre [46]. Furthermore, Huang et al. shared that in-office laryngology procedure clinics enhance economic, organizational, and clinical outcomes in terms of the quality of operating theatres [47]. Additionally, Saleem et al. suggested that surgeon-led trauma beds in recovery improve daily case volumes and theatre start times, thereby enhancing the quality of operating theatre management [48]. Empirical studies consistently highlight the connection between operating theatre management and quality operating theatre, focusing on resource utilization and workflow efficiency. Thus, the following hypothesis was developed.
H4:
Operating theatre management significantly influences the quality of operating theatre.
Pathology service in the operating theatre
In-operating theatre pathology services enable immediate tissue analysis, providing real-time diagnostic support during surgery for timely surgical decisions [49]. According to a study by Jaafar, internal pathology services through frozen section biopsies enable surgeons to make necessary decisions during surgical procedures [21]. Likewise, Iwasaki et al. indicated that pathology is necessary for skilled pathologists to enhance surgical decision-making and minimize delays [50]. Similarly, Start et al. highlighted the efficiency of pathology services, including timely specimen transport and proper fixation practices, which influence the output of operating theatres [51]. Additionally, D’Angelo and Mejabi found that improving pathology services in workflow efficiency and specimen sampling enhances the overall safety and quality of operating theatre outcomes [52]. Correspondingly, Vladu et al. highlighted the role of the pathology service in enhancing the quality of the operating theatre through collaboration with the surgical team and intraoperative involvement [7]. Empirical studies consistently highlight the connection between pathology services in the operating theatre and the quality of the operating theatre, which supports accurate and timely decision-making. Hence, the following hypothesis was developed.
H5:
Pathology service in the operating theatre significantly influences the quality of the operating theatre.
Unidirectional workflows
To minimize contamination risks, a unidirectional workflow during surgeries is implemented by ensuring that materials and healthcare staff move exclusively from clean areas to higher-risk zones, thereby reducing the risk of cross-contamination [53]. According to Fan et al., a unidirectional workflow is a successful method for infection prevention in surgeries and efficient operating theatres [22]. Notably, Whyte et al. and Bhaskar established that a unidirectional workflow achieves consistency, performance, and design, and enhances the quality of the operating theatre [54, 55]. Likewise, Andersson et al. explained that its unidirectional workflow improves the safety of the operating theatre and represents the quality and effectiveness of the operating theatre [56]. Similarly, Leber confirmed that unidirectional workflow ensures high-quality results and minimizes contamination risks by maintaining sterility and improving operation effectiveness [57]. Additionally, McElroy et al. proposed that leadership, teamwork, and safety in the operating room will reduce errors and improve patient safety [58]. Empirical studies consistently highlight the connection between unidirectional workflow and quality operating theatre, which enhances efficiency and reduces contamination. Therefore, the following hypothesis was developed.
H6:
Unidirectional workflow significantly influences the quality of operating theatre.
The moderating role of operating theatre management
According to Talbot and Moore, medical waste in operating theatres has an environmental impact, highlighting the need for improved waste segregation, proper staff education, and clear guidelines on waste disposal through operating theatre management, which can lead to ecological benefits and cost savings for high-quality operating theatres [23]. According to Warda, revising single-use surgical packs will reduce hospital costs and waste in the operating theatre, highlighting the effectiveness of simple and sustainable practices in improving both financial and environmental factors within the operating theatre [59]. Correspondingly, Magasich-Airola et al. emphasized that operating theatre management can reduce hospital waste and greenhouse gas emissions, which supports the sustainable goals of medical waste management and improves the quality of the operating theatre [60]. Additionally, a study by Kaposi et al. noted that effective operating theatre management practices can reduce hazardous waste generation through proper medical waste management, thereby improving the quality of the operating theatre [61]. Empirical studies consistently highlight the connection between operating theatre management, medical waste management, and the quality of the operating theatre, which is essential for safety and sustainability. Thus, the following hypothesis was developed.
H7:
Operating theatre management moderates between medical waste management and quality operating theatre.
The existing literature has examined various factors independently, and most of it remains fragmented, focusing on single components in isolation. There are only a few studies that have combined both structural and process-level factors within a unified quality framework, as in the Donabedian quality of care framework, which is structured as a model of structure, process, and outcome. Moreover, the moderating role of operating theatre management in enhancing specific quality relationships between medical waste management and quality operating theatre has not been sufficiently explored. Therefore, this study fills the gaps by offering a comprehensive, theory-driven model that links multiple factors influencing quality in operating theatres, contributing both theoretically and practically.
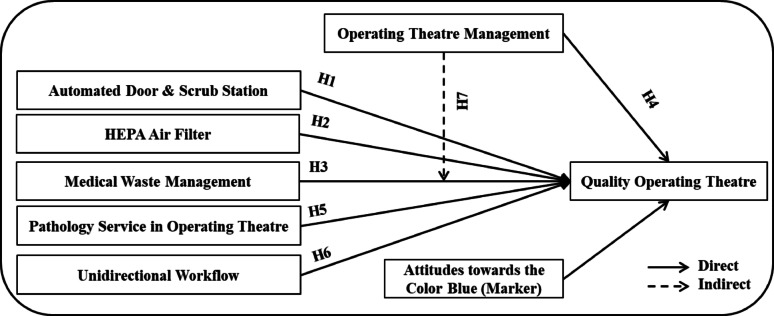
Figure 2’s conceptual (structural) model represents the direct connection between independent (automated doors, scrub station, HEPA filters, medical waste management, operating theatre management, pathology service in the operating theatre, and unidirectional workflow) and dependent (quality of the operating theatre) variables. Next, the indirect connection between operating theatre management (moderator) and medical waste management leads to quality operating theatres. Moreover, attitudes towards the color blue as a marker variable reduce measurement error and improve model validity.
Fig. 2.
Conceptual Model.
Source: Developed by the authors based on the literature.
Methodology
Area of study
According to NABH, licensed medical facilities in India are classified into private, government, and public-private partnership hospitals [62]. Additionally, private hospitals were further classified into multispecialty, super specialty, tertiary specialty, and quaternary specialty categories based on the services provided [63]. This study selected only multispecialty hospitals for data collection. At the same time, in terms of the study area, this study utilized the top 7 medical destinations in India, namely Bengaluru, Chennai, Delhi, Hyderabad, Mumbai, Kerala, and Kolkata, as per Ghosh [64]. Further, the multispeciality hospitals in these destinations are equipped with highly trained professionals and advanced medical technology to ensure comprehensive patient care [65]. Moreover, this study identified 14 multispecialty hospitals (the top 2 hospitals from the top 7 medical destinations) in India [62]. Consequently, this study focused on automated doors and scrub stations, HEPA filters, medical waste management, operating theatre management, pathology services in the operating theatre, unidirectional workflow, and quality assurance in the operating theatre in this context.
Measurement
This study used a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree) [66]. According to Hair et al., the measurement model in PLS can be reflective or formative [67]. However, this study employed the reflective model to verify whether the model explains the phenomenon by observing the constructs that influence their indicators. In contrast, formative models aim to adjust a target construct through factor relationships, using indicators as drivers.
Table 1 represents the constructs (automated doors and scrub station, HEPA filters, medical waste management, pathology service in the operating theatre, and unidirectional workflow), which contain three indicators, each serving as an exogenous variable. The constructs (pathology service in the operating theatre and quality of the operating theatre) comprise three indicators, each serving as an endogenous variable. Additionally, the attitude towards the color blue contains four indicators as marker variables, which are used to detect or control for common method bias and serve as a control variable. (Appendix).
Table 1.
Constructs and indicators in the model
| Construct | Position | Indicators | References |
|---|---|---|---|
| Automated doors and scrub station | Exogenous | ADSS1-ADSS3 | (Dickey et al., 2015) |
| HEPA filters | Exogenous | HEPA1-HEPA3 | (Dickey et al., 2015) |
| Medical waste management | Exogenous | MWMS1-MWMS3 | (Chartier et al., 2001) |
| Operating theatre management | Endogenous | OTMS1-OTMS3 | (Schouten et al., 2023) |
| Pathology service in operating theatre | Exogenous | PSOT1-PSOT3 | (Dere, 2017) |
| Unidirectional workflow | Exogenous | UDWF1-UDWF3 | (Smith et al., 2015) |
| Quality operating theatre | Endogenous | QUOT1-QUOT3 | (Vinayakumar & John, 2020) |
| Attitude towards color blue | Marker | MAR1-MAR4 | (Miller, 2013) |
Source: Developed by the authors based on the literature
Sampling and data collection
This study focused on surgeons, scrub nurses or operating room nurses, anaesthesiologists or anesthesia providers, pathologists, operating theatre managers or coordinators, and others directly involved in operating theatre activities. There are 14 private multispecialty hospitals from the top seven selected destinations, with approximately 2,598 employees working in this category [68]. Using the G*Power calculator [69] for an F test in linear multiple regression (fixed mode R² deviation from zero), with an effect size f2 of 0.15, an alpha of 0.05, a power of 0.95, and 6 predictors, the required sample size is 146. When adding the marker variable, the required sample size is 153. However, the plan to collect the data involves obtaining at least 500 responses from 14 private multispecialty hospitals across the top seven selected destinations in India. Finally, 483 responses were collected, with no missing data, which exceeds the minimum sample size required to analyze the conceptual model.
In addition, this study utilized a quantitative research approach with a random sampling procedure using a cross-sectional study design to collect data from respondents. Furthermore, the data were collected through an online survey using a structured questionnaire in English, distributed via email, and managed by the researchers, who coordinated directly with the respondents to ensure informed consent and confidentiality for a period of six months from May 2024 to October 2024. During data collection, no significant language-related concerns were reported. As the study used an online survey, measures such as email verification and duplication checks were employed to ensure the accuracy and authenticity of participant responses.
Methods
Partial least squares structural equation modeling (PLS-SEM) is the analytical technique used in this study. According to Sarstedt et al., PLS-SEM is a causal-predictive approach to structural equation modeling (SEM) that prioritizes prediction while estimating statistical models [70]. Moreover, PLS-SEM demonstrated a greater predictive power than covariance-based structural equation modelling (CB-SEM) [70]. Further, the key advantages of using PLS-SEM include higher item loadings, superior composite reliability (CR) value indicating better construct reliability and validity, and excellent outcomes through composite-based models [71]. Additionally, this study employed PLS-SEM due to the inclusion of mediation effects and the model’s complexity. In the first stage, the measurement model’s initial data validation is done with reliability markers, internal consistency, convergent validity, and discriminant validity using SmartPLS 4, and in the second stage, correlation, regression, and ANOVA using SPSS 27 and in the third stage hypothesis tested using the structural model using SmartPLS 4 through the bootstrap technique (10,000 iterations) has subsequently applied to evaluate the significance of correlations after confirming model reliability.
Ethical statement
This study was conducted in full compliance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Research Center at the University of Technology, Bahrain (Approval No. UTB2024CAFSEC020, dated 1 December 2024). The research also adhered to the ethical guidelines outlined in the IRB-HSBS informed consent policy of the University of Technology, Bahrain. Moreover, the data were collected solely from the employees working in the hospitals using a non-interventional, survey-based approach, with no involvement of patient data or clinical procedures. At the same time, the study adhered to the Indian Council of Medical Research (ICMR) ethical guidelines [72] and international ethical standards, including the World Medical Association’s Declaration of Helsinki [73].
Informed consent
This study employed a written informed consent form, included at the beginning of the questionnaire, which all participants signed (Appendix). Participants were exclusively the surgeons, scrub nurses or operating room nurses, anaesthesiologists or anesthesia providers, pathologists, operating theatre managers or coordinators, and others directly connected to the operating theatre activities from 14 private multispeciality hospitals in India. Before participating, each individual received a comprehensive information sheet detailing the research purpose and methods. Participation was entirely voluntary, and individuals were asked to complete the questionnaire only after carefully reviewing the information sheet and addressing any questions or concerns they may have had. This process ensured informed consent, guaranteeing that all participants fully understood the study’s objectives and their voluntary contribution to the research.
Data analysis
PLS modelling was employed in this study by using SmartPLS4 [74] to analyze both the measurement and structural model. In addition, PLS has the advantage of not requiring normality assumptions, which makes it ideal for survey data that is non-normally distributed [75]. Moreover, the cross-sectional data collected from respondents is single-source data; there is a chance of common method bias as a potential issue [76]. Also, the study utilized full collinearity by regressing all variables against a common variable [77].
Table 2 represents all the VIF values that are less than 3.3; therefore, it satisfies the rule of thumb that VIF ≤ 3.3 [78], indicating that single-source bias is not a significant concern for the data. Additionally, using the attitude towards the color blue [79] as a marker, the difference in R² between the baseline method (0.580) and the method factor model (0.579) indicates a minor difference, suggesting no method bias and confirming data validity.
Table 2.
Full collinearity testing
| Construct | ADSS | HEPA | MEWM | OPTM | PSOT | QUOT | UDWF |
|---|---|---|---|---|---|---|---|
| VIF | 1.878 | 1.987 | 2.234 | 2.158 | 2.233 | 1.822 | 1.930 |
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality operating theatre; UDWF, Unidirectional workflow
Measurement model
As mentioned by Anderson and Gerbing (1988), this study used a two-step approach to test the development model [80]. In step one, the measurement model is used to assess the instrument’s validity and reliability [81, 82]. Furthermore, the measurement model requires that loadings must be ≥ 0.50, the average variance extracted (AVE) must be ≥ 0.50, and composite reliability (CR) must be ≥ 0.70 [81].
Table 3 indicates that loading greater than 0.50 ranges between (0.902 − 0.716), AVE greater than 0.50 ranges between (0.785 − 0.565), and CR greater than 0.70 ranges between (0.916 − 0.886). Next, to assess discriminant validity, the heterotrait-monotrait ratio of correlation (HTMT) criterion was used [83, 84], with a value of ≤ 0.90.
Table 3.
Measurement model for the constructs
| Constructs | Items | Loading | AVE | CR |
|---|---|---|---|---|
| Automated doors and scrub station | ADSS1 | 0.860 | 0.741 | 0.895 |
| ADSS2 | 0.859 | |||
| ADSS3 | 0.862 | |||
| HEPA filters | HEPA1 | 0.893 | 0.754 | 0.902 |
| HEPA2 | 0.840 | |||
| HEPA3 | 0.872 | |||
| Medical waste management | MEWM1 | 0.870 | 0.785 | 0.916 |
| MEWM2 | 0.887 | |||
| MEWM3 | 0.900 | |||
| Operating theatre management | OPTM1 | 0.852 | 0.774 | 0.911 |
| OPTM2 | 0.899 | |||
| OPTM3 | 0.888 | |||
| Pathology service in operating theatre | PSOT1 | 0.902 | 0.782 | 0.915 |
| PSOT2 | 0.881 | |||
| PSOT3 | 0.870 | |||
| Quality of operating theatre | QUOT1 | 0.754 | 0.565 | 0.886 |
| QUOT2 | 0.770 | |||
| QUOT3 | 0.796 | |||
| QUOT4 | 0.717 | |||
| QUOT5 | 0.716 | |||
| QUOT6 | 0.754 | |||
| Unidirectional workflow | UDWF1 | 0.866 | 0.747 | 0.899 |
| UDWF2 | 0.865 | |||
| UDWF3 | 0.862 |
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
Table 4 represents all the HTMT values that are less than 0.90, indicating that the respondents understood the difference between the constructs. Therefore, considering the measurement model for the constructs and the discriminant validity (HTMT) tests, it is evident that the measurement items are valid and reliable.
Table 4.
Discriminant validity (HTMT)
| Constructs | ADSS | HEPA | MEWM | OPTM | PSOT | QUOT | UDWF |
|---|---|---|---|---|---|---|---|
| ADSS | |||||||
| HEPA | 0.894 | ||||||
| MEWM | 0.830 | 0.878 | |||||
| OPTM | 0.830 | 0.896 | 0.881 | ||||
| PSOT | 0.813 | 0.874 | 0.841 | 0.824 | |||
| QUOT | 0.736 | 0.757 | 0.747 | 0.765 | 0.729 | ||
| UDWF | 0.836 | 0.827 | 0.850 | 0.868 | 0.893 | 0.811 |
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
Inferential statistical analysis
Correlation analysis was used to measure the direction and strength of the linear relationship between the variables [85]. Additionally, it facilitates the identification of a relationship that guides further analysis without implying causation [86]. Moreover, this technique is crucial for examining data relationships and detecting multicollinearity prior to advanced modeling [87].
Table 5 revealed that all the variables (automated doors and scrub station, HEPA filters, medical waste management, operating theatre management, pathology service in operating theatre, and unidirectional workflow) have a strong and highly significant positive relationship with the correlation coefficient ranging from 0.61 to 0.88 with each other and with the quality operating theatre. Thus, any improvements in these factors are strongly associated with enhancing the quality of the operating theatre, and a statistically significant relationship at the 0.01 level confirms that the relationship is highly reliable.
Table 5.
Correlation analysis
| Variables | Correlation | P-value | Interpretation |
|---|---|---|---|
| ADSS | 0.61 - 0.82 | p < 0.01** | Highly Significant and Strong positive correlations |
| HEPA | 0.64 - 0.84 | p < 0.01** | Highly Significant and Strong positive correlations |
| MEWM | 0.64 - 0.84 | p < 0.01** | Highly Significant and Strong positive correlations |
| OPTM | 0.65 - 0.88 | p < 0.01** | Highly Significant and Strong positive correlations |
| PSOT | 0.63 - 0.88 | p < 0.01** | Highly Significant and Strong positive correlations |
| UDWF | 0.69 - 0.85 | p < 0.01** | Highly Significant and Strong positive correlations |
| QUOT | 0.61 - 0.69 | p < 0.01** | Highly Significant and Strong positive correlations |
**. Correlation is significant at the 0.01 level (2-tailed)
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
Regression analysis was employed to investigate the relationship between various independent variables and the dependent variables, aiming to predict the outcomes [85]. Furthermore, it helps in determining the significance and strength of the predictors while controlling for other factors, and it’s a widely used method to test the model’s causal relationship in research [87].
Table 6 illustrates that the predictors of automated doors and scrub stations, HEPA filters, medical waste management, operating theatre management, pathology service in the operating theatre, and unidirectional workflow are significant positive predictors of the quality of operating theatre. At the same time, the unidirectional workflow shows the strongest predictor (β = 0.278, t = 6.178), and operating theatre management (β = 0.128, t = 4.267) indicates its critical role in ensuring quality operating theatres.
Table 6.
Regression analysis
| Description | Std. Beta | t-value | p-value | Interpretation |
|---|---|---|---|---|
| (Constant) | 18.339 | p < 0.01 | The regression model is significant overall. | |
| ADSS | 0.070 | 3.500 | 0.001 | Positive and significant predictor |
| HEPA | 0.119 | 3.967 | p < 0.01 | Positive and significant predictor |
| MEWM | 0.090 | 3.600 | p < 0.01 | Positive and significant predictor |
| OPTM | 0.128 | 4.267 | p < 0.01 | Positive and significant predictor |
| PSOT | 0.081 | 3.682 | p < 0.01 | Positive and significant predictor |
| UDWF | 0.278 | 6.178 | p < 0.01 | Strongest positive and significant predictor |
a. Dependent Variable: QUOT
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality operating theatre; UDWF, Unidirectional workflow
To determine if a significant difference exists, ANOVA is used to compare the means across multiple groups [86]. Additionally, ANOVA facilitates testing the hypothesis about the group effect on dependent variables while controlling for within-group variation [88].
Table 7 shows that the overall regression model is statistically significant, with an F value of 109.56 and a p-value of less than 0.001, confirming that the combination of six predictors significantly explains the variation in the quality of the operating theatre. Additionally, the model accounts for 58% of the total variance in the quality of the operating theatre, demonstrating strong explanatory power. Thus, the six predictors collectively provide a robust framework for improving and understanding the quality of the operating theatre, with only 42% of the variance attributed to other external factors.
Table 7.
ANOVA
| Source | Sum of Squares | Df | Mean Squre | F | Sig. |
|---|---|---|---|---|---|
| Regression | 58.00 | 6 | 9.667 | 109.56 | p < 0.01 |
| Residual/Error | 42.00 | 476 | 0.08824 | ||
| Total | 100.00 | 482 |
a. Dependent Variable: QUOT
b. Predictors: (Constant), UDWF, HEPA, ADSS, MEWM, PSOT, OPTM
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
Structural model
In testing the structural model, with univariate skewness and kurtosis within the base value of -1 to + 1, Mardia’s multivariate skewness (p < 0.05) and Mardia’s multivariate kurtosis (p < 0.05) show the significance [75, 89].
Figure 3 shows the path coefficients of the factors: Automated doors and scrub station, HEPA filters, Medical waste management, Operating theatre management, Pathology service in the operating theatre, and Unidirectional workflow. The R-squared value for a quality operating theatre is 0.580, which explains a moderate amount of variance with 58% predictability.
Fig. 3.
Path coefficient.
Source: Developed by authors based on the data analysis. Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
Table 8 presents the hypothesis testing of the direct effect between the independent and dependent variables. The results reveal that automated doors and scrub stations (β = 0.211, p < 0.001), HEPA filters (β = 0.127, p < 0.001), medical waste management (β = 0.203, p = 0.024), operating theatre management (β = 0.309, p = 0.011), pathology services in operating theatre (β = 0.109, p < 0.001), and unidirectional workflow (β = 0.346, p < 0.001) are significant which gives support to all H1, H2, H3, H4, H5, and H6. Moreover, all the independent variables have a significant influence on the quality of operating theatre. Furthermore, the beta values of the unidirectional workflow (0.346) have the strongest influence, followed by operating theatre management (0.309), which has a substantial positive influence. Automated doors and scrub stations (0.211) and medical waste management (0.203) have a moderate influence. HEPA filters (0.127) and pathology service in the operating theatre (0.109) have the weakest influence on the quality of the operating theatre. Thus, all the factors significantly influence the quality of the operating theatre, but the degree of influence varies.
Table 8.
Hypothesis testing direct effect
| Relationship | Std. Beta | Std. Error | t-values | p-values |
|---|---|---|---|---|
| ADSS → QUOT | 0.211 | 0.050 | 4.194 | P < 0.001 |
| HEPA → QUOT | 0.127 | 0.036 | 3.520 | P < 0.001 |
| MEWM → QUOT | 0.203 | 0.090 | 2.256 | 0.024 |
| OPTM → QUOT | 0.309 | 0.121 | 2.557 | 0.011 |
| PSOT → QUOT | 0.109 | 0.035 | 3.089 | P < 0.001 |
| UDWF → QUOT | 0.346 | 0.097 | 3.553 | P < 0.001 |
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
Table 9 presents the hypothesis testing of the indirect effect through bootstrapping [90, 91] of operating theatre management on medical waste management and quality operating theatre (β = 0.211, p < 0.001), which is significant, providing support for H7. Moreover, the significant moderating effect confirms that operating theatre management plays a crucial role in enhancing the impact of medical waste management on the quality of the operating theatre. Hence, when operating theatre management is well-organized, then effective medical waste management has a more significant influence on the quality of operating theatre.
Table 9.
Hypothesis testing indirect effect
| Relationship | Std. Beta | Std. Error | t-values | p-values |
|---|---|---|---|---|
| OPTM x MEWM → QUOT | 0.211 | 0.044 | 4.794 | P < 0.001 |
Source: Developed by the authors based on the data analysis
Note: ADSS, Automated doors and scrub station; HEPA, HEPA filters; MEWM, Medical waste management; OPTM, Operating theatre management; PSOT, Pathology service in operating theatre; QUOT, Quality of operating theatre; UDWF, Unidirectional workflow
PLSpredict
To assess the predictive relevance, this study used PLSpredict with a 10-fold procedure as proposed by Shmueli et al. [92]. Also, it is a holdout sample-based procedure that makes case-level predictions at either the item or construct level.
Table 10 highlights that the Q²predict values (0.206 to 0.352) are greater than 0, indicating that the PLS model has predictive relevance for all indicators. Additionally, PLS_RMSE is lower than LM_RMSE for all items. Furthermore, for PLS-LM_RMSE, all values are negative, indicating that PLS outperforms LM. Similarly, for PLS-IA_RMSE, all values are negative, indicating that PLS predictions are better than the in-sample average. Therefore, the results confirm that the PLS model is a reliable predictive tool for the dataset.
Table 10.
PLSpredict
| MV | Q²predict | PLS_RMSE | LM_RMSE | IA_RMSE | PLS-LM_RMSE | PLS-IA_RMSE |
|---|---|---|---|---|---|---|
| QUOT1 | 0.352 | 0.680 | 0.714 | 0.845 | -0.034 | -0.165 |
| QUOT2 | 0.310 | 0.693 | 0.767 | 0.834 | -0.074 | -0.141 |
| QUOT3 | 0.313 | 0.622 | 0.654 | 0.751 | -0.032 | -0.129 |
| QUOT4 | 0.206 | 0.663 | 0.690 | 0.744 | -0.027 | -0.081 |
| QUOT5 | 0.243 | 0.590 | 0.641 | 0.678 | -0.051 | -0.088 |
| QUOT6 | 0.291 | 0.664 | 0.683 | 0.788 | -0.019 | -0.124 |
Source: Developed by the authors based on the data analysis
Note: QUOT, Quality of operating theatre
Discussion
This study aimed to investigate the factors influencing the quality of operating theatres and the moderating role of operating theatre management in medical waste management and the quality of operating theatres. First, the automated doors and scrub stations positively and significantly influence the quality of the operating theatre, consistent with the findings of [17, 32] stated that automated doors reduce contamination risks and improve operational efficiency [35, 93], indicated the importance of automated doors in maintaining sterile environments and door opening affects contamination control. Second, the HEPA filters positively and significantly influence the quality of operating theatre, aligning with the findings of [18, 36], who highlighted that infection rates and airborne contaminations in operating theatre will reduced through HEPA filters [37], revealed that HEPA filters contribute to infection control and air cleanliness ensure a high-quality surgical environment.
Third, medical waste management positively and significantly influences the quality of operating theatre, consistent with the findings of [40, 41], which mentioned the importance of comprehensive waste segregation and sterilization to mitigate contamination risks [42, 43], pointed out the importance of sustainability and recycling initiatives in improving waste management efficiency. Fourth, operating theatre management has a positive and significant influence on the quality of the operating theatre, aligning with the findings of [20, 45], who demonstrated the benefits of resource optimization [47, 48]. also found that structured operating theatre management improves patient safety and workflow efficiency, ultimately enhancing the quality of the operating theatre.
Fifth, pathology services in the operating theatre positively and significantly influence the quality of the operating theatre, consistent with the findings of [21, 50]. These studies suggest that real-time pathology services enhance surgical decision-making [52]. It was also noted that pathology services improve specimen sampling and workflow efficiency, ultimately leading to better patient outcomes. Sixth, a unidirectional workflow positively and significantly influences the quality of the operating theatre, aligning with the findings of [54, 57], which established that a unidirectional workflow minimizes contamination risks and improves operating theatre effectiveness [22, 56]. explained that structured workflow management enhances efficiency and surgical safety.
Seventh, the indirect effect of operating theatre management on the relationship between medical waste management and the quality operating theatre confirms a moderating role consistent with the findings of [23, 59], which confirmed the need for structured waste management guidelines and policies to reduce environmental impact and enhance the sustainability of the operating theatre [60, 61, 94] proposed the role of operating theatre management in improving operational efficiency and minimize hazardous waste. Additionally, it supports the Donabedian quality of care framework by aligning structure, process, and outcome to ensure quality in the operating theatre, promoting total quality management [95]. Therefore, this study empirically validates the influence of the key factors on the quality of operating theatre and highlights the critical role of infection control measures in ensuring optimal surgical outcomes. Thus, the importance of efficient workflow management in improving the quality of operating theatre underlines the significance of environmental sustainability in maintaining high-quality surgical environments.
Conclusion
This study identified the key managerial and infrastructural factors of multispecialty hospitals in the quality operating theatres. Based on the results, the most significant factors are automated doors and scrub stations, HEPA filters, medical waste management, pathology services, and unidirectional workflows. Moreover, unidirectional workflow has the most substantial influence on the quality of the operating theatre, underscoring the importance of structural movement in reducing contamination risks. Additionally, operating theatre management moderates the relationship between medical waste management and the quality of the operating theatre, highlighting the role of effective administration. Thus, the findings align with the Donabedian quality of care framework, which reinforces the interplay between structure, process, and outcomes in quality healthcare. These insights offer practical implications for policymakers and hospital administrators, supporting strategic improvements in surgical environments.
Theoretical implications
This study reinforces the applicability of the Donabedian framework in assessing the quality of care. It empirically demonstrates the structure (automated doors and scrub stations) and procedural (unidirectional workflow and medical waste management) factors that contribute to the quality of healthcare. Furthermore, the extension of the framework by identifying the moderating effect of operating theatre management on the relationship between medical waste management and the quality of operating theatre expands the existing literature on operational efficiency and healthcare management. In emerging economies, the study’s findings address research gaps related to quality operating theatres, providing insights relevant to resource-constrained healthcare settings and differentiating them from studies conducted in Western contexts. Moreover, the study deepens the theoretical perspectives on the interplay between management and infrastructure, highlighting the need for an integrated approach to improving surgical outcomes, patient care, and safety.
Practical implications
First, the practical implications for hospital administration include investing in automated systems, such as automated doors, scrub stations, and HEPA filters for infection control; implementing unidirectional workflow to improve surgical efficiency and reduce cross-contamination; and adopting effective operating theatre management practices to enhance patient safety and optimize resource utilization. Second, the practical implications for policymakers regarding standardized guidelines for framing and implementing medical waste management and integrated pathology services are to ensure consistent quality and proper operating theatre protocols, as well as mandatory staff training to enhance managerial efficiency and promote best practices. Third, the practical implications for healthcare practitioners include the utilization of real-time data tracking tools, such as air quality monitors and waste disposal logs, to maintain compliance with hygiene and safety standards. Additionally, the adoption of evidence-based management strategies is recommended to minimize risk and improve operating theatre processes associated with surgical environments.
Limitations and future research
Even though the study brought significant advantages to the existing literature, there are a few limitations that will be addressed by future research. First, the study focused on multispecialty private hospitals in India, which limits the generalizability to rural healthcare and public hospital settings. Therefore, future research could explore different healthcare sectors to identify variations in the quality of operating theatres. Second, the study employed cross-sectional data, which limits causal inference; therefore, future research can assess the long-term impact of artificial intelligence, waste management, and technological advancements on the quality of operating theatres. Although no significant language-related issues were reported during data collection, the absence of native researchers and the potential for language or cultural misunderstandings remain the limitations of the study. Third, the study used a marker-variable test to avoid bias despite the fact that the responses from healthcare professionals may be biased, so future research could include infection incidence and surgical success rates connected to patient-centric metrics to improve validity. Fourth, the study doesn’t include post-surgical recovery in measuring the quality of the operating theatre, so that future research could measure operating theatre efficiency by patient outcomes. Finally, the study’s findings are specific to the Indian context, so future research could include comparative studies with Western or high-income countries, which would help differentiate universal quality determinants from region-specific factors.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to express their sincere gratitude to the Editor and the anonymous reviewers of the journal for their constructive comments, insightful suggestions, and valuable feedback, which have significantly improved the quality and clarity of this manuscript. Their time and effort in reviewing our work are deeply appreciated. Also, heartfelt thanks to the friends and family members who helped in collecting the data from the respondents.
Author contributions
Nidhi and Sridhar - Main concept, data collection, theoretical perspective, and framework. Jayendira - Main manuscript, data analysis, tables, figures, discussion, and implications. Shabana - Review of literature and support.
Funding
The University of Technology Bahrain provides open-access funding.
Data availability
The datasets for this article are not publicly available due to restrictions set by the data holder. Requests to access the datasets should be directed to the authors.
Declarations
Ethics approval and consent to participate
This study was conducted in full compliance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Research Center at the University of Technology, Bahrain (UTB2024CAFSEC020) on 1 December 2024. Also, the research adhered to the ethical principles outlined in the IRB-HSBS informed consent guidelines of the University of Technology Bahrain. Further, informed consent was obtained from all the participants included in the study. Moreover, the study exclusively involved data collection from surgeons, scrub nurses or operating room nurses, anaesthesiologists or anesthesia providers, pathologists, operating theatre managers or coordinators, and others directly connected to the operating theatre activities from private multispecialty hospitals in India. Prior to their participation, all individuals were furnished with a comprehensive information sheet that outlined the purpose and details of the research. Participation in the study was entirely voluntary, and individuals were asked to complete the questionnaire only after they had thoroughly reviewed the information sheet and had any questions or concerns addressed. Data collectors or authors stress the importance of informed consent, ensuring that all participants were fully aware of the study’s objectives and their voluntary role in contributing to this research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Generative AI and AI-assisted technologies in the writing process
During the preparation of this work, the author(s) used Grammarly to check the spelling and grammar. After using this tool/service, the author(s) reviewed and edited the content as needed and take full responsibility for the content of the publication.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mosadeghrad AM, Afshari M. Quality management effects on operating theater’s productivity: a participatory action research. TQM J. 2020;33:882–95. 10.1108/TQM-04-2020-0083. [Google Scholar]
- 2.Endalamaw A, Khatri RB, Mengistu TS, et al. A scoping review of continuous quality improvement in healthcare system: conceptualization, models and tools, barriers and facilitators, and impact. BMC Health Serv Res. 2024;24:487. 10.1186/S12913-024-10828-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Junaid SB, Imam AA, Balogun AO et al. (2022) Recent Advancements in Emerging Technologies for Healthcare Management Systems: A Survey. Healthc. 10:1–45. [DOI] [PMC free article] [PubMed]
- 4.Perez ER, Kerko R, Lever N, et al. Operating room relay strategy for turnover time improvement: a quality improvement project. BMJ Open Qual. 2022;11:e001957. 10.1136/BMJOQ-2022-001957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spagnolo AM, Ottria G, Amicizia D, et al. Operating theatre quality and prevention of surgical site infections. J Prev Med Hyg. 2013;54:131–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Gradisnik L, Bunc G, Ravnik J, Velnar T. Enhancing surgical safety: Microbiological air control in operating theatres at university medical centre Maribor. Diagnostics. 2024;14:1054. 10.3390/diagnostics14101054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vladu A, Ghitea TC, Daina LG et al. (2024) Enhancing Operating Room Efficiency: The Impact of Computational Algorithms on Surgical Scheduling and Team Dynamics. Healthcare 12:1906. 10.3390/HEALTHCARE12191906 [DOI] [PMC free article] [PubMed]
- 8.Bredella MA, Fintelmann FJ, Iafrate AJ, et al. Administrative alignment for integrated diagnostics leads to shortened time to diagnose and service optimization. Radiology. 2024;312:e240335. 10.1148/RADIOL.240335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varnosfaderani SM, Forouzanfar M. The role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering. 2024;11:337. 10.3390/BIOENGINEERING11040337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ducatman BS, Ducatman AM, Crawford JM, et al. The value proposition for pathologists: A population health approach. Acad Pathol. 2020;7:2374289519898857. 10.1177/2374289519898857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhaskar HL. Establishing a link among total quality management, market orientation and organizational performance. TQM J. 2020;32:1507–24. 10.1108/TQM-01-2019-0012. [Google Scholar]
- 12.Bali RK. Operating room protocols and infection control. Oral and maxillofacial surgery. Clinician. 2020;24:173–94. 10.1007/978-981-15-1346-6_9. [Google Scholar]
- 13.Dallolio L, Raggi A, Sanna T, et al. Surveillance of environmental and procedural measures of infection control in the operating theatre setting. Int J Environ Res Public Health 2018. 2017;15:1546. 10.3390/IJERPH15010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Benna S. Infection control in operating theatres. J Perioper Pract. 2012;22:318–22. 10.1177/175045891602201002. [DOI] [PubMed] [Google Scholar]
- 15.Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83:691–729. 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santry HP, Strassels SA, Ingraham AM, et al. Identifying the fundamental structures and processes of care contributing to emergency general surgery quality using a mixed-methods Donabedian approach. BMC Med Res Methodol. 2020;20:247. 10.1186/s12874-020-01096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glowicz JB, Landon E, Sickbert-Bennett EE, et al. SHEA/IDSA/APIC practice recommendation: strategies to prevent healthcare-associated infections through hand hygiene: 2022 update. Infect Control Hosp Epidemiol. 2023;44:355–76. 10.1017/ice.2022.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li T, Katz A, Osei-Twum J-A, et al. Science tells Us that portable air filters reduce infection risk. It’s time for public health authorities to make this clear. J Infect Public Health. 2025;18:102650. 10.1016/j.jiph.2024.102650. [DOI] [PubMed] [Google Scholar]
- 19.Moya E, Bryant SA, Horneck N, et al. Advancing sustainability in healthcare: A scoping review of global recycling practices in operating rooms. Am J Surg. 2025;241:116178. 10.1016/J.AMJSURG.2024.116178. [DOI] [PubMed] [Google Scholar]
- 20.Agnoletti V, Buccioli M, Padovani E, et al. Operating room data management: improving efficiency and safety in a surgical block. BMC Surg. 2013;13:7. 10.1186/1471-2482-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaafar H. Intra-Operative frozen section consultation: concepts, applications and limitations. Malaysian J Med Sciences: MJMS. 2006;13:4. [PMC free article] [PubMed] [Google Scholar]
- 22.Fan L, Ye L, Gong J, et al. Surgical workflow and infection prevention and control strategies for patients with COVID-19 during the epidemic in children’s hospitals. Translational Pediatr. 2022;11:1787–95. 10.21037/TP-22-463/COIF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Talbot S, Moore D. Waste management in the operating theatre. Surgeon: J Royal Colleges Surg Edinb Irel. 2024;22:248–52. 10.1016/J.SURGE.2024.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Ghofrani M, Valizadeh L, Zamanzadeh V, et al. Adapting the Donabedian model in undergraduate nursing education: a modified Delphi study. BMC Med Educ. 2024;24:202. 10.1186/s12909-024-05187-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guta NM. Application of Donabedian quality-of-care framework to assess quality of neonatal resuscitation, its outcome, and associated factors among resuscitated newborns at public hospitals of East Wollega zone, oromia, Western ethiopia, 2021. BMC Pediatr. 2022;22:605. 10.1186/s12887-022-03638-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ameh S, Gómez-Olivé FX, Kahn K, et al. Relationships between structure, process and outcome to assess quality of integrated chronic disease management in a rural South African setting: applying a structural equation model. BMC Health Serv Res. 2017;17:229. 10.1186/s12913-017-2177-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Endalamaw A, Khatri RB, Erku D, et al. Successes and challenges towards improving quality of primary health care services: a scoping review. BMC Health Serv Res. 2023;23:893. 10.1186/s12913-023-09917-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pogorzelska-Maziarz M, de Cordova PB, Manning M, Lou, et al. Voices from frontline nurses on care quality and patient safety during COVID-19: an application of the Donabedian model. Am J Infect Control. 2023;51:1295–301. 10.1016/j.ajic.2023.08.014. [DOI] [PubMed] [Google Scholar]
- 29.Naz S, Saleem S, Islam ZS, et al. Obstetric triage improvement process using the Donabedian model of quality care: a quality improvement initiative. BMJ Open Qual. 2022;11:e001483. 10.1136/bmjoq-2021-001483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhaskar HL. A conceptual study of total quality management. In: Kumar S, Juyal SL, Deshpande PP, Kumar R, editors. Handbook of management and behavioural science. Delhi: Wisdom; 2012. pp. 217–31. [Google Scholar]
- 31.Otter JA, Yezli S, Barbut F, Perl TM. An overview of automated room disinfection systems: when to use them and how to choose them. Decontamination in hospitals and healthcare. Elsevier; 2020. pp. 323–69.
- 32.Reddy K, Gharde P, Tayade H, et al. Advancements in robotic surgery: A comprehensive overview of current utilizations and upcoming frontiers. Cureus. 2023;15:1–15. 10.7759/cureus.50415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gould DJ, Moralejo D, Drey N, et al. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Reviews. 2017;2017:1–96. 10.1002/14651858.CD005186.pub4. [DOI] [PubMed] [Google Scholar]
- 34.Lansing SS, Moley JP, McGrath MS, et al. High number of door openings increases the bacterial load of the operating room. Surg Infect. 2021;22:684–9. 10.1089/sur.2020.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Camera A, Della, Cevenini G, Nante N, et al. Sliding doors: how does their opening affect particulate matter levels in operating theatres? Int J Infect Control. 2022;18:1–8. 10.3396/ijic.v18.22156. [Google Scholar]
- 36.Lans JLA, Mathijssen NMC, Traversari AAL, et al. Capital and operational expenditures of different operating room air-handling installations with conventional or ultra-clean air supply systems. J Building Eng. 2023;78:107714. 10.1016/j.jobe.2023.107714. [Google Scholar]
- 37.Soleha TU, Oktafany, Ayu PR, Nafisah A. (2024) The effectiveness of using HEPA filters in reducing the number of airborne bacteria in the operating room area. In: The 4th International Conference on Applied Sciences, Mathematics, and Informatics: ICASMI2022. AIP Publishing, p 50026.
- 38.Ereth MH, Hess DH, Driscoll A, et al. Particle control reduces fine and ultrafine particles greater than HEPA filtration in live operating rooms and kills biologic warfare surrogate. Am J Infect Control. 2020;48:777–80. 10.1016/j.ajic.2019.11.017. [DOI] [PubMed] [Google Scholar]
- 39.Sadrizadeh S, Aganovic A, Bogdan A, et al. A systematic review of operating room ventilation. J Building Eng. 2021;40:102693. 10.1016/j.jobe.2021.102693. [Google Scholar]
- 40.Lee SM, Lee D. Effective medical waste management for sustainable green healthcare. Int J Environ Res Public Health. 2022;19:14820. 10.3390/ijerph192214820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ramos T, Christensen TB, Oturai N, Syberg K. Reducing plastic in the operating theatre: towards a more circular economy for medical products and packaging. J Clean Prod. 2023;383:135379. 10.1016/j.jclepro.2022.135379. [Google Scholar]
- 42.Ong PJ, Moore D, Boyland R, et al. No time to waste: improving waste segregation in the operating theatre. BJA Open. 2022;4:100077. 10.1016/j.bjao.2022.100077. [Google Scholar]
- 43.Selvy M, Bellin M, Slim K, Muret J. Eco-responsibility in the operating theater: an urgent need for organizational transformation. J Visc Surg. 2020;157:301–7. 10.1016/J.JVISCSURG.2020.07.001. [DOI] [PubMed] [Google Scholar]
- 44.Lorenzon L, Magalini S, Antolino L, et al. Impact of operating room waste in a high-volume institution and strategies for reduction: results from the CARING NATURE project. Br J Surg. 2025;112. 10.1093/BJS/ZNAF027. [DOI] [PMC free article] [PubMed]
- 45.Morri M, Forni C, Campagna A, et al. Evaluation of the performance of an innovative model for the organisation of specialised hospital activities throughout italy: the diffuse hospital. Ann Ital Chir. 2025;96:221–7. 10.62713/AIC.3565. [DOI] [PubMed] [Google Scholar]
- 46.Slim K, Veziant J, Enguix A, Zieleskiewicz L. Environmental impact of the enhanced recovery pathway in colorectal surgery: A simulation study. Colorectal Disease: Official J Association Coloproctology Great Br Irel. 2025;27:e17247. 10.1111/CODI.17247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang JL, Khalid H, Alvaran KAB, et al. Improving laryngeal procedure workflow: moving from the operating room to the outpatient setting. Laryngoscope. 2025;135:1132–42. 10.1002/LARY.31849. [DOI] [PubMed] [Google Scholar]
- 48.Saleem J, Brown O, Mclean C, et al. The provision of a trauma bed in theatre recovery and its impact on trauma theatre efficiency: experience from a high-volume trauma unit. Annals Royal Coll Surg Engl. 2024;107:1–6. 10.1308/RCSANN.2023.0106/ASSET/IMAGES/RCSANN.2023.0106.02.JPG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Micco F, De BA, De, Scendoni R, et al. From the operating theater to the pathology laboratory: failure mode, effects, and criticality analysis of the biological samples transfer. Healthcare. 2024;12:2279. 10.3390/HEALTHCARE12222279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iwasaki M, Ishihara S, Okada S, et al. Prognostic impact of using combined plasma fibrinogen level and Neutrophil-to-Lymphocyte ratio in resectable Non-small cell lung cancer. Ann Surg Oncol. 2022;29:5699–707. 10.1245/S10434-022-11835-3/METRICS. [DOI] [PubMed] [Google Scholar]
- 51.Start RD, Cross SS, Smith JHF. Assessment of specimen fixation in a surgical pathology service. J Clin Pathol. 1992;45:546–7. 10.1136/JCP.45.6.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.D’Angelo R, Mejabi O. Getting it right for patient safety: specimen collection process improvement from operating room to pathology. Am J Clin Pathol. 2016;146:8–17. 10.1093/AJCP/AQW057. [DOI] [PubMed] [Google Scholar]
- 53.Kang JH, Kim EJ, Choi JH, et al. Minimizing contamination in the use of personal protective equipment: simulation results through tracking contamination and enhanced protocols. Am J Infect Control. 2020;49:713. 10.1016/J.AJIC.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Whyte W, Mackintosh CA, Whyte WM. The design and testing of unidirectional airflow operating theatres. Int J Vent. 2022;21:247–62. 10.1080/14733315.2021.1889104. [Google Scholar]
- 55.Bhaskar HL. Business process reengineering: A process based management tool. Serbian J Manage. 2018;13:63–87. 10.5937/sjm13-13188. [Google Scholar]
- 56.Andersson AE, Petzold M, Bergh I, et al. Comparison between mixed and laminar airflow systems in operating rooms and the influence of human factors: experiences from a Swedish orthopedic center. Am J Infect Control. 2014;42:665–9. 10.1016/J.AJIC.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 57.Leber AL. General aspects of molecular diagnostics. In: Wiley, editor. Clinical microbiology procedures handbook. 4th ed. Ltd: Wiley; 2016. pp. 1–12. [Google Scholar]
- 58.McElroy C, Skegg E, Mudgway M, et al. Psychological safety and hierarchy in operating room debriefing: reflexive thematic analysis. J Surg Res. 2024;295:567–73. 10.1016/J.JSS.2023.11.054. [DOI] [PubMed] [Google Scholar]
- 59.Warda G. Anesthesia and operating room waste management. Acad Med Surg. 2024. 10.62186/001C.123424. [Google Scholar]
- 60.Magasich-Airola N, Souberbielle Q, L’Hotel L, et al. Waste management in Belgian operating rooms: A narrative review. Acta Anaesthesiologica Belgica. 2024;75:149–54. 10.56126/75.2.47. [Google Scholar]
- 61.Kaposi A, Nagy A, Gomori G, Kocsis D. Analysis of healthcare waste and factors affecting the amount of hazardous healthcare waste in a university hospital. J Mater Cycles Waste Manage. 2024;26:1169–80. 10.1007/S10163-024-01890-1/TABLES/4. [Google Scholar]
- 62.NABH. (2025) NABH Accredited Hospitals. In: Natl. Accredit. Board Hosp. Healthc. Provid. https://portal.nabh.co/frmViewAccreditedHosp.aspx#gsc.tab=0. Accessed 29 Mar 2025.
- 63.(2023) New age healthcare delivery models in India. In: Fed. Indian Chambers Commer. KPMG, Ind. https://assets.kpmg.com/content/dam/kpmgsites/in/pdf/2023/10/new-age-healthcare-delivery-models-in-india-20-plus-modes-to-redefine-healthcare-landscape.pdf.coredownload.inline.pdf. Accessed 29 Mar 2025.
- 64.Ghosh D. (2025) 7 medical tourism destinations in India. In: India TV. https://www.indiatvnews.com/photos/fashion-lifestyle-7-medical-tourism-destinations-in-india-2025-01-31-973952. Accessed 29 Mar 2025.
- 65.Kumar A. The transformation of the Indian healthcare system. Cureus. 2023;15:e39079. 10.7759/CUREUS.39079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Likert R. A technique for the measurement of attitudes. Archives Psychol. 1932;140:5–55. [Google Scholar]
- 67.Hair, Hult GTM, Ringle CM, Sarstedt MA. A primer on partial least squares structural equation modeling (PLS-SEM). 2nd ed. Thousand Oaks, CA: Sage Publication; 2017. [Google Scholar]
- 68.IBEF. (2025) Healthcare Industry in India. In: India Brand Equity Found. https://www.ibef.org/industry/healthcare-india. Accessed 29 Mar 2025.
- 69.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60. 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 70.Sarstedt M, Hair JF, Cheah J-H, et al. How to specify, estimate, and validate higher-order constructs in PLS-SEM. Australasian Mark J. 2019;27:197–211. 10.1016/j.ausmj.2019.05.003. [Google Scholar]
- 71.Dash G, Paul J. CB-SEM vs PLS-SEM methods for research in social sciences and technology forecasting. Technol Forecast Soc Chang. 2021;173:121092. 10.1016/j.techfore.2021.121092. [Google Scholar]
- 72.ICMR. (2017) National Ethical Guidelines for Biomedical and Health Research Involving Human Participants. New Delhi.
- 73.Association WM. World medical association declaration of Helsinki. JAMA. 2013;310:2191. 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 74.Ringle CM, Wende S, Baker J-M. (2022) SmartPLS 4. Oststeinbek: SmartPLS. In: Smart-Pls. http://www.smartpls.com. Accessed 8 Jun 2024.
- 75.Chin WW, Marcelin BL, Newsted PR. A partial least squares latent variable modeling approach for measuring interaction effects: results from a Monte Carlo simulation study and an electronic-mail emotion/adoption study. Inform Syst Res. 2003;14:189–217. 10.1287/isre.14.2.189.16018. [Google Scholar]
- 76.Kock N, Lynn GS. Lateral collinearity and misleading results in variance-based SEM: an illustration and recommendations. J Association Inform Syst. 2012;13:546–80. 10.17705/1jais.00302. [Google Scholar]
- 77.Kock N. Common method bias in PLS-SEM: A full collinearity assessment approach. Int J e-Collaboration. 2015;11:1–10. 10.4018/ijec.2015100101. [Google Scholar]
- 78.Diamantopoulos A, Siguaw JA. Formative versus reflective indicators in organizational measure development: A comparison and empirical illustration. Br J Manag. 2006;17:263–82. 10.1111/j.1467-8551.2006.00500.x. [Google Scholar]
- 79.Miller BK. Measurement of academic entitlement. Psychol Rep. 2013;113:654–74. 10.2466/17.08.PR0.113x25z1. [DOI] [PubMed] [Google Scholar]
- 80.Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended Two-Step approach. Psychol Bull. 1988;103:411–23. 10.1037/0033-2909.103.3.411. [Google Scholar]
- 81.Hair JF, Hult GTM, Ringle CM, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM). 3rd ed. Los Angeles, CA, USA: Sage; 2022. [Google Scholar]
- 82.Ramayah T, Cheah J, Chuah F, et al. Partial least squares structural equation modeling (PLS-SEM) using SmartPLS 3.0 an updated and practical guide to statistical analysis. 2nd ed. Malaysia: Pearson, Kuala Lumpur; 2018. [Google Scholar]
- 83.Franke G, Sarstedt M. Heuristics versus statistics in discriminant validity testing: a comparison of four procedures. Internet Res. 2019;29:430–47. 10.1108/IntR-12-2017-0515. [Google Scholar]
- 84.Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. 2015;43:115–35. 10.1007/s11747-014-0403-8. [Google Scholar]
- 85.Cohen P, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences, second. Taylor and Francis Ltd.; 2014.
- 86.Field A. Discovering statistics using IBM SPSS statistics. 6th ed. Thousand Oaks, California: Sage Publication; 2024. [Google Scholar]
- 87.Hair JF, Babin BJ, Anderson RE, Black WC. Multivariate data analysis. 8th ed. United Kingdom: Cengage Learning; 2018. [Google Scholar]
- 88.Tabachnick B, Fidell L. Using multivariate statistics. 7th ed. London: Pearson; 2018. [Google Scholar]
- 89.Hair J, Alamer A. Partial least squares structural equation modeling (PLS-SEM) in second Language and education research: guidelines using an applied example. Res Methods Appl Linguistics. 2022;1:100027. 10.1016/j.rmal.2022.100027. [Google Scholar]
- 90.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instruments Computers. 2004;36:717–31. 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- 91.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- 92.Shmueli G, Sarstedt M, Hair JF, et al. Predictive model assessment in PLS-SEM: guidelines for using PLSpredict. Eur J Mark. 2019;53:2322–47. 10.1108/EJM-02-2019-0189. [Google Scholar]
- 93.Bhaskar HL. A critical analysis of information technology and business process reengineering. Int J Productivity Qual Manage. 2016;19:98–115. 10.1504/IJPQM.2016.078018. [Google Scholar]
- 94.Bhaskar HL. BPR as a quality improvement tool. Handbook of management, technology and social sciences, handbook. Rajastan: Society of Engineering & Management Sciences, Jodhpur; 2014. pp. 1–10. [Google Scholar]
- 95.Bhaskar HL. A comparative analysis of business process reengineering and total quality management. Global J Bus Manage. 2015;9:11–28. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets for this article are not publicly available due to restrictions set by the data holder. Requests to access the datasets should be directed to the authors.