Abstract
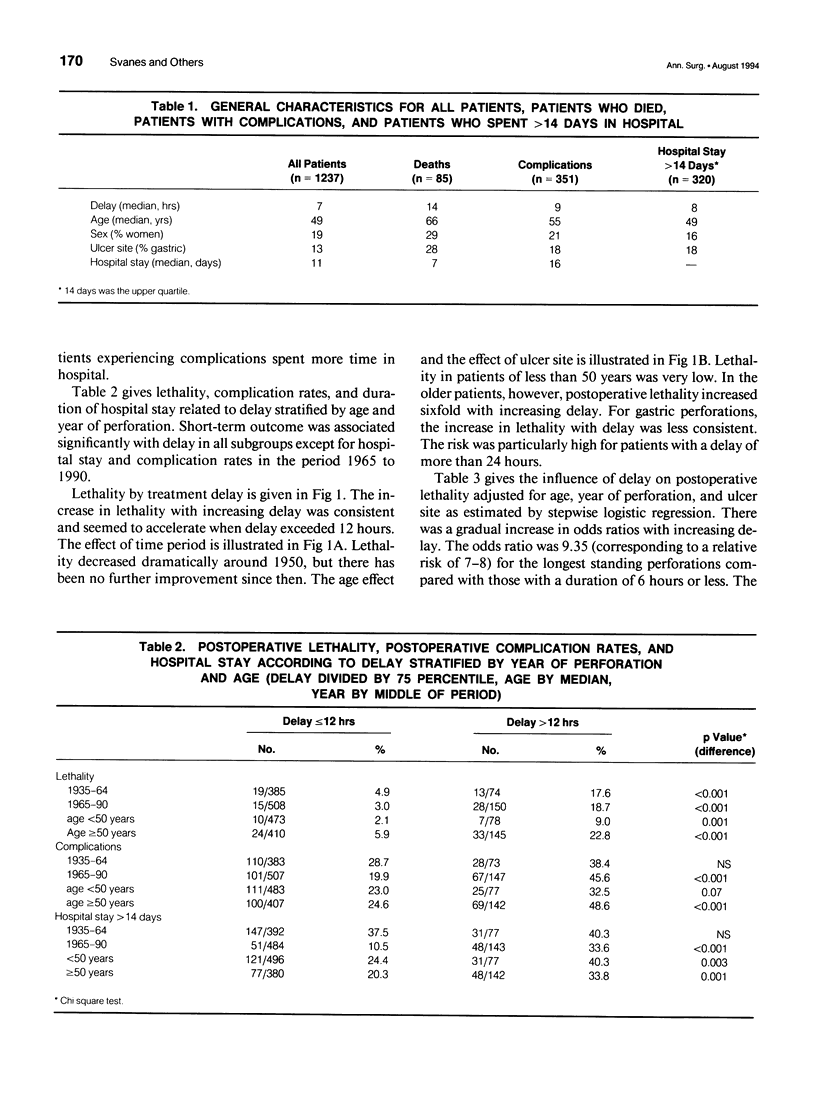
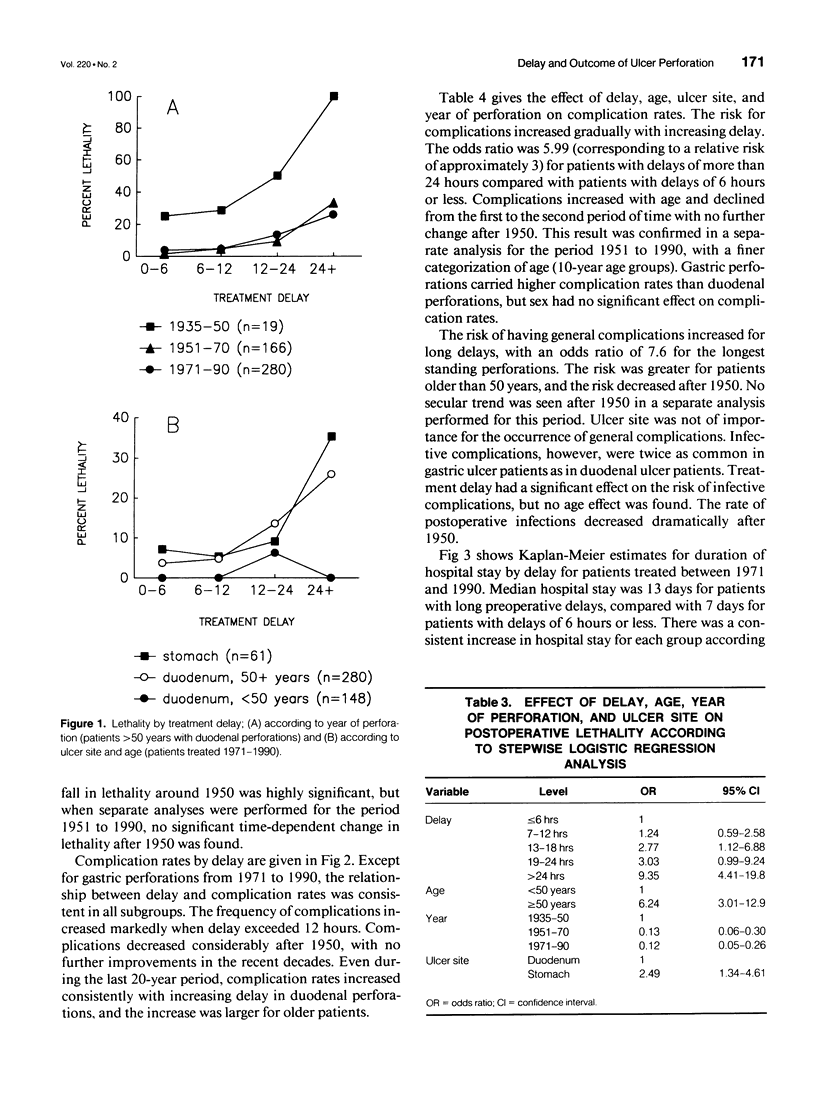
OBJECTIVE: The authors assessed the consequences of delayed treatment for ulcer perforation with regard to short-term and long-term survival, complication rates, and length of hospital stay. SUMMARY BACKGROUND DATA: Important adverse effects of delayed treatment have not been studied previously. Conflicting results have been given with regard to short-term survival. METHODS: One thousand two hundred ninety-two patients operated on for perforated peptic ulcer in the Bergen area between 1935 and 1990 were studied. The effect of delay on postoperative lethality and complications adjusted for age, sex, ulcer site, and year of perforation was analyzed by stepwise logistic regression. The effect of delay on duration of hospital stay adjusted for potential confounding factors was analyzed by Cox proportional hazards regression. Observed survival was estimated by the Kaplan-Meier method, and expected survival was calculated from population mortality data. RESULTS: Adverse effects increased markedly when delay exceeded 12 hours. Delay of more than 24 hours increased lethality sevenfold to eightfold, complication rate to threefold, and length of hospital stay to twofold, compared with delay of 6 hours or less. The reduced long-term survival for patients treated more than 12 hours after perforation could be attributed entirely to high postoperative mortality. CONCLUSIONS: Delayed treatment after peptic ulcer perforation reduced survival, increased complication rates, and caused prolonged hospital stay. To improve outcome after ulcer perforation, an effort should be made to keep delay at less 12 hours, particularly in elderly patients.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agrez M. V., Senthiselvan S., Henry D. A., Mitchell A., Duggan J. M. Perforated peptic ulcer in the Hunter region: a review of 174 cases. Aust N Z J Surg. 1992 May;62(5):338–343. doi: 10.1111/j.1445-2197.1992.tb07200.x. [DOI] [PubMed] [Google Scholar]
- Bodner B., Harrington M. E., Kim U. A multifactorial analysis of mortality and morbidity in perforated peptic ulcer disease. Surg Gynecol Obstet. 1990 Oct;171(4):315–320. [PubMed] [Google Scholar]
- Boey J., Choi S. K., Poon A., Alagaratnam T. T. Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg. 1987 Jan;205(1):22–26. doi: 10.1097/00000658-198701000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdette W. J., Rasmussen B. Perforated peptic ulcer. Surgery. 1968 Apr;63(4):576–585. [PubMed] [Google Scholar]
- Cohen M. M. Treatment and mortality of perforated peptic ulcer: a survey of 852 cases. Can Med Assoc J. 1971 Aug 7;105(3):263–passim. [PMC free article] [PubMed] [Google Scholar]
- Devitt J. E., Taylor G. A. Perforated peptic ulcer. Can Med Assoc J. 1967 Mar 4;96(9):519–523. [PMC free article] [PubMed] [Google Scholar]
- Graves A. M. Perforated Peptic Ulcer in German Clinics: An Analysis of 4,402 Cases. Ann Surg. 1933 Aug;98(2):197–209. doi: 10.1097/00000658-193308000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunshefski L., Flancbaum L., Brolin R. E., Frankel A. Changing patterns in perforated peptic ulcer disease. Am Surg. 1990 Apr;56(4):270–274. [PubMed] [Google Scholar]
- Hennessy E. Perforated peptic ulcer: mortality and morbidity in 603 cases. Aust N Z J Surg. 1969 Feb;38(3):243–252. [PubMed] [Google Scholar]
- Horowitz J., Kukora J. S., Ritchie W. P., Jr All perforated ulcers are not alike. Ann Surg. 1989 Jun;209(6):693–697. doi: 10.1097/00000658-198906000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvin T. T. Mortality and perforated peptic ulcer: a case for risk stratification in elderly patients. Br J Surg. 1989 Mar;76(3):215–218. doi: 10.1002/bjs.1800760304. [DOI] [PubMed] [Google Scholar]
- Jordan P. H., Jr, Morrow C. Perforated peptic ulcer. Surg Clin North Am. 1988 Apr;68(2):315–329. doi: 10.1016/s0039-6109(16)44480-4. [DOI] [PubMed] [Google Scholar]
- Krenzien J., Röding H., Rudtke B. Das perforierte Gastroduodenalulkus. II. Risikoanalyse zur prognostischen Beurteilung des postoperativen Verlaufes. Zentralbl Chir. 1990;115(8):471–481. [PubMed] [Google Scholar]
- Lanng C., Palnaes Hansen C., Christensen A., Thagaard C. S., Lassen M., Klaerke A., Tønnesen H., Ostgaard S. E. Perforated gastric ulcer. Br J Surg. 1988 Aug;75(8):758–759. doi: 10.1002/bjs.1800750812. [DOI] [PubMed] [Google Scholar]
- Mattingly S. S., Ram M. D., Griffen W. O., Jr Factors influencing morbidity and mortality in perforated duodenal ulcer. Am Surg. 1980 Feb;46(2):61–66. [PubMed] [Google Scholar]
- NOORDIJK J. A. Perforated peptic ulcer: the results of treatment in the Netherlands, 1934-1950; an analysis of 2551 cases. Arch Chir Neerl. 1953;5(4):262–270. [PubMed] [Google Scholar]
- Olsen R. K., Liavåg I., Roland M. Ulcus perforatum. Tidsskr Nor Laegeforen. 1983 Oct 10;103(28):1924–1927. [PubMed] [Google Scholar]
- Svanes C., Salvesen H., Espehaug B., Søreide O., Svanes K. A multifactorial analysis of factors related to lethality after treatment of perforated gastroduodenal ulcer. 1935-1985. Ann Surg. 1989 Apr;209(4):418–423. doi: 10.1097/00000658-198904000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svanes C., Salvesen H., Stangeland L., Svanes K., Søreide O. Perforated peptic ulcer over 56 years. Time trends in patients and disease characteristics. Gut. 1993 Dec;34(12):1666–1671. doi: 10.1136/gut.34.12.1666. [DOI] [PMC free article] [PubMed] [Google Scholar]


