Abstract
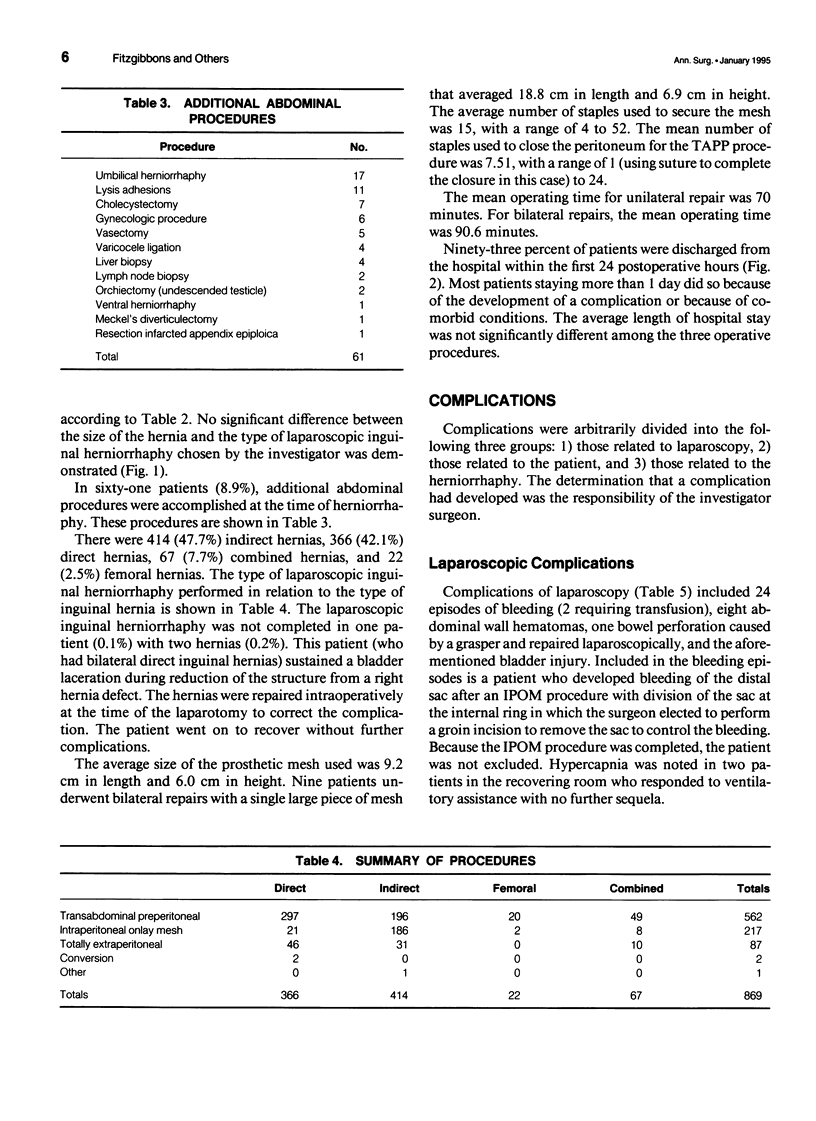
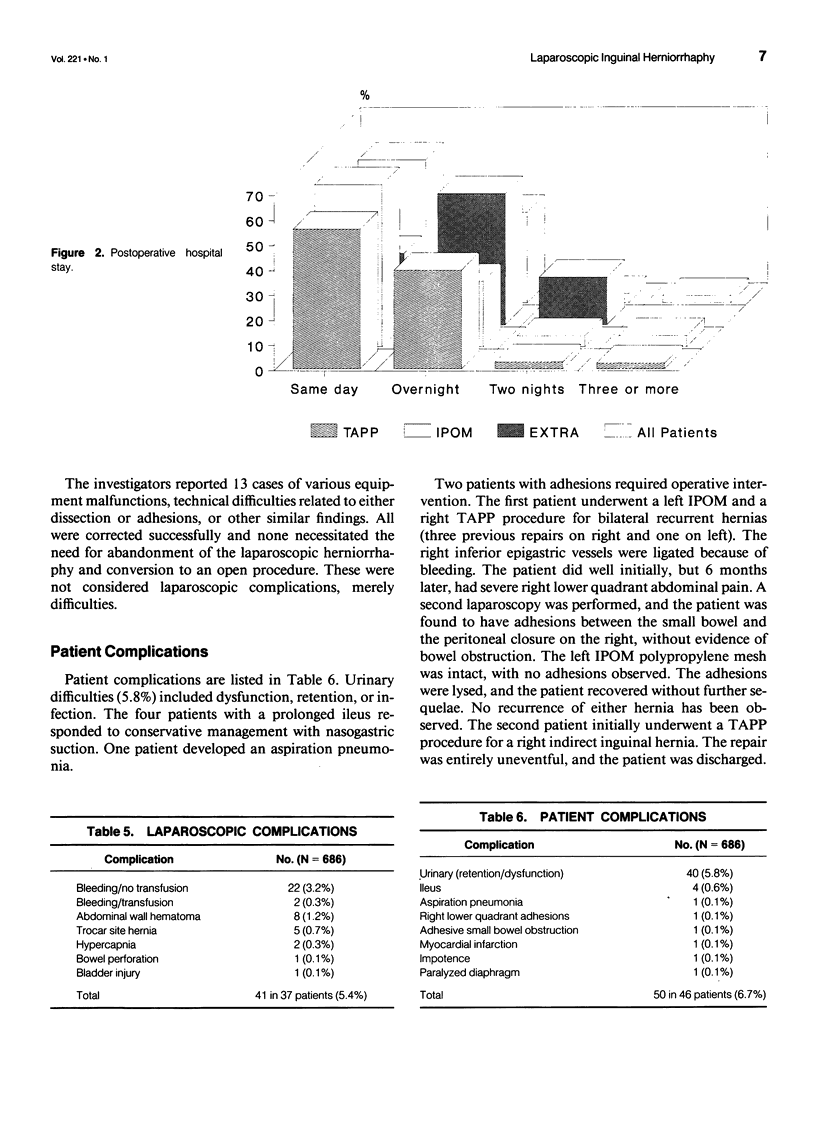
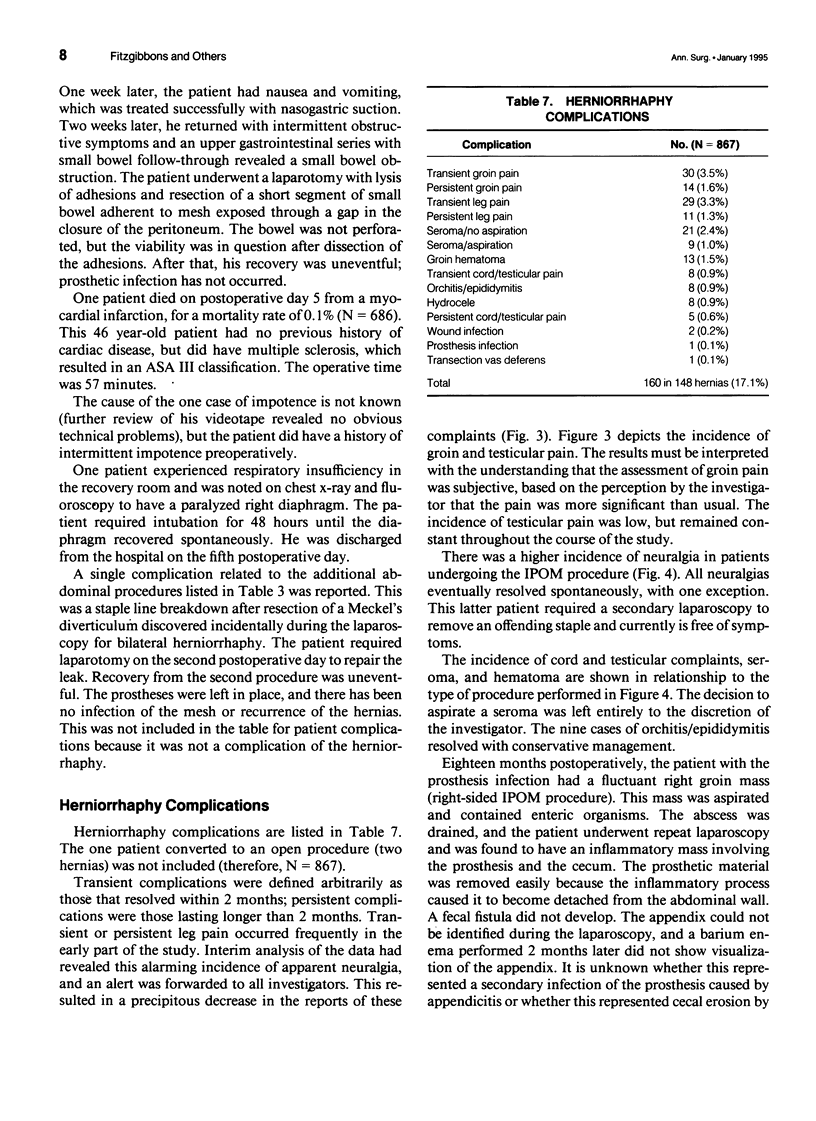
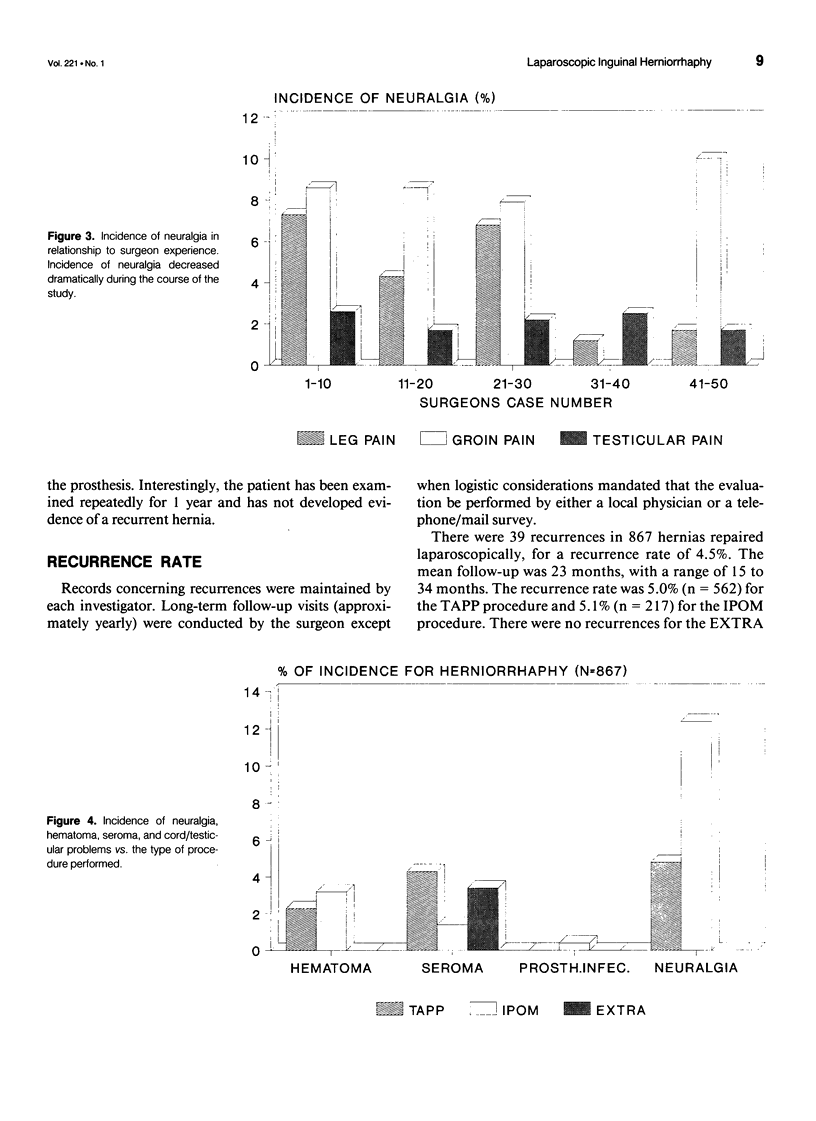
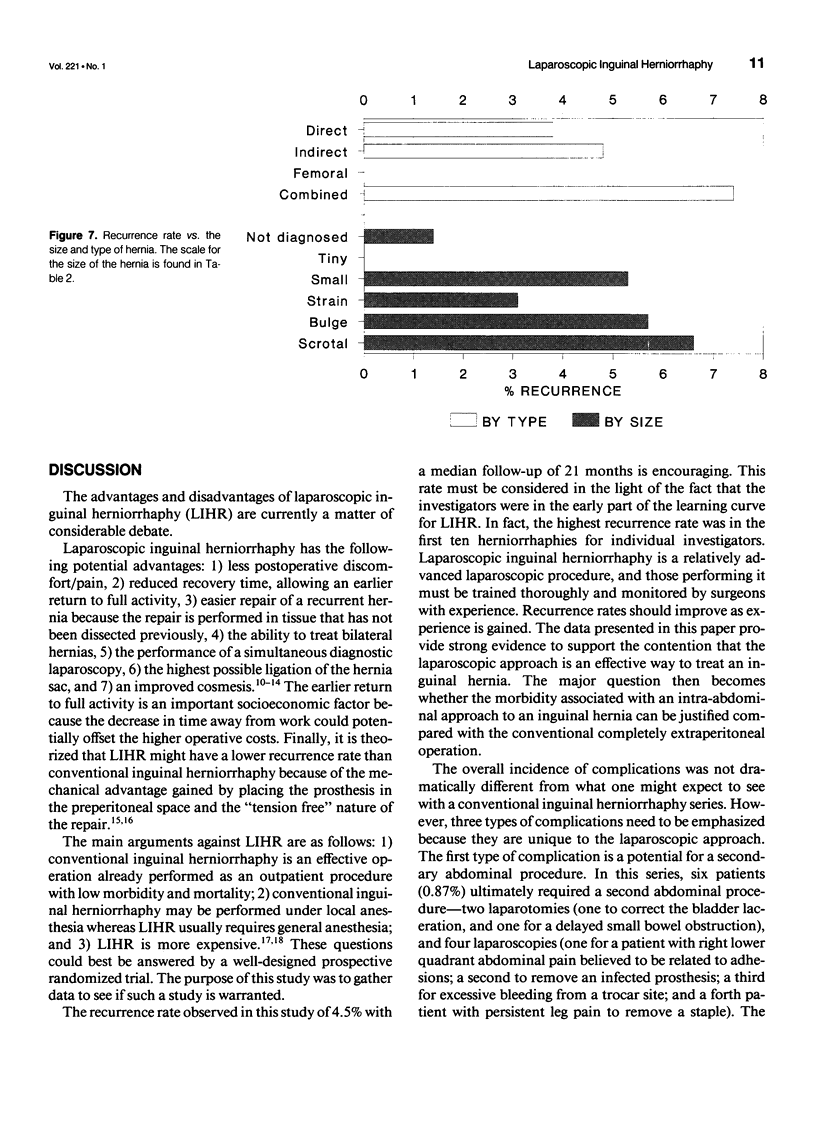
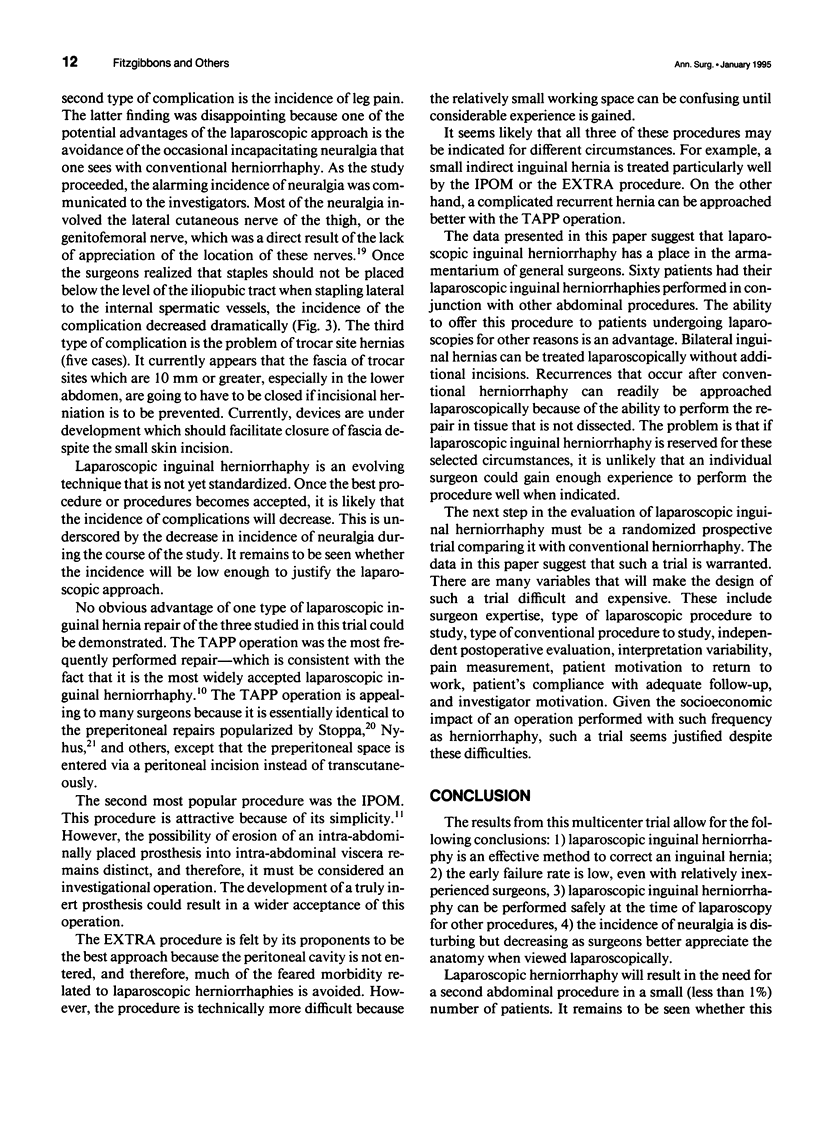
OBJECTIVE: The purpose of this study was to determine if laparoscopic inguinal herniorrhaphy represents a viable alternative to the conventional repair and to assess whether a prospective randomized controlled trial comparing both procedures is warranted. METHODS: Three types of laparoscopic inguinal herniorrhaphies (transabdominal preperitoneal [TAPP], intraperitoneal onlay mesh [IPOM], and totally extraperitoneal [EXTRA]) were studied in a phase II design. Twenty-one investigators from 19 institutions participated. Approval from the local human research committee was required at each institution before patients could be enrolled. RESULTS: There were 686 patients with 869 hernias; 366 (42.1%) were direct, 414 (47.6%) were indirect, 22 (2.5%) were femoral, and 67 (7.7%) were combination hernias. The TAPP procedure was used for 562 hernias, the IPOM was used for 217 hernias, and the EXTRA was used for 87 hernias. Sixty-one patients had additional abdominal procedures performed at the time of laparoscopy without any adverse affects on their herniorrhaphies. The overall recurrence rate was 4.5%, with a minimum follow-up of 15 months. Complications were divided into the following three groups: 1) those related to laparoscopy, 2) those related to the patient, and 3) those related to the herniorrhaphy. Complications related to the laparoscopy occurred in 5.4% of patients; bleeding or abdominal wall hematomas occurred 31 times, (two patients required transfusion); one patient had bowel perforation, which was sutured laparoscopically; a bladder injury required laparotomy for management. Patient complications occurred in 6.7%. The majority involved the urinary tract (5.8%). Two patients required secondary abdominal procedures for adhesions, one for pain in the right lower quadrant and the other for adhesive small bowel obstruction. Postoperative myocardial infarction on day 5 resulted in the only operative mortality, for a rate of 0.1%. Complications related to the herniorrhaphy itself occurred in 17.1%. Most of these were minor, consisting of transient groin pain (3.5%), seroma (3.5%), transient leg pain (3.3%), hematoma (1.5%), or transient cord or testicular problems (0.9%). The incidence of leg pain decreased dramatically as surgeons became more familiar with the anatomy of the nerve supply to the groin when viewed laparoscopically. Ninety-three percent of patients were discharged within 24 hours of their operations. CONCLUSIONS: Laparoscopic inguinal herniorrhaphy is an effective method to correct an inguinal hernia. It can be offered safely to patients undergoing other abdominal procedures. The TAPP, IPOM, and EXTRA procedures appear to be equally effective. A controlled randomized trial is needed to compare this procedure with conventional inguinal herniorrhaphy.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asmussen T., Jensen F. U. A follow-up study on recurrence after inguinal hernia repair. Surg Gynecol Obstet. 1983 Feb;156(2):198–200. [PubMed] [Google Scholar]
- Barnes F. E. Cost-effective hernia repair. Arch Surg. 1993 May;128(5):600–600. doi: 10.1001/archsurg.1993.01420170136024. [DOI] [PubMed] [Google Scholar]
- Cuschieri A. The spectrum of laparoscopic surgery. World J Surg. 1992 Nov-Dec;16(6):1089–1097. doi: 10.1007/BF02067066. [DOI] [PubMed] [Google Scholar]
- Felix E. L., Michas C. Double-buttress laparoscopic herniorrhaphy. J Laparoendosc Surg. 1993 Feb;3(1):1–8. doi: 10.1089/lps.1993.3.1. [DOI] [PubMed] [Google Scholar]
- Filipi C. J., Fitzgibbons R. J., Jr, Salerno G. M., Hart R. O. Laparoscopic herniorrhaphy. Surg Clin North Am. 1992 Oct;72(5):1109–1124. doi: 10.1016/s0039-6109(16)45835-4. [DOI] [PubMed] [Google Scholar]
- Fitzgibbons R. J., Jr, Salerno G. M., Filipi C. J., Hunter W. J., Watson P. A laparoscopic intraperitoneal onlay mesh technique for the repair of an indirect inguinal hernia. Ann Surg. 1994 Feb;219(2):144–156. doi: 10.1097/00000658-199402000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ger R., Mishrick A., Hurwitz J., Romero C., Oddsen R. Management of groin hernias by laparoscopy. World J Surg. 1993 Jan-Feb;17(1):46–50. doi: 10.1007/BF01655704. [DOI] [PubMed] [Google Scholar]
- Ger R., Monroe K., Duvivier R., Mishrick A. Management of indirect inguinal hernias by laparoscopic closure of the neck of the sac. Am J Surg. 1990 Apr;159(4):370–373. doi: 10.1016/s0002-9610(05)81273-5. [DOI] [PubMed] [Google Scholar]
- Lichtenstein I. L., Shulman A. G., Amid P. K. Laparoscopic hernioplasty. Arch Surg. 1991 Dec;126(12):1449–1449. doi: 10.1001/archsurg.1991.01410360019002. [DOI] [PubMed] [Google Scholar]
- McKernan J. B., Laws H. L. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993 Jan-Feb;7(1):26–28. doi: 10.1007/BF00591232. [DOI] [PubMed] [Google Scholar]
- Nyhus L. M. Laparoscopic hernia repair: a point of view. Arch Surg. 1992 Feb;127(2):137–137. doi: 10.1001/archsurg.1992.01420020019002. [DOI] [PubMed] [Google Scholar]
- Nyhus L. M., Pollak R., Bombeck C. T., Donahue P. E. The preperitoneal approach and prosthetic buttress repair for recurrent hernia. The evolution of a technique. Ann Surg. 1988 Dec;208(6):733–737. doi: 10.1097/00000658-198812000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popp L. W. Improvement in endoscopic hernioplasty: transcutaneous aquadissection of the musculofascial defect and preperitoneal endoscopic patch repair. J Laparoendosc Surg. 1991;1(2):83–90. doi: 10.1089/lps.1991.1.83. [DOI] [PubMed] [Google Scholar]
- Rutkow I. M. Laparoscopic hernia repair. The socioeconomic tyranny of surgical technology. Arch Surg. 1992 Nov;127(11):1271–1271. doi: 10.1001/archsurg.1992.01420110013003. [DOI] [PubMed] [Google Scholar]
- Schultz L., Graber J., Pietrafitta J., Hickok D. Laser laparoscopic herniorraphy: a clinical trial preliminary results. J Laparoendosc Surg. 1990;1(1):41–45. doi: 10.1089/lps.1990.1.41. [DOI] [PubMed] [Google Scholar]
- Spaw A. T., Ennis B. W., Spaw L. P. Laparoscopic hernia repair: the anatomic basis. J Laparoendosc Surg. 1991 Oct;1(5):269–277. doi: 10.1089/lps.1991.1.269. [DOI] [PubMed] [Google Scholar]
- Zucker K. A. Perceived future of laparoscopic general surgery. Can J Surg. 1992 Jun;35(3):297–304. [PubMed] [Google Scholar]


