Abstract
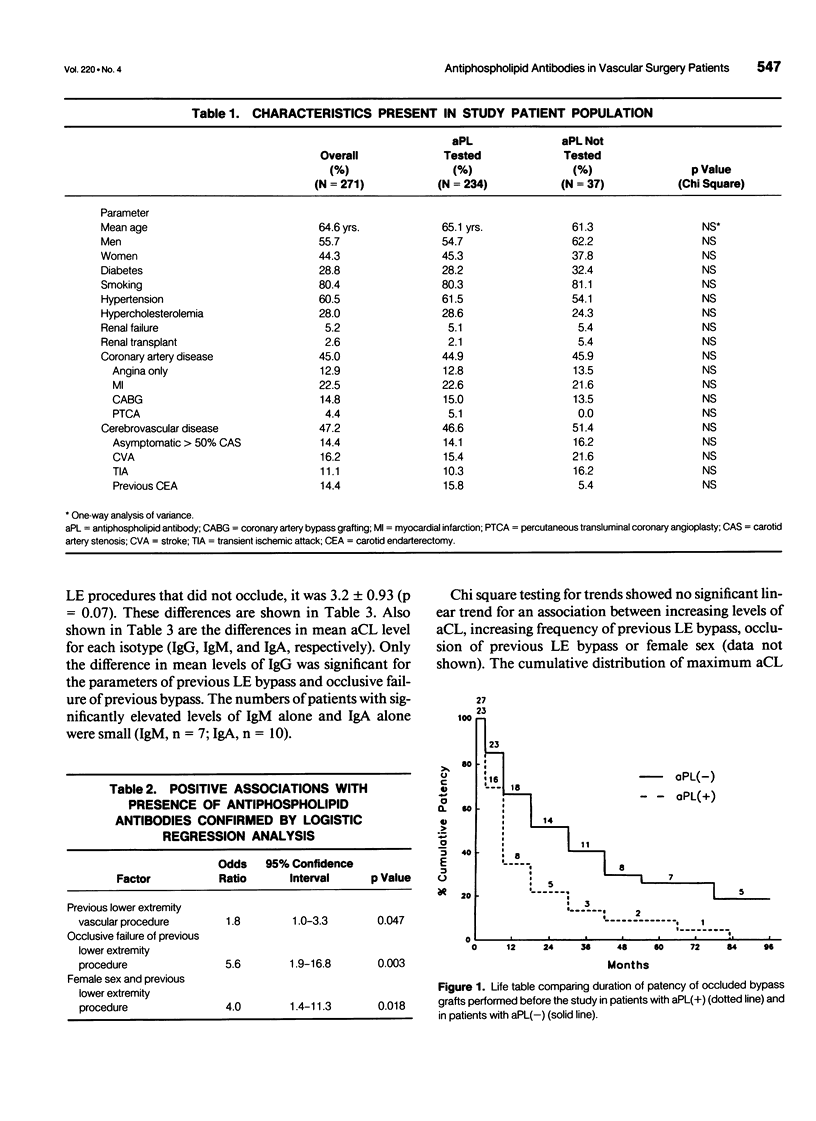
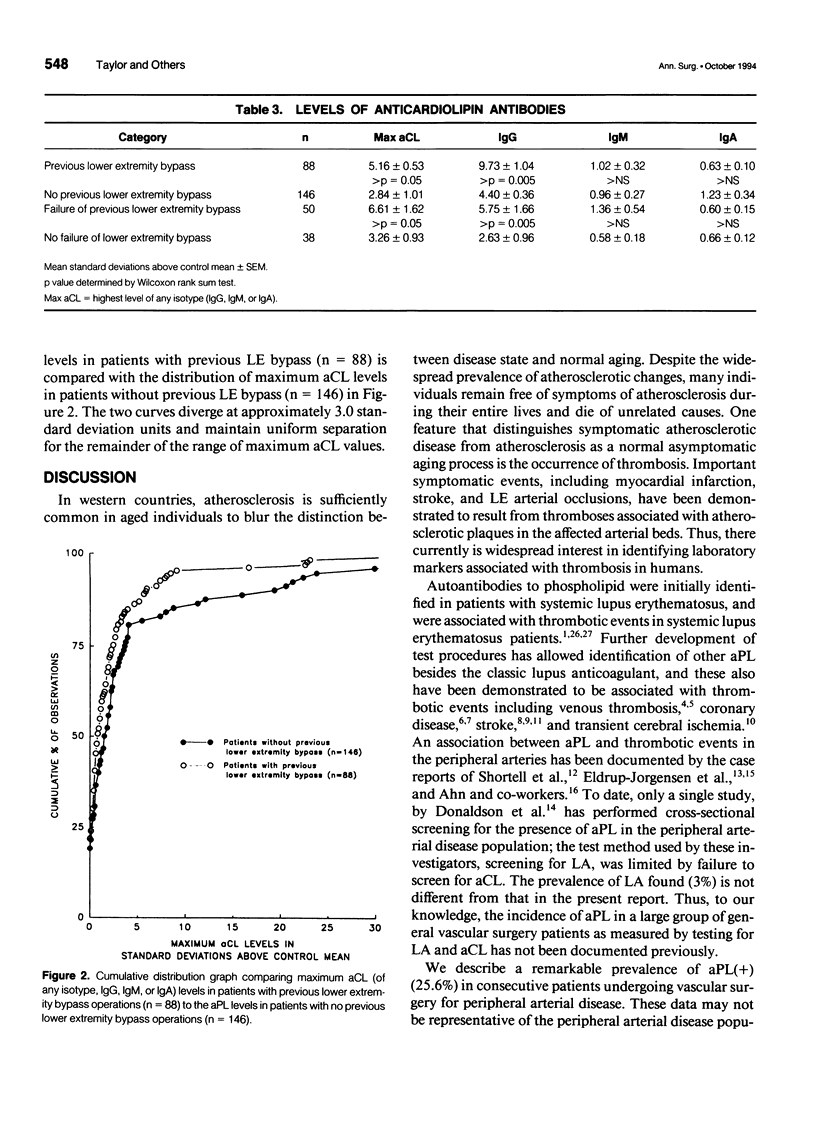
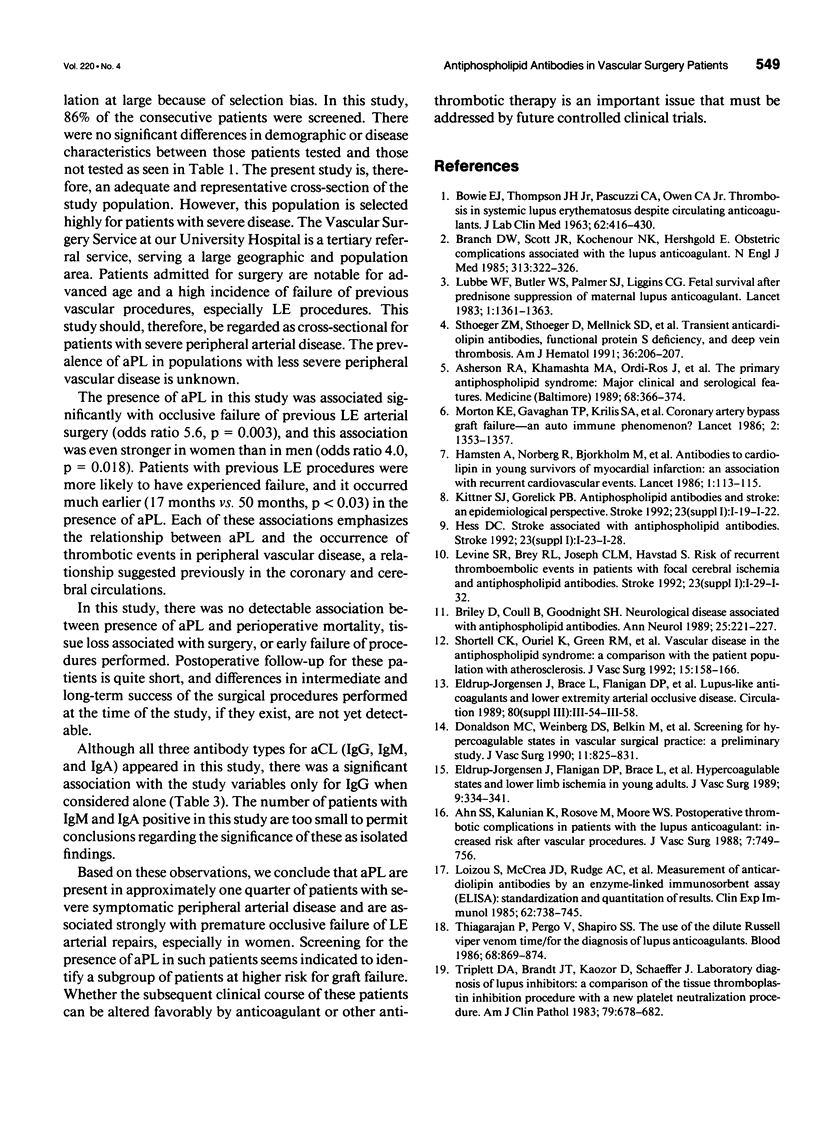
BACKGROUND: Autoantibodies to phospholipid (aPL) have been associated with vascular thromboses in cerebral, coronary, and peripheral venous and arterial sites. To date, no large cross-sectional study has examined the incidence of occurrence of aPL in patients with peripheral arterial disease. METHODS: A cross-sectional study was performed with patients admitted for vascular surgery procedures to treat peripheral arterial disease for 23 months between January 1, 1990 and November 1, 1991. Consecutive patients were evaluated for the presence of aPL. Medical records for each patient were reviewed in detail, and historic, operative, and postoperative parameters were tabulated for relationship to the presence of aPL. RESULTS: Two hundred thirty-four patients underwent complete testing for aPL. All patients were receiving chronic aspirin therapy. This represented 86% of admissions. Antiphospholipid antibodies were detected in 60 patients (26%). No differences in age, sex, operation performed, or postoperative outcome were found between patients with and without aPL. However, patients with aPL were 1.8 times more likely to have undergone previous lower extremity (LE) vascular surgery than patients without aPL (95% confidence interval = 1.0 - 3.6, p = 0.047). Patients with aPL and previous LE vascular surgery were 5.6 times more likely to have had occlusion of that procedure than patients without aPL (95% confidence interval = 1.9 - 16.8, p = 0.03). The occluded previous LE procedures had a shorter duration of patency before occlusion in patients with aPL than in those without (mean duration of patency 17 months vs. 50 months, p < 0.003). Patients with occluded previous LE procedures and aPL were 4 times more likely to be female (95% C.I. = 1.4 - 11.3, p = 0.018). CONCLUSIONS: The incidence of aPL in vascular surgery patients is substantial. Vascular surgery patients with aPL are more likely to have failure of previous LE bypass procedures and to be female and the bypass failure occurs significantly more rapidly than in patients without aPL. Based on these data, testing of vascular surgery patients for aPL and investigation of alternative antithrombotic treatment regimens in patients with aPL appears warranted.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahn S. S., Kalunian K., Rosove M., Moore W. S. Postoperative thrombotic complications in patients with lupus anticoagulant: increased risk after vascular procedures. J Vasc Surg. 1988 Jun;7(6):749–756. doi: 10.1067/mva.1988.avs0070749. [DOI] [PubMed] [Google Scholar]
- Asherson R. A., Chan J. K., Harris E. N., Gharavi A. E., Hughes G. R. Anticardiolipin antibody, recurrent thrombosis, and warfarin withdrawal. Ann Rheum Dis. 1985 Dec;44(12):823–825. doi: 10.1136/ard.44.12.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asherson R. A., Khamashta M. A., Ordi-Ros J., Derksen R. H., Machin S. J., Barquinero J., Outt H. H., Harris E. N., Vilardell-Torres M., Hughes G. R. The "primary" antiphospholipid syndrome: major clinical and serological features. Medicine (Baltimore) 1989 Nov;68(6):366–374. [PubMed] [Google Scholar]
- BOWIE E. J., THOMPSON J. H., Jr, PASCUZZI C. A., OWEN C. A., Jr THROMBOSIS IN SYSTEMIC LUPUS ERYTHEMATOSUS DESPITE CIRCULATING ANTICOAGULANTS. J Lab Clin Med. 1963 Sep;62:416–430. [PubMed] [Google Scholar]
- Briley D. P., Coull B. M., Goodnight S. H., Jr Neurological disease associated with antiphospholipid antibodies. Ann Neurol. 1989 Mar;25(3):221–227. doi: 10.1002/ana.410250303. [DOI] [PubMed] [Google Scholar]
- Dalman R. L., Taylor L. M., Jr, Moneta G. L., Yeager R. A., Porter J. M. Simultaneous operative repair of multilevel lower extremity occlusive disease. J Vasc Surg. 1991 Feb;13(2):211–221. [PubMed] [Google Scholar]
- Donaldson M. C., Weinberg D. S., Belkin M., Whittemore A. D., Mannick J. A. Screening for hypercoagulable states in vascular surgical practice: a preliminary study. J Vasc Surg. 1990 Jun;11(6):825–831. doi: 10.1067/mva.1990.20120. [DOI] [PubMed] [Google Scholar]
- Eldrup-Jorgensen J., Flanigan D. P., Brace L., Sawchuk A. P., Mulder S. G., Anderson C. P., Schuler J. J., Meyer J. R., Durham J. R., Schwarcz T. H. Hypercoagulable states and lower limb ischemia in young adults. J Vasc Surg. 1989 Feb;9(2):334–341. doi: 10.1067/mva.1989.vs0090334. [DOI] [PubMed] [Google Scholar]
- Harris E. N., Gharavi A. E., Boey M. L., Patel B. M., Mackworth-Young C. G., Loizou S., Hughes G. R. Anticardiolipin antibodies: detection by radioimmunoassay and association with thrombosis in systemic lupus erythematosus. Lancet. 1983 Nov 26;2(8361):1211–1214. doi: 10.1016/s0140-6736(83)91267-9. [DOI] [PubMed] [Google Scholar]
- Loizou S., McCrea J. D., Rudge A. C., Reynolds R., Boyle C. C., Harris E. N. Measurement of anti-cardiolipin antibodies by an enzyme-linked immunosorbent assay (ELISA): standardization and quantitation of results. Clin Exp Immunol. 1985 Dec;62(3):738–745. [PMC free article] [PubMed] [Google Scholar]
- Lubbe W. F., Butler W. S., Palmer S. J., Liggins G. C. Fetal survival after prednisone suppression of maternal lupus-anticoagulant. Lancet. 1983 Jun 18;1(8338):1361–1363. doi: 10.1016/s0140-6736(83)92141-4. [DOI] [PubMed] [Google Scholar]
- Morton K. E., Gavaghan T. P., Krilis S. A., Daggard G. E., Baron D. W., Hickie J. B., Chesterman C. N. Coronary artery bypass graft failure--an autoimmune phenomenon? Lancet. 1986 Dec 13;2(8520):1353–1357. doi: 10.1016/s0140-6736(86)92004-0. [DOI] [PubMed] [Google Scholar]
- Shortell C. K., Ouriel K., Green R. M., Condemi J. J., DeWeese J. A. Vascular disease in the antiphospholipid syndrome: a comparison with the patient population with atherosclerosis. J Vasc Surg. 1992 Jan;15(1):158–166. doi: 10.1067/mva.1992.33160. [DOI] [PubMed] [Google Scholar]
- Sthoeger Z. M., Sthoeger D., Mellnick S. D., Steen D., Berrebi A. Transient anticardiolipin antibodies, functional protein S deficiency, and deep vein thrombosis. Am J Hematol. 1991 Mar;36(3):206–207. doi: 10.1002/ajh.2830360309. [DOI] [PubMed] [Google Scholar]
- Taylor L. M., Jr, Edwards J. M., Brant B., Phinney E. S., Porter J. M. Autogenous reversed vein bypass for lower extremity ischemia in patients with absent or inadequate greater saphenous vein. Am J Surg. 1987 May;153(5):505–510. doi: 10.1016/0002-9610(87)90803-8. [DOI] [PubMed] [Google Scholar]
- Taylor L. M., Jr, Hamre D., Dalman R. L., Porter J. M. Limb salvage vs amputation for critical ischemia. The role of vascular surgery. Arch Surg. 1991 Oct;126(10):1251–1258. doi: 10.1001/archsurg.1991.01410340093013. [DOI] [PubMed] [Google Scholar]
- Taylor L. M., Jr, Loboa L., Porter J. M. The clinical course of carotid bifurcation stenosis as determined by duplex scanning. J Vasc Surg. 1988 Sep;8(3):255–261. doi: 10.1067/mva.1988.avs0080255. [DOI] [PubMed] [Google Scholar]
- Thiagarajan P., Pengo V., Shapiro S. S. The use of the dilute Russell viper venom time for the diagnosis of lupus anticoagulants. Blood. 1986 Oct;68(4):869–874. [PubMed] [Google Scholar]
- Triplett D. A., Brandt J. T., Kaczor D., Schaeffer J. Laboratory diagnosis of lupus inhibitors: a comparison of the tissue thromboplastin inhibition procedure with a new platelet neutralization procedure. Am J Clin Pathol. 1983 Jun;79(6):678–682. doi: 10.1093/ajcp/79.6.678. [DOI] [PubMed] [Google Scholar]


