Abstract
Background
Heart failure (HF) remains a major public health burden, necessitating reliable biomarkers for early risk stratification. The triglyceride glucose weight-adjusted waist index (TyG-WWI), a novel metabolic indicator, has emerged as a potential predictor, but its association with HF in the general population remains underexplored.
Methods
This retrospective cross-sectional study included 22,575 participants from the National Health and Nutrition Examination Survey (NHANES) conducted between 1999 and 2018, 704 of whom had HF. The TyG-WWI was calculated, and its association with HF risk was analyzed via multivariable logistic regression (adjusted for demographics, lifestyle factors, disease history, and medication use), restricted cubic splines (with 4 knots), and subgroup analyses. Additionally, interaction tests by different survey cycles were performed to account for temporal effects. ROC analysis with DeLong’s test and net reclassification improvement (NRI) were used to compare the diagnostic performance of the TyG-WWI with that of conventional TyG-related parameters (TyG, TyG-WC, TyG-WHtR) and traditional HF prognostic factors. Sensitivity analyses with multiple imputation for missing data were performed to assess the robustness of the results.
Results
The study population had a mean age of 49.5 years, with 48.34% males. Baseline characteristics differed significantly between the HF and non-HF groups in terms of demographics, lifestyle, disease history, and medication use. After full adjustment for demographic, clinical, and lifestyle factors, each standard deviation increase in the TyG-WWI was associated with a 52% greater HF risk (OR 1.52, 95% CI 1.27–1.81). Restricted cubic spline analysis revealed a linear positive correlation between the TyG-WWI and HF risk. ROC analysis demonstrated that compared with conventional TyG-WWI (AUC = 0.697, 95% CI 0.678–0.715), TyG-WWI exhibited superior discriminative performance for HF diagnosis (TyG: AUC = 0.616; TyG-WC: AUC = 0.665; TyG-WHtR: AUC = 0.673) and traditional prognostic factors (BMI: 0.592; waist circumference: 0.654; fasting blood glucose: 0.524, all DeLong-P < 0.001 after Bonferroni correction). NRI analysis revealed that TyG-WWI provided an 11.41% NRI compared with TyG, 4.20% compared with TyG-WC, and 2.99% compared with TyG-WHtR. Further subgroup analyses revealed that this association was more pronounced in men, patients not using β-blockers, and nondiabetic individuals. Sensitivity analyses reinforced the robustness of the findings.
Conclusion
In the general population, the TyG-WWI is strongly, independently, and dose-dependently associated with heart failure (HF) risk. Notably, its diagnostic performance for HFs surpasses that of traditional TyG-related indices, and it has incremental value as a supplementary parameter to existing TyG-derived metrics. These findings support the use of the TyG-WWI as a promising tool for HF risk stratification with practical clinical utility. However, further validation in large-scale prospective cohorts is warranted to confirm its long-term predictive value and generalizability across diverse populations.
Graphic abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-025-02896-1.
Research insights
What is currently known about this topic?
IR and central obesity are critical metabolic drivers of HF, with their interplay exacerbating cardiac dysfunction.
The TyG index reflects IR and correlates with HF risk, while TyG-WC and TyG-WHtR combine IR with obesity metrics but lack optimization for body weight-adapted adiposity assessment.
TyG-WWI integrates IR and weight-adjusted central obesity, potentially addressing limitations of traditional indices in capturing combined metabolic and adiposity-related HF risk.
What is the key research question?
Does the novel composite index TyG-WWI serve as a valuable supplementary diagnostic tool for HF, with improved reclassification ability beyond traditional TyG-related indices in the general population?
What is new?
TyG-WWI has a strong, independent, linear HF association, more pronounced in men/non-β-blocker/non-diabetic users.
It shows superior discriminative performance for HF compared to traditional TyG-related indices, with significant NRI (NRI: 2.99%–11.41%).
Sensitivity analyses confirm the robustness of these associations, supporting its reliability as a metabolic marker.
How might this study influence clinical practice?
TyG-WWI, a simple supplementary tool to TyG-related parameters with better reclassification, enhances HF risk stratification in primary care/resource-limited settings, aiding precise high-risk identification and targeted prevention.
Introduction
Heart failure (HF) remains a major global health concern, with persistently high morbidity and mortality rates that severely compromise patients’ quality of life and impose a substantial healthcare burden [1, 2]. While established biomarkers such as BNP/NT-proBNP and echocardiographic indices such as the E/e’ ratio (a key parameter for evaluating diastolic function) have significantly advanced HF management [3], their limitations underscore the need for complementary tools. BNP levels are influenced by noncardiac factors (e.g., renal dysfunction and advanced age) [4, 5], and echocardiographic assessments require specialized equipment and expertise, creating barriers in resource-constrained settings. Traditional risk factors, including hypertension, diabetes, and coronary heart disease, are well recognized contributors to HF pathogenesis [6–8]. However, the continued rise in HF incidence despite the control of these factors, coupled with deficiencies in existing diagnostic modalities, highlights the necessity of exploring novel, accessible indicators [2, 9].
In recent years, insulin resistance (IR), a prominent metabolic disorder, has garnered increasing attention for its role in cardiovascular diseases [10–14]. The triglyceride-glucose (TyG) index, a simple and practical surrogate marker for IR [15], is calculated as ln(fasting triglycerides × fasting glucose/2) and has demonstrated potential in predicting cardiovascular disease risk [15–20]. Validated against gold-standard methods such as the hyperinsulinemic-euglycemic clamp and HOMA-IR, the TyG index effectively reflects IR and has been confirmed to be closely associated with the development and progression of various cardiovascular diseases, including coronary heart disease, hypertension, and stroke [21–24]. Indeed, IR contributes to the pathogenesis of all HF subtypes—including heart failure with preserved ejection fraction (HFpEF)—through mechanisms such as myocardial steatosis, systemic inflammation, and endothelial dysfunction [25, 26]. These findings are supported by population-based studies, where multiple investigations have linked the TyG index to the risk and prognosis of various HF subtypes [27–30]. However, the traditional TyG index fails to adequately account for obesity-related factors. Obesity, particularly central obesity, is a key risk factor for IR and is closely linked to multiple cardiometabolic diseases [31–33]. Waist circumference (WC), a marker of central obesity, reflects visceral fat accumulation and systemic inflammation and has been established as an independent risk factor for HF [34, 35] but does not consider the influence of body weight. While body mass index (BMI) has clinical utility in obesity classification, its ability to characterize the complex relationship between fat distribution and metabolic health remains limited [36, 37]. Thus, WC and BMI alone may not fully capture the metabolic‒cardiac interplay in HF risk assessment. The recently developed weight-adjusted waist index (WWI), defined as waist circumference (cm) divided by the square root of body weight (kg), is a novel indicator for evaluating central obesity [38]. By calibrating waist circumference against body weight, WWI enhances stability across diverse populations and improves its capacity to reflect visceral fat accumulation independently of overall body size. Unlike WC, which may overestimate risk in individuals with high muscle mass, or the waist‒to-height ratio (WHTR), which focuses primarily on proportionality without accounting for total adiposity [39], WWI integrates both weight and waist circumference to assess abdominal fat accumulation more accurately [38, 40]. Emerging evidence from multiple studies indicates that WWI is associated with an increased risk of type 2 diabetes and cardiovascular diseases and outperforms traditional indices such as BMI or WC alone in evaluating metabolic disease risk [41–43]. The triglyceride‒glucose-weighted adjusted waist index (TyG-WWI), which combines the TyG index and WWI, was developed to address the limitations of traditional metabolic risk markers by integrating two complementary domains: IR and central obesity. The rationale for this combination lies in their distinct yet synergistic roles: the TyG index captures metabolic dysfunction associated with IR, whereas the WWI quantifies central obesity—a key driver of cardiometabolic inflammation. This integration fills a gap in the literature, where single markers fail to comprehensively assess combined metabolic and obesity-related risks, simultaneously capturing two major drivers of HF progression: metabolic dysfunction and visceral obesity. Research on the associations between the TyG-WWI and cardiovascular diseases remains limited. Huo G et al. explored the relationship between the TyG-WWI and stroke risk [44], whereas Duan C et al. reported in a cohort study that the cumulative TyG-WWI was significantly positively correlated with increased overall cardiovascular disease risk, although no significant association was found between the baseline TyG-WWI and overall cardiovascular disease [45]. Currently, the relationship between the TyG-WWI and HF risk remains unclear.
This study aimed to investigate the association between the TyG-WWI and HF risk via cross-sectional data and to compare the diagnostic value of the TyG-WWI for HF with that of other TyG-related parameters. These findings are expected to provide new insights into the utility of TyG-related parameters in HF risk prediction and prevention.
Methods
Study population
This study employed a retrospective cohort design utilizing data from the National Health and Nutrition Examination Survey (NHANES), which was conducted between 1999 and 2018. The NHANES is a nationwide, continuous survey program administered by the National Center for Health Statistics (NCHS), a subdivision of the Centers for Disease Control and Prevention (CDC). Its primary objective is to assess the health and nutritional status of the U.S. population. The survey adopts a multistage probability sampling method, covering a representative sample of the noninstitutionalized U.S. population.
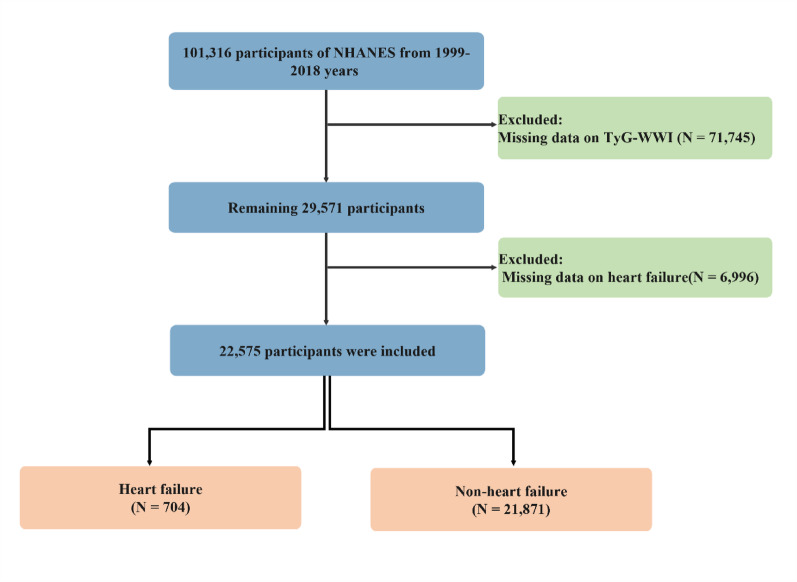
Initially, data for 101,316 participants between 1999 and 2018 were extracted from the NHANES database. To ensure data integrity and validity, certain participants were excluded on the basis of the following criteria: (1) missing triglyceride‒glucose waist‒to‒weight adjusted index (TyG‒WWI) data (n = 71,745) and (2) missing HF diagnosis data (n = 6996). After this screening process, a total of 22,575 eligible participants were included in the study. Among these, 704 participants were identified as having heart failure according to its definition. The entire screening process for the study population strictly adhered to NHANES data usage guidelines and ethical standards. A detailed flowchart of the study population screening is presented in Fig. 1.
Fig. 1.
Study population screening flowchart. The NHANES data were screened on the basis of the study design to select eligible participants
Definitions of outcomes
In this study, the diagnosis of heart failure was primarily based on participants’ responses to specific questions in a questionnaire survey. Specifically, we used the following question to identify cases of heart failure: “Has a doctor ever told you that you have congestive heart failure?” Participants who answered “yes” to this question were defined as having heart failure. This self-reported method of diagnosing heart failure has been widely used in previous studies on the basis of NHANES data [46, 47].
Definition of the TyG-WWI
The triglyceride‒glucose weight‒adjusted waist circumference index (TyG-WWI) is an indicator used to evaluate insulin resistance. The formula for calculating the TyG-WWI is as follows: waist circumference (cm)/√(weight (kg)) * ln(fasting triglyceride (mg/dL) * fasting glucose (mg/dL)/2). The data for waist circumference and weight were extracted directly from the body measurement section of the NHANES database. Similarly, the fasting triglyceride and fasting glucose data, which are actual measured values obtained from participants during fasting, are also sourced from the NHANES database.
Covariates
To control for potential confounding factors, this study included a range of covariates, specifically demographic characteristics: age (continuous variable); sex (male/female); ethnicity (including Hispanic White and Black, Mexican, and other ethnicities); education (categorized as less than high school, high school or equivalent, and college or above); and marital status (married/living with a partner, widowed/divorced/separated, never married). Socioeconomic status: Poverty income ratio (PIR, the ratio of family income to the poverty line, with PIR categories defined as follows: low: PIR < 1.35, medium: 1.35 ≤ PIR < 3.0, high: ≥ 3.0). Lifestyle factors: Drinking status (never, former, and current drinking (categorized as mild, moderate, and heavy)); smoking status (never, former, and current smoking); height (continuous variable, in centimeters); weight (continuous variable, in kilograms). Body mass index (BMI) was calculated as weight (measured to the nearest 0.1 kg via calibrated electronic scales) divided by height squared (measured to the nearest 0.1 cm via portable stadiometers) in fasting participants, with all measurements performed by trained medical personnel following standardized protocols. Fasting blood glucose (FBG) and triglyceride (TG) levels were obtained from venous blood samples collected after an overnight fast of at least 8 h at the Mobile Examination Center (MEC) as part of the NHANES protocol. The estimated glomerular filtration rate (eGFR) was calculated via the 2009 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, which incorporates serum creatinine, age, sex, and race/ethnicity [48]. Total physical activity (PA) time was self-reported by participants via the Global Physical Activity Questionnaire (GPAQ) developed by the World Health Organization. This questionnaire assesses PA across different domains, including occupational, transportation, and leisure-time activities, with detailed assessment protocols available at the website [49]. Following WHO analysis guidelines, each participant’s PA was converted to weekly metabolic equivalent (MET) minutes of moderate-to-vigorous intensity activity. MET values vary by activity type, with reference values for each PA category provided in the NHANES. PA scores were calculated via the following formula: MET value × weekly frequency × duration per activity session, integrating activity type, frequency, and duration [50].
Medication use information from the NHANES was collected through in-person interviews where participants were asked to report all prescription medications they had taken in the past 30 days, including product names and dosages, with additional verification using medication containers when available. In the present study, β-blocker use was defined as self-reported use of any of the following agents: metoprolol (succinate, tartrate, or unspecified), atenolol (including combinations with chlorthalidone), bisoprolol (including combinations with hydrochlorothiazide), propranolol hydrochloride, nadolol, timolol (including ophthalmic formulations and combinations with dorzolamide), acebutolol hydrochloride, labetalol hydrochloride, betaxolol (including ophthalmic formulations), carvedilol, sotalol, nebivolol, or combinations of metoprolol with hydrochlorothiazide. ACEI/ARB use was defined as self-reported use of any of the following: quinapril hydrochloride, enalapril maleate (including combinations with hydrochlorothiazide), lisinopril (including combinations with hydrochlorothiazide), benazepril hydrochloride (including combinations with hydrochlorothiazide or amlodipine), captopril (including combinations with hydrochlorothiazide), fosinopril sodium, ramipril, perindopril (including combinations with amlodipine), irbesartan (including combinations with hydrochlorothiazide), valsartan (including combinations with hydrochlorothiazide or amlodipine and triple combinations with amlodipine and hydrochlorothiazide), candesartan cilexetil, losartan potassium (including combinations with hydrochlorothiazide), telmisartan (including combinations with hydrochlorothiazide), or combinations of quinapril with hydrochlorothiazide.
Medical history: Coronary heart disease (CHD) history (yes/no) was determined through the following questionnaire: “Has a doctor or other health professional ever told you that you had coronary heart disease?” [51] Hypertension history (yes/no) was based on physician diagnosis, records of antihypertensive medication use, and two nonconsecutive blood pressure readings exceeding diagnostic criteria [52]. Participants were categorized into glucose metabolism groups on the basis of predefined criteria: diabetes mellitus (DM) was diagnosed if participants reported a doctor’s diagnosis of diabetes, had glycated hemoglobin (HbA1c) ≥ 6.5%, fasting glucose ≥ 7.0 mmol/L, random blood glucose ≥ 11.1 mmol/L, two-hour OGTT blood glucose ≥ 11.1 mmol/L, or were using diabetes medication or insulin; impaired fasting glycemia (IFG) was defined as fasting glucose ≥ 6.1 mmol/L but < 7.0 mmol/L; impaired glucose tolerance (IGT) was defined as two-hour OGTT blood glucose ≥ 7.8 mmol/L but < 11.1 mmol/L; and normal glucose status was assigned to those not meeting the above criteria [53]. Metabolic syndrome was diagnosed per ATP III criteria (≥ 3 of waist circumference ≥ 102 cm [men]/ ≥ 88 cm [women], TG ≥ 1.7 mmol/L or lipid-lowering therapy, HDL-C < 1.03 mmol/L [men]/ < 1.29 mmol/L [women], FBG ≥ 6.1 mmol/L or treated diabetes, blood pressure ≥ 130/85 mmHg or antihypertensive therapy) [54]. The Charlson Comorbidity Index was calculated from self-reported conditions with predefined weights, with independent extraction by two researchers and discrepancies resolved via third-party review [55]. All analyses adhered to NHANES standardized procedures, with data quality ensured through CLIA-certified internal and external quality controls.
Statistical analysis
This study employed the NHANES complex sampling weighting method to ensure the representativeness and accuracy of the results. We conducted weighting according to the official NHANES guidelines, using Mobile Examination Center (MEC) weights (variable names: wtmec2yr and wtmec4yr) to correct for sampling probability, nonresponse, and poststratification, thereby ensuring the representativeness of the results for the noninstitutionalized civilian population in the United States. These weights were incorporated into the regression model via the survey package in R software to account for the clustering and stratification effects inherent in the sampling design.
To compare differences in baseline characteristics between groups, survey weighting methods were used, with weighted linear regression models for continuous variables and weighted chi-square tests for categorical variables. Weighted logistic regression analysis was conducted to evaluate the association between the TyG-WWI and the risk of heart failure. To control for potential confounding factors, we constructed three progressively adjusted multivariable weighted logistic regression models: the crude model without any adjustments; Model I adjusted for age, sex, ethnicity, education, marital status, and PIR; and Model II further adjusted for drinking status, smoking status, eGFR, PA, β-blocker use, ACEI/ARB use, CHD history, hypertension history, and blood glucose status based on Model I. Notably, the TyG-WWI was analyzed both as a continuous variable and by quartile grouping, with a trend test performed to evaluate the potential dose‒response relationship. To explore temporal trends in the association between the TyG-WWI and heart failure over the 20-year study period (1999–2018), supplementary analyses were conducted across five 4-year intervals. These analyses followed the same model adjustment strategies as described above.
Before constructing the multivariate model, we checked for multicollinearity between the TyG-WWI and other variables by calculating the generalized variance inflation factor (GVIF). If GVIF^ (1/2Df) was equal to or greater than 2 (Df, degrees of freedom), the variable was considered to be significantly multicollinear [56]. Importantly, we did not find any covariates with significant multicollinearity (Supplementary Table S2).
The more flexible dose‒response relationship between the TyG-WWI and heart failure was explored via RCS with adjustments for all variables in Model II. The RCS analysis was performed via the rcs function from the rms package in conjunction with the svyglm function (from the survey package), incorporating NHANES sampling weights, stratification, and clustering to account for design effects. Four knots were placed at the 10th, 30th, 70th, and 90th percentiles of the TyG-WWI. Owing to widened confidence intervals for TyG-WWI values > 140 (potentially affecting fit reliability), participants with TyG-WWI > 140 were excluded from the primary analysis. The RCS fitting results for the original data (including all participants) are presented in Supplementary Figure S1. To further investigate possible interactions, we conducted subgroup analyses stratified by age, sex, ethnicity, education level, marital status, PIR, drinking status, smoking status, metabolic syndrome, β-blocker use, ACEI/ARB use, CHD history, hypertension history, and blood glucose status to evaluate the heterogeneity of the associations between the TyG-WWI and heart failure in different populations. Furthermore, to assess the clinical value of the TyG-WWI in diagnosing heart failure, receiver operating characteristic (ROC) curves were used to evaluate the diagnostic performance of the TyG-WWI, TyG-related indices (TyG, TyG-WC, TyG-WHtR), and traditional heart failure risk factors (BMI, WC, WHtR, FPG, HbA1c, TG, LDL-C, and CRP). The DeLong test was applied to compare differences in diagnostic ability, with the Bonferroni correction used to adjust for multiple comparisons; for comparisons with TyG-related indices, the significance level was set at 0.0167 (0.05 divided by 3 comparisons), and for comparisons with traditional risk factors, it was set at 0.00625 (0.05 divided by 8 comparisons). Additionally, net reclassification improvement (NRI) analysis was performed to quantify the incremental predictive value of the TyG-WWI beyond conventional TyG-related parameters.
Sensitivity analyses were conducted to evaluate the potential impact of missing data on the results. Among the variables included in the analysis, only age, sex, and ethnicity had no missing values; all other variables (education, marital status, PIR, drinking status, smoking status, eGFR, PA, β-blocker use, ACEI/ARB use, CHD history, hypertension history, and blood glucose status) contained missing values and underwent multiple imputation. To handle these missing data, multiple imputation by chained equations (MICE) was employed, a method that models each variable with missing values on the basis of other variables in the dataset, including demographic characteristics, lifestyle factors, clinical indicators, and disease history. This process generated three complete imputed datasets. Logistic regression analyses were repeated on each of these imputed datasets, with quartile grouping and trend tests performed consistently with the original model. Additionally, sensitivity analyses were performed to assess the robustness of the findings, including excluding extreme values of the TyG-WWI (defined as values greater than 140) and further adjusting for potential confounding factors such as sleep apnea syndrome and atrial fibrillation history in the regression models, with quartile grouping and trend tests also conducted in line with the original analytical approach.
All analyses were performed via R software versions 4.2.1 and Free Statistics software versions 2.1, and a P value less than 0.05 was considered statistically significant.
Results
Characteristics of the included and excluded patients
On the basis of the study design, a total of 78,741 participants were excluded because of missing data on key variables (the exposure TyG-WWI and the outcome HF) from the initial 101,316 participants in NHANES 1999–2018 (Fig. 1). Given the high proportion of exclusions due to missing data, we compared baseline characteristics between the included cohort (n = 22,575) and the excluded group (n = 78,741) (Supplementary Table S1). Significant differences were observed in multiple variables: the excluded group was older (65.54 vs. 46.70 years), had a higher BMI (30.96 vs. 28.63 kg/m2), waist circumference (107.87 vs. 98.19 cm), TyG (8.96 vs. 8.62), and TyG-WWI (104.30 vs. 94.14), and a higher Charlson comorbidity index (3.56 vs. 0.81) (all p < 0.001). Additionally, the excluded group had a greater proportion of males (55.26% vs. 48.11%), non-Hispanic White individuals (54.55% vs. 44.46%), former drinkers (37.26% vs. 17.07%), and individuals with metabolic syndrome (71.23% vs. 34.99%) or coronary heart disease (39.26% vs. 2.91%) (all p < 0.001). In contrast, no significant differences were noted in height, fasting blood glucose, eGFR, education level, marital status, ACEI/ARB use, or other variables (p > 0.05).
Baseline characteristics of the study participants
The baseline characteristics of the participants stratified by HF status are presented in Table 1. Among 22,575 participants, 704 (3.1%) had HF. Compared with non-HF participants, those with HF were significantly older (65.54 vs. 46.70), heavier (87.39 vs. 82.01), and had larger waist circumferences (107.87 vs. 98.19) and higher BMIs (30.96 vs. 28.63 kg/m2, p < 0.001). Metabolic parameters revealed that HF participants had higher TyG (8.96 vs. 8.62) and TyG-WWI (104.30 vs. 94.14) values, whereas fasting blood glucose (6.11 vs. 5.85) and eGFR (101.99 vs. 103.05) did not differ significantly. Sex and ethnicity distributions differed significantly (both p < 0.001). Cardiovascular risk profiles revealed that HF participants had a greater Charlson Comorbidity Index, with a significantly greater incidence of coronary heart disease, hypertension, metabolic syndrome, and diabetes mellitus (all p < 0.05). Medication use differed significantly for β-blockers (p < 0.001) but not for ACEIs/ARBs (p = 0.310). Lifestyle factor data revealed that HF participants had lower physical activity scores and were more likely to be former smokers and drinkers (all p < 0.05). Socioeconomic indicators revealed marginal differences in the poverty income ratio (p = 0.015) but no significant variation in education level or marital status (p > 0.05). These results indicate significant differences in baseline characteristics between HF and non-HF individuals across demographic, clinical, and behavioral domains.
Table 1.
Baseline characteristics of participants stratified by the presence of HF
| Non-HF | HF | P value | |
|---|---|---|---|
| Participants | 21,871 | 704 | |
| Age, years | 46.70 (0.22) | 65.54 (0.65) | < 0.001 |
| Weight, kg | 82.01 (0.22) | 87.39 (1.25) | < 0.001 |
| Height, m | 168.99 (0.09) | 167.66 (0.54) | 0.075 |
| WC, cm | 98.19 (0.20) | 107.87 (0.93) | < 0.001 |
| BMI, kg/m2 | 28.63 (0.08) | 30.96 (0.40) | < 0.001 |
| FBG, mmol/L | 5.85 (0.03) | 6.11 (0.19) | 0.166 |
| eGFR | 103.05 (0.28) | 101.99 (1.94) | 0.588 |
| PA-Scores | 3400.63 (70.69) | 2575.11 (352.84) | 0.021 |
| CCI | 0.81 (0.01) | 3.56 (0.09) | < 0.001 |
| TyG | 8.62 (0.66) | 8.96 (0.73) | < 0.001 |
| TyG-WWI | 94.14 (0.15) | 104.30 (0.59) | < 0.001 |
| Sex | < 0.001 | ||
| Female | 11,348 (51.89%) | 315 (44.74%) | |
| Male | 10,523 (48.11%) | 389 (55.26%) | |
| Ethnicity | < 0.001 | ||
| Non-Hispanic White | 9723 (44.46%) | 384 (54.55%) | |
| Non-Hispanic Black | 4291 (19.62%) | 153 (21.73%) | |
| Mexican American | 3969 (18.15%) | 79 (11.22%) | |
| Other races | 3888 (17.78%) | 88 (12.50%) | |
| Education | 0.365 | ||
| Below high school | 5256 (28.84%) | 151 (26.54%) | |
| High school or equivalent | 6365 (34.92%) | 213 (37.43%) | |
| Above high school | 6606 (36.24%) | 205 (36.03%) | |
| Marital status | 0.712 | ||
| Married/cohabiting | 7077 (53.57%) | 233 (55.61%) | |
| Widowed/divorced/separated | 2683 (20.31%) | 81 (19.33%) | |
| Never married | 3450 (26.12%) | 105 (25.06%) | |
| PIR | 0.015 | ||
| Low | 7842 (39.49%) | 231 (36.26%) | |
| Medium | 5862 (29.52%) | 222 (34.85%) | |
| High | 6153 (30.99%) | 184 (28.89%) | |
| Smoking status | < 0.001 | ||
| Never | 11,873 (54.34%) | 287 (40.77%) | |
| Former | 5433 (24.86%) | 275 (39.06%) | |
| Now | 4544 (20.80%) | 142 (20.17%) | |
| Drinking status | < 0.001 | ||
| Never | 2817 (14.07%) | 92 (14.47%) | |
| Former | 3417 (17.07%) | 237 (37.26%) | |
| Mild | 6757 (33.75%) | 199 (31.29%) | |
| Moderate | 2986 (14.91%) | 45 (7.08%) | |
| Heavy | 4044 (20.20%) | 63 (9.91%) | |
| Metabolic syndrome | < 0.001 | ||
| No | 13,800 (65.01%) | 202 (28.77%) | |
| Yes | 7428 (34.99%) | 500 (71.23%) | |
| β-blockers use | < 0.001 | ||
| No | 20,691 (94.67%) | 622 (88.48%) | |
| Yes | 1165 (5.33%) | 81 (11.52%) | |
| ACEI/ARB use | 0.310 | ||
| No | 21,222 (97.10%) | 678 (96.44%) | |
| Yes | 634 (2.90%) | 25 (3.56%) | |
| Hypertension history | 0.036 | ||
| No | 11,838 (70.33%) | 353 (66.10%) | |
| Yes | 4994 (29.67%) | 181 (33.90%) | |
| CHD history | < 0.001 | ||
| No | 21,188 (97.09%) | 413 (60.74%) | |
| Yes | 636 (2.91%) | 267 (39.26%) | |
| Blood glucose status | < 0.001 | ||
| Normal | 14,155 (66.68%) | 241 (34.33%) | |
| DM | 3862 (18.19%) | 355 (50.57%) | |
| IFG | 1983 (9.34%) | 67 (9.54%) | |
| IGT | 1228 (5.78%) | 39 (5.56%) |
HF, heart failure; WC, waist circumference; BMI, body mass index; FBG, fasting blood glucose; eGFR, estimated glomerular filtration rate; PA, physical activity; CCI, Charlson comorbidity index; TyG, triglyceride glucose; TyG-WWI, triglyceride glucose weight adjusted waist index; PIR, poverty income ratio; ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor blocker; CHD, coronary heart disease; DM, diabetes mellitus; IFG, impaired fasting glucose; IGT, Impaired glucose tolerance
Associations between the TyG-WWI and HF risk
Table 2 presents the results of logistic regression analyses examining the association between the TyG-WWI and HF across progressively adjusted models. In the crude model, each standard deviation increase in the TyG-WWI was associated with 2.17-fold greater odds of HF (95% CI 2.00–2.35). This association remained statistically significant after adjustment for demographic factors in Model I (OR 1.76, 95% CI 1.56–1.99) and further attenuated but persisted after comprehensive multivariable adjustment in Model II (OR 1.47, 95% CI 1.16–1.87). When analyzed by quartiles, a clear dose‒response relationship was observed (p-trend < 0.01 in all models). In the fully adjusted Model II, compared with those in the lowest quartile (Q1), the odds ratios for HF in Q2, Q3, and Q4 were 2.36 (95% CI 1.15–4.83), 2.21 (95% CI 1.01–4.79), and 3.97 (95% CI 1.85–8.54), respectively. These findings confirm that the TyG-WWI has an independent, graded association with HF risk, with the strength of the association decreasing but remaining significant with increasing covariate adjustment, particularly in the highest quartile.
Table 2.
Logistic regression analyses for the associations between the TyG-WWI and HF in different models
| Exposure | OR (95%CI) | ||
|---|---|---|---|
| Crude model | Model I | Model II | |
| TyG-WWI (per SD) | 2.17 (2.00, 2.35) | 1.76 (1.56, 1.99) | 1.47 (1.16, 1.87) |
| TyG-WWI | |||
| Q1 | 1.0(Ref) | 1.0(Ref) | 1.0(Ref) |
| Q2 | 2.78 (1.78, 4.37) | 1.45 (0.86, 2.44) | 2.36 (1.15, 4.83) |
| Q3 | 4.58 (3.12, 6.73) | 1.89 (1.18, 3.04) | 2.21 (1.01, 4.79) |
| Q4 | 11.03 (7.42, 16.42) | 3.77 (2.32, 6.12) | 3.97 (1.85, 8.54) |
| p-trend | < 0.01 | < 0.01 | < 0.01 |
OR, odds ratio; SD, standard deviation. Other abbreviations are listed in Table 1
Crude model adjusted for: none
Model I adjusts for age, sex, ethnicity, education, marital status and PIR
The Model II model adjusts for age, sex, ethnicity, education, marital status, PIR, drinking status, smoking status, eGFR, PA, β-blocker use, ACEI/ARB use, CHD, hypertension and blood glucose status
Dose‒response relationship between the TyG-WWI and HF
The dose‒response relationship between the TyG-WWI and HF risk is illustrated in Fig. 2 (after excluding outliers with a TyG-WWI > 140). This RCS analysis, adjusted for all variables in Model II and incorporating NHANES sampling weights, stratification, and clustering, revealed a significant positive association (P for overall effect = 0.003). The trend was nearly linear with no evidence of significant nonlinearity (P for nonlinearity = 0.522), indicating that HF risk increases continuously as TyG-WWI levels rise within the physiological range, without distinct threshold effects. This pattern aligns with the quartile-based findings, reinforcing that the TyG-WWI acts as a graded risk indicator for HF in the study population after extreme values are excluded. On the basis of the RCS analysis of the original data (Supplementary Figure S1), which included all participants regardless of TyG-WWI values, the overall association between the TyG-WWI and HF risk remained significant (P for overall effect = 0.004). Although the confidence intervals widened for TyG-WWI values > 140, suggesting potential instability in the fit for extreme values, the nonlinear test still showed no strong evidence of deviation from linearity (P for nonlinearity = 0.228). This consistency between the original and outlier-excluded analyses supports the robustness of the positive dose‒response relationship between the TyG-WWI and HF risk .
Fig. 2.
Dose‒response relationship between the TyG-WWI and HF. Restricted cubic spline adjusted for age, sex, ethnicity, education, marital status, PIR, drinking status, smoking status, eGFR, PA, β-blocker use, ACEI/ARB use, CHD, hypertension and blood glucose status. Abbreviations: OR: odds ratio. Other abbreviations are listed in Table 1
Subgroup analysis of the association between the TyG-WWI and HF
Subgroup analyses revealed significant interactions for sex, β-blocker use, and blood glucose status (all P-interaction < 0.05), whereas no significant interaction was detected for age (P-interaction = 0.30). In terms of sex, the association between the TyG-WWI and HF risk was significant in males (OR 1.61, 95% CI 1.25–2.07) but not in females (OR 1.11, 95% CI 0.84–1.47). For β-blocker use, the association was evident in participants not using β-blockers (OR 1.43, 95% CI 1.16–1.76) but not in those using β-blockers (OR 0.67, 95% CI 0.34–1.32). With respect to blood glucose status, the association was strongest in participants with normal blood glucose (OR 2.07, 95% CI 1.45–2.95), followed by prediabetes (OR 1.64, 95% CI 0.95–2.82), and was not significant in those with diabetes mellitus (OR 1.05, 95% CI 0.80–1.37). No significant interactions were observed in ethnicity, education, marital status, PIR, drinking status, smoking status, metabolic syndrome, ACEI/ARB use, CHD history, or hypertension history (all P-interaction > 0.05), with consistent positive associations between TyG-WWI and HF risk across these subgroups (Table 3).
Table 3.
Association between the TyG-WWI and HF stratified by age, sex, ethnicity, education, marital status, PIR, drinking status, smoking status, metabolic syndrome, β-blocker use, ACEI/ARB use, CHD, hypertension and blood glucose status
| Subgroup | Adjusted OR (95%CI) | P-interaction |
|---|---|---|
| Age | 0.30 | |
| < 60 years | 1.57 (1.20, 2.07) | |
| ≥ 60 years | 1.30 (1.02, 1.66) | |
| Sex | 0.04 | |
| Female | 1.11 (0.84, 1.47) | |
| Male | 1.61 (1.25, 2.07) | |
| Ethnicity | 0.74 | |
| Non-Hispanic White | 1.45 (1.11, 1.89) | |
| Non-Hispanic Black | 1.32 (0.93, 1.88) | |
| Mexican American | 1.04 (0.61, 1.79) | |
| Other races | 1.40 (0.82, 2.38) | |
| Education | 0.38 | |
| Below high school | 1.14 (0.73, 1.80) | |
| High school or equivalent | 1.25 (0.93, 1.68) | |
| Above high school | 1.54 (1.17, 2.03) | |
| Marital status | 0.82 | |
| Married/cohabiting | 1.42 (1.10, 1.83) | |
| Widowed/divorced/separated | 1.37 (0.90, 2.08) | |
| Never married | 1.25 (0.89, 1.75) | |
| PIR | 0.58 | |
| Low | 1.30 (0.93, 1.82) | |
| Medium | 1.51 (1.14, 2.02) | |
| High | 1.24 (0.90, 1.71) | |
| Drinking status | 0.26 | |
| Current | 1.49 (1.16, 1.90) | |
| Never/past | 1.22 (0.92, 1.62) | |
| Smoking status | 0.82 | |
| Current | 1.40 (0.96, 2.04) | |
| Never/past | 1.34 (1.07, 1.66) | |
| Metabolic syndrome | 0.18 | |
| No | 1.53 (1.02, 2.30) | |
| Yes | 1.11 (0.85, 1.44) | |
| β-blockers use | 0.03 | |
| No | 1.43 (1.16, 1.76) | |
| Yes | 0.67 (0.34, 1.32) | |
| ACEI/ARB use | 0.85 | |
| No | 1.38 (1.14, 1.68) | |
| Yes | 1.26 (0.47, 3.34) | |
| CHD history | 0.72 | |
| No | 1.39 (1.11, 1.73) | |
| Yes | 1.29 (0.90, 1.85) | |
| Hypertension history | 0.65 | |
| No | 1.41 (1.09, 1.82) | |
| Yes | 1.31 (0.99, 1.71) | |
| Blood glucose status | < 0.01 | |
| Normal | 2.07 (1.45, 2.95) | |
| DM | 1.05 (0.80, 1.37) | |
| Prediabetes | 1.64 (0.95, 2.82) |
All abbreviations are listed in Table 1
Comparison of the TyG-WWI with conventional TyG-related parameters and traditional prognostic factors for heart failure diagnosis
ROC curve analysis (Fig. 3) revealed that the TyG-WWI has diagnostic value for HF, with an area under the curve (AUC) of 0.696 (95% CI 0.678–0.715) and an optimal diagnostic threshold of 98.93. Further comparative ROC analyses (Table 4 and Fig. 4) confirmed that the TyG-WWI had the highest AUC (0.697, 95% CI 0.678–0.715) for heart failure diagnosis among all evaluated indices. Compared with conventional TyG-related parameters, the TyG-WWI exhibited significantly superior discriminative performance (all DeLong-P < 0.001 after Bonferroni correction), with AUC values of 0.616 for TyG, 0.665 for TyG-WC, and 0.673 for TyG-WHtR. Moreover, NRI analysis revealed that the TyG-WWI provided an 11.41% NRI over TyG, a 4.20% NRI over TyG-WC, and a 2.99% NRI over TyG-WHtR. Additionally, supplementary analyses compared with traditional heart failure prognostic factors (Table S4) revealed that the TyG-WWI outperformed obesity-related indices (BMI: 0.592; WC: 0.654; WHtR: 0.604), glucose metabolism markers (fasting plasma glucose: 0.524; HbA1c: 0.518), lipid profiles (TG: 0.497; LDL-C: 0.510), and inflammatory markers (CRP: 0.505), with all DeLong-P values < 0.0001 after Bonferroni correction (0.00625).
Fig. 3.
ROC curve of the TyG-WWI for the diagnosis of HF. Abbreviations: ROC: receiver operating characteristic; AUC: area under the curve. Other abbreviations are listed in Table 1
Table 4.
ROC analysis comparing the TyG-WWI and conventional TyG-related parameters for the diagnosis of heart failure
| Test | AUC (95%CI) | Delong-P | NRI (%) | Best threshold | Specificity | Sensitivity |
|---|---|---|---|---|---|---|
| TyG-WWI | 0.697 (0.678–0.715) | – | – | 98.9341 | 0.6241 | 0.6619 |
| TyG | 0.616 (0.595–0.637) | < 0.001 | 11.41% | 8.6429 | 0.5228 | 0.6491 |
| TyG-WC | 0.665 (0.645–0.685) | < 0.001 | 4.20% | 871.3319 | 0.5623 | 0.6818 |
| TyG-WHtR | 0.673 (0.653–0.692) | < 0.001 | 2.99% | 5.4764 | 0.6580 | 0.601 |
For Delong-P, the Bonferroni-corrected p value (0.0167) was used as the significance level
ROC, receiver operating characteristic; AUC, area under the curve; NRI, net reclassification improvement. Other abbreviations are listed in Table 1
Fig. 4.
TyG-WWI and TyG correlation index for the diagnosis of HF ROC curves. Abbreviations: ROC: receiver operating characteristic; AUC: area under the curve. Other abbreviations are listed in Table 1
Sensitivity analysis
Sensitivity analyses confirmed the robustness of the association between the TyG-WWI and HF risk across multiple scenarios (Table 5). For missing data handling, three imputed datasets (sensitivity-1 to sensitivity-3) generated by MICE consistently showed significant positive associations. Each standard deviation increase in the TyG-WWI was associated with 44–45% increased odds of HF (OR range: 1.44–1.45, all 95% CIs excluding 1). The dose‒response relationship remained statistically significant (all p values < 0.01), with participants in the highest quartile (Q4) having approximately 2.46–2.47 times greater HF risk than those in the lowest quartile (Q1). Additional sensitivity analyses further supported the stability of the findings. After excluding extreme values of TyG-WWI (> 140) (sensitivity-4), each standard deviation increase in TyG-WWI was associated with 40% higher odds of HF (OR 1.40, 95% CI 1.16–1.70), and the highest quartile still showed a significant 3.30-fold elevated risk (95% CI 1.62–6.72, p-trend < 0.01). When further adjusting for sleep apnea syndrome and atrial fibrillation history (sensitivity-5), the association remained significant: each standard deviation increase in TyG-WWI corresponded to a 36% higher odds of HF (OR 1.36, 95% CI 1.13–1.64), and the highest quartile had a 3.33-fold greater risk than the lowest quartile did (95% CI 1.62–6.81, p-trend < 0.01). These results collectively indicate that the positive association between the TyG-WWI and HF risk is robust to missing data patterns, extreme values, and additional confounding factors, reinforcing the reliability of the primary findings.
Table 5.
Sensitivity analysis of the association between the TyG-WWI and HF incidence
| OR (95% CI) | |||||
|---|---|---|---|---|---|
| Sensitivity-1 | Sensitivity-2 | Sensitivity-3 | Sensitivity-4 | Sensitivity-5 | |
| TyG-WWI (per SD) | 1.45 (1.25, 1.68) | 1.45 (1.26, 1.68) | 1.44 (1.24, 1.67) | 1.40 (1.16, 1.70) | 1.36 (1.13, 1.64) |
| TyG-WWI | |||||
| Q1 | 1.0(Ref) | 1.0(Ref) | 1.0(Ref) | 1.0(Ref) | 1.0(Ref) |
| Q2 | 1.41 (0.85, 2.32) | 1.41 (0.85, 2.33) | 1.41 (0.85, 2.33) | 2.27 (1.13, 4.57) | 2.27 (1.12, 4.59) |
| Q3 | 1.70 (1.04, 2.78) | 1.70 (1.04, 2.77) | 1.71 (1.05, 2.79) | 2.08 (1.03, 4.21) | 2.05 (1.01, 4.16) |
| Q4 | 2.47 (1.52, 4.01) | 2.47 (1.51, 4.04) | 2.46 (1.51, 4.02) | 3.30 (1.62, 6.72) | 3.33 (1.62, 6.81) |
| p-trend | < 0.01 | < 0.01 | < 0.01 | < 0.01 | < 0.01 |
Sensitivity-1 to sensitivity‐3 were repeated analyses using data after multiple imputations of missing covariates. Sensitivity analysis-4 was repeated after removing the extreme values (greater than 140) of the TYG-WWI. Sensitivity analysis-5 further adjusted for sleep apnea syndrome and atrial fibrillation history on the basis of Model II
Discussion
In this retrospective cross-sectional study, using nationally representative survey data, we investigated—for the first time—a positive linear correlation between the TyG-WWI score and the risk of heart failure. Further subgroup analyses revealed that this association was more pronounced in men, patients not using β-blockers, and nondiabetic individuals, whereas sensitivity analyses consistently confirmed the robustness of our core findings. Notably, our results demonstrated that the TyG-WWI not only exhibited superior diagnostic performance for heart failure than traditional TyG-related parameters but also, more importantly, NRI analyses indicated that the TyG-WWI provides incremental value over these conventional TyG-derived indices. These observations underscore that the TyG-WWI is a promising simple marker that serves as a valuable complement to current TyG-related parameters in assessing heart failure risk.
Despite encouraging advancements in extensive heart failure research in recent years, the prognosis for heart failure patients has remained unchanged [1, 2]. Identifying valuable risk assessment tools is paramount for improving heart failure outcomes. The association between IR and heart failure risk has garnered significant attention. Although accurately assessing IR can be challenging, surrogate markers of IR developed on the basis of routine blood biochemical indicators, such as TyG, have demonstrated good agreement with gold-standard IR assessments [57]. This significantly enhances the practicality of these surrogate markers as disease risk screening and stratification tools. In fact, in addition to IR, several anthropometric parameters used to evaluate obesity have also been proven to be significantly correlated with heart failure risk [31–35]. In particular, on the basis of the widespread discussion of the “obesity paradox,” combining indicators that reflect central obesity and overall obesity is considered a more valuable new anthropometric parameter [36, 37]. Consequently, in recent years, an increasing number of risk assessment tools that combine IR with anthropometric measurements have been developed and proven to have good disease predictive value. The combination of the TyG index and the optimized anthropometric parameter WWI is a recently developed index. Previous studies have indicated a significant correlation between this index and the overall risk of cardiovascular disease and stroke [46, 47]. However, the value of the TyG-WWI in heart failure remains to be further elucidated.
In this study, we evaluated the association between the combination of the TyG score and WWI and the risk of heart failure and reported that high TyG-WWI values are associated with an increased risk of heart failure. Our findings align with previous research examining the relationships among the TyG index, WWI, and heart failure outcomes. The association between TyG and heart failure risk has been widely studied [58], with most research highlighting a positive correlation [28–30, 59–62]. Notably, recent studies have focused specifically on the link between TyG and heart failure with preserved ejection fraction (HFpEF), a subtype characterized by distinct pathophysiological features. One study investigating insulin resistance indices (including TyG) in HFpEF patients revealed that elevated TyG levels correlate with increased adverse events [28], whereas another study demonstrated that a high TyG index is linked to poor prognosis in HFpEF patients, supporting its potential as a prognostic marker [29]. These findings underscore the relevance of TyG-related metabolic perturbations in heart failure subsets, and despite our inability to stratify by ejection fraction owing to dataset limitations, the associations observed in the current study are consistent with these subtype-specific links.Beyond subtype-specific analyses, cumulative evidence from broader populations reinforces the relevance of TyG in heart failure. A meta-analysis revealed a significant association between the TyG index and the incidence of heart failure and adverse outcomes [27], whereas two large cohorts (over 100,000 individuals) and Mendelian randomization studies confirmed that a higher TyG index is an independent, causal risk factor for new-onset heart failure in the general population [63]. However, conflicting evidence exists: one study reported no significant association between TyG and heart failure risk in nonobese individuals (BMI < 30 kg/m2) [64], and another in a nonalcoholic fatty liver disease population showed no association [65], likely due to differences in study design and population selection. Regarding WWI, although research is less extensive than for TyG, limited evidence suggests a significant positive correlation with heart failure risk [43, 66–68]. Our results emphasize that combining the TyG score and WWI into a new parameter strengthens the association with increased heart failure risk: each standard deviation increase in the TyG-WWI was linked to elevated risk, suggesting its promise as a risk assessment tool.
Multiple studies have investigated the diagnostic and predictive value of TyG-related parameters for heart failure. A meta-analysis by Khalaji A et al. [27] demonstrated that the TyG has good discriminatory ability between heart failure and nonheart failure individuals, highlighting its potential as a simple and effective risk stratification and assessment tool for heart failure. In another meta-analysis, the predictive value of TyG-WC for heart failure was also confirmed [69]. Additionally, three cross-sectional studies [19, 60, 65] and one cohort study [70] indicated that the TyG-WHtR has good diagnostic and predictive value for heart failure. A comparison of the three indicators by Dang et al. [60] and Zheng et al. [19] revealed that the TyG-WHtR has greater diagnostic value for heart failure than the TyG and TyG-WC indices do. Similarly, when combined with a basic model, Zhang Y et al.’s study demonstrated that the diagnostic performance of TyG-WHtR combined with the basic model for heart failure is greater than that of TyG [66]. These findings emphasize that the TyG-WHtR is a better diagnostic and predictive indicator for heart failure than the TyG and TyG-WC ratios are. In the present study, for the first time, we assessed the diagnostic value of the TyG-WWI for heart failure. Importantly, compared with the three traditional TyG indicators mentioned above, the TyG-WWI has superior diagnostic value for heart failure (all DeLong test P values < 0.05). Importantly, the results of the NRI analysis indicate that the TyG-WWI has greater predictive value in the diagnosis of heart failure than traditional TyG-related parameters do, as confirmed by positive NRI values: 11.41% compared with TyG, 4.20% compared with TyG-WC, and 2.99% compared with TyG-WHtR. These results suggest that the TyG-WWI can serve as a useful supplement to existing TyG-related parameters in the diagnosis of heart failure, thereby enhancing the accuracy of risk stratification.
The association between the TyG-WWI and heart failure is likely mediated by the synergistic interplay of metabolic dysfunction and obesity-related pathways. In fact, the TyG-WWI was designed to integrate two complementary domains—insulin resistance and central obesity—to overcome the limitations of traditional metabolic risk markers, which often assess these factors in isolation. Its mathematical formulation combines the triglyceride‒glucose (TyG) index and the weight‒adjusted waist index (WWI), with each component having a distinct physiological rationale and calibration background. First, the TyG index, which is composed of triglycerides and glucose, serves as a reliable marker of insulin resistance. Its physiological validity stems from the close link between triglycerides and insulin-resistant states, and its efficacy has been extensively validated against gold-standard methods such as the hyperinsulinemic-euglycemic clamp and HOMA-IR [15]. In insulin resistance, impaired insulin-mediated suppression of lipolysis leads to increased release of free fatty acids, stimulating hepatic synthesis and secretion of triglycerides and increasing circulating triglyceride levels [71]. By combining triglycerides with glucose, the TyG index captures the synergistic effects of dyslipidemia and hyperglycemia—core features of insulin resistance syndrome—thereby enhancing its ability to reflect systemic metabolic dysfunction [72]. Insulin resistance, as indicated by elevated TyG levels, contributes to heart failure pathogenesis through multiple pathways: (1) inducing systemic metabolic disturbances that promote myocardial lipid accumulation and oxidative stress, impairing cardiac structure and function; (2) exacerbating endothelial dysfunction and arterial stiffness to increase cardiac afterload; and (3) triggering chronic low-grade inflammation (via upregulation of proinflammatory cytokines such as TNF-α and IL-6) and activating the renin‒angiotensin‒aldosterone system (RAAS), accelerating myocardial fibrosis, ventricular remodeling, and diastolic dysfunction [73–77]. Additionally, insulin resistance impairs myocardial insulin signaling, reducing myocardial glucose uptake and utilization while shifting substrate preference toward excessive free fatty acid oxidation, which induces mitochondrial dysfunction, lipotoxicity, and lipoapoptosis in cardiomyocytes, directly damaging cardiac structure and function [78, 79]. The WWI component of the TyG-WWI reflects central obesity relative to total body weight and independently increases heart failure risk through multiple mechanisms. First, WWI is calculated as waist circumference (cm) divided by the square root of body weight (kg) and is designed to overcome the limitations of BMI in capturing fat distribution. Derived from regression analyses showing that waist circumference scales with the square root of body weight (β ≈ 0.5), WWI calibrates waist circumference by body weight, optimizing stability across diverse populations and enhancing its ability to reflect visceral adiposity independently of total body mass [38]. Indeed, assessing obesity and related HF risk via BMI and WC alone is complicated by the “obesity paradox” [80], whereas weight-adjusted waist circumference better reflects central obesity. This promotes visceral fat accumulation, which releases proinflammatory cytokines (e.g., TNF-α and IL-6) and adipokines (e.g., leptin and resistin), inducing a state of chronic low-grade inflammation [81] that drives myocardial fibrosis and extracellular matrix remodeling. Furthermore, prior studies have indicated that it increases blood pressure, exacerbates the hemodynamic load, and contributes to ventricular remodeling and diastolic dysfunction [82, 83]. Additionally, abdominal obesity correlates with left ventricular hypertrophy and impaired diastolic relaxation, partly via increased hemodynamic load and sympathetic activation, while also exacerbating dyslipidemia and endothelial dysfunction to accelerate atherosclerotic and nonatherosclerotic cardiac damage [31–33, 84, 85]. By integrating the TyG and WWI, the TyG-WWI amplifies heart failure risk through the synergistic convergence of these pathways. Insulin resistance mediated by the TyG component impairs myocardial substrate utilization and promotes oxidative stress, whereas central obesity captured by WWI induces inflammatory and hemodynamic stress, resulting in a “double hit” to cardiac structure and function. This synergistic integration addresses the limitations of isolated markers in comprehensively assessing combined metabolic and obesity-related risks, which may explain why the TyG-WWI demonstrates superior diagnostic performance for heart failure compared with the traditional TyG index alone, as supported by our comparative analyses of discriminative ability. As a novel composite index, the current calibration of the TyG-WWI relies on indirect validation through its components’ established relationships with cardiometabolic endpoints. Future studies are needed to directly validate these findings against gold-standard measures of metabolic health and obesity-related pathologies.
The TyG-WWI, as a composite indicator integrating metabolic and anthropometric parameters, holds distinct clinical value in HF risk assessment, although its utility must be interpreted within clear boundaries. First, in terms of risk stratification, the TyG-WWI demonstrates incremental value beyond traditional TyG-related indices. With an AUC of 0.697, while lower than the 0.8 threshold required for independent diagnosis, the NRI is meaningful compared with conventional parameters: 11.41% versus the basic TyG index, 4.20% versus TyG-WC, and 2.99% versus TyG-WHtR. These NRI values indicate that the TyG-WWI can correctly reclassify 2.99–11.41% more individuals into their appropriate risk categories, reducing misclassification rates in clinical practice. This is particularly valuable for identifying individuals with mild metabolic‒anthropometric abnormalities who might be missed by traditional risk scores, thereby enhancing the comprehensiveness of risk assessment. Second, as a preliminary screening tool, the TyG-WWI has practical utility in resource-constrained settings. On the basis of the basis of the Youden index maximization principle, its optimal cutoff value for identifying HF is 98.93, balancing a sensitivity of 66.2% and specificity of 62.4%. In regions where advanced diagnostic modalities such as echocardiography or BNP testing are limited, TyG-WWI can efficiently triage high-risk populations using easily measurable parameters (triglycerides, glucose, waist circumference, and weight). Individuals exceeding the cutoff should be prioritized for further comprehensive evaluations via gold-standard methods, aligning with hierarchical healthcare models to optimize resource allocation and minimize missed diagnoses. Third, in guiding clinical management, the TyG-WWI serves as a prompt for metabolic assessment and intervention. An elevated TyG-WWI indicates potential metabolic disturbances linked to insulin resistance, prompting clinicians to conduct thorough evaluations of fasting glucose levels, lipid profiles, and obesity parameters. For patients with elevated TyG-WWI (with or without overt diabetes), lifestyle interventions—including dietary adjustments (e.g., reducing refined carbohydrate intake), regular physical activity, and weight management—may lower TyG-WWI levels by improving insulin sensitivity and lipid metabolism. However, it is crucial to note that direct evidence supporting TyG-WWI-guided pharmacological interventions for improving HF outcomes remains limited; treatment decisions should be individualized on the basis of comorbidities, current guidelines, and patient-specific conditions. Notably, the TyG-WWI should never be used alone for HF diagnosis or clinical decision-making. Its role is strictly complementary, enhancing rather than replacing existing risk assessment tools and standard diagnostic protocols. Future prospective studies are needed to establish definitive clinical decision thresholds and validate whether targeted reduction of TyG-WWI through specific therapies can improve HF prognosis, which will further strengthen its clinical utility in treatment planning.
Our study has several compelling strengths that enhance the reliability and relevance of its findings. First, we utilized data from the NHANES, a large-scale, nationally representative sample, which ensures that our results are generalizable to the U.S. civilian noninstitutionalized population and strengthens the external validity of the associations observed between the TyG-WWI and heart failure. Second, the methodological rigor is a key strength. We employed comprehensive adjustment for a wide range of potential confounding factors, including demographic characteristics, lifestyle factors, clinical indicators, and comorbidities, to minimize the impact of confounding factors on the observed associations. Additionally, rigorous sensitivity analyses—incorporating multiple imputation for missing data, exclusion of extreme values, and further adjustment for additional confounding factors—confirmed the robustness of our findings, ensuring that missing data and potential outliers were unlikely to bias the conclusions. Third, the identification of a clinically actionable optimal cutoff point (98.93) for the TyG-WWI enhances its practical applicability. This threshold, derived from maximizing the Youden index to balance sensitivity and specificity, provides a clear reference for potential clinical use, where individuals with TyG-WWI values above this level may warrant closer monitoring for heart failure risk. Finally, the TyG-WWI itself offers inherent advantages as a screening tool. Composed of easily obtainable parameters (triglycerides, glucose, waist circumference, and weight), it is simple to calculate and applicable in primary care settings, especially in resource-constrained environments where advanced diagnostic tools are limited. When used in combination with other established risk factors, it can serve as a valuable supplementary screening tool to identify individuals at elevated risk of heart failure, facilitating early intervention and risk stratification.
However, several limitations must be acknowledged. First, the cross-sectional design of this study precludes the establishment of a causal relationship between the TyG-WWI and heart failure, which only demonstrated an association. This inherent limitation means that we cannot determine the direction of the relationship, highlighting the need for prospective longitudinal studies to validate the predictive value of the TyG-WWI for incident heart failure and clarify its clinical utility. Second, there is potential for reverse causality. Chronic heart failure can induce metabolic disturbances such as insulin resistance, dyslipidemia, and altered adiposity through mechanisms including neurohormonal activation and chronic inflammation. These changes may increase the TyG-WWI, implying that the observed association could partially reflect metabolic adaptations to preexisting heart failure rather than the TyG-WWI driving the pathogenesis of heart failure. Prospective studies are thus needed to clarify the temporal relationship between the two. Third, the diagnosis of heart failure in this study relied solely on self-reported physician diagnoses, without validation against international criteria (such as Framingham or ESC guidelines) or objective indicators such as echocardiography, BNP, or medical records. This may introduce diagnostic bias, including misclassification of undiagnosed asymptomatic or subclinical cases and recall bias affecting reporting accuracy. Additionally, owing to the constraints of the NHANES dataset, we were unable to obtain detailed subtype information on the basis of the ejection fraction, limiting analysis of the associations between the TyG-WWI and specific heart failure phenotypes. While the NHANES employs standardized survey procedures to reduce reporting variability and sampling weights to enhance population representativeness, these methods cannot fully eliminate the uncertainties introduced by the lack of objective diagnostic validation.
Fourth, a high proportion of participants were excluded because of missing data on key variables, with significant differences in age, comorbidities, and metabolic indices between the included and excluded groups. Despite the use of multiple imputation by chained equations to address missingness, residual bias from these baseline disparities cannot be completely eliminated, potentially restricting the generalizability of our findings. Finally, residual confounding may persist despite extensive covariate adjustment. Furthermore, the modest AUC of the TyG-WWI, while statistically significant, indicates that it should complement rather than replace existing risk assessment tools. Our findings are exploratory, and any discussion of TyG-WWI-guided interventions remains speculative, given the unresolved challenges in targeting insulin resistance for clinical benefit.
Conclusion
In this cross-sectional study, we demonstrated that the TyG-WWI is strongly, independently, and dose-dependently associated with HF risk in the general population. Notably, its diagnostic performance for HFs surpasses that of traditional TyG-related indices, and NRI analyses further confirm its incremental value as a supplementary parameter to existing TyG-derived metrics. These findings position the TyG-WWI as a promising metabolic biomarker for HF risk stratification, with its simplicity—rooted in easily measurable parameters (triglycerides, glucose, waist circumference, and weight)—rendering it particularly valuable in resource-limited settings where advanced diagnostic tools are scarce. Given its clinical utility, the TyG-WWI could serve as a practical tool for HF risk assessment in primary care, facilitating more precise identification of high-risk individuals. Future longitudinal studies are warranted to investigate whether monitoring the TyG-WWI can enable earlier targeted interventions, potentially mitigating HF incidence and improving patient outcomes.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all the workers who contributed to the collection and collation of the NHANES data and all the authors for their contributions to this study.
Author contributions
L.H.-Y. conceptualized the study, developed the methodology, supervised the project, and administered its execution. Y.Q.-F. wrote the original draft. Y.Q.-F., D.-Y., K.B.-Z., L.-C., and L.H.-Y. reviewed and edited the manuscript. Y.Q.-F. and D.-Y. developed the software. Y.Q.-F., D.-Y., K.B.-Z., and L.-C. performed formal analysis and validation. Y.Q.-F., D.-Y., and K.B.-Z. curated the data. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ran J, Zhou P, Wang J, Zhao X, Huang Y, Zhou Q, et al. Global, regional, and national burden of heart failure and its underlying causes, 1990–2021: results from the global burden of disease study 2021. Biomark Res. 2025;13:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Z, Li Z, Li X, Yan Y, Liu J, Wang J, et al. Global trends in heart failure from 1990 to 2019: an age-period-cohort analysis from the Global Burden of Disease study. ESC Heart Fail. 2024;11:3264–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e895-1032. [DOI] [PubMed] [Google Scholar]
- 4.Hogenhuis J, Voors AA, Jaarsma T, Hillege HL, Boomsma F, van Veldhuisen DJ. Influence of age on natriuretic peptides in patients with chronic heart failure: a comparison between ANP/NT-ANP and BNP/NT-proBNP. Eur J Heart Fail. 2005;7:81–6. [DOI] [PubMed] [Google Scholar]
- 5.DeFilippi CR, Christenson RH. B-type natriuretic peptide (BNP)/NT-proBNP and renal function: is the controversy over? Clin Chem. 2009;55:1271–3. [DOI] [PubMed] [Google Scholar]
- 6.Wang X, Deng C, Cao X, Gao H. Risk variables of heart failure among patients in China: gray relational approach based multidimensional assessment study. Diabetol Metab Syndr. 2024;16:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Essen BJ, Emmens JE, Tromp J, Ouwerkerk W, Smit MD, Geluk CA, et al. Sex-specific risk factors for new-onset heart failure: the PREVEND study at 25 years. Eur Heart J. 2025;46:1528–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen Q, Clark L, Diaz FJ, Pierce JD. Multidimensional risk factors for heart failure in Hispanic adults: findings from the all of Us research program. Am J Cardiol. 2025;245:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014;1:4–25. [DOI] [PubMed] [Google Scholar]
- 10.Tian X, Chen S, Xia X, Xu Q, Zhang Y, Zheng C, et al. Pathways from insulin resistance to incident cardiovascular disease: a Bayesian network analysis. Cardiovasc Diabetol. 2024;23:421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14:575–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang F, Yu Z. Mendelian randomization study on insulin resistance and risk of hypertension and cardiovascular disease. Sci Rep. 2024;14: 6191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart AJ, Tuncay E, Pitt SJ, Rainbow RD. Editorial: insulin resistance and cardiovascular disease. Front Endocrinol. 2023;14:1266173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luo JW, Duan WH, Yu YQ, Song L, Shi DZ. Prognostic significance of triglyceride-glucose index for adverse cardiovascular events in patients with coronary artery disease: a systematic review and meta-analysis. Front Cardiovasc Med. 2021;8: 774781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mo D, Zhang P, Zhang M, Dai H, Guan J. Cholesterol, high-density lipoprotein, and glucose index versus triglyceride-glucose index in predicting cardiovascular disease risk: a cohort study. Cardiovasc Diabetol. 2025;24:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Y, Li S, Ren Q, Qiu Y, Pan M, Liu G, et al. The interaction between triglyceride-glucose index and visceral adiposity in cardiovascular disease risk: findings from a nationwide Chinese cohort. Cardiovasc Diabetol. 2024;23:427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng D, Cai J, Xu S, Jiang S, Li C, Wang B. The association of triglyceride-glucose index and combined obesity indicators with chest pain and risk of cardiovascular disease in American population with prediabetes or diabetes. Front Endocrinol. 2024;15:1471535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xia X, Chen S, Tian X, Xu Q, Zhang Y, Zhang X, et al. Association of triglyceride-glucose index and its related parameters with atherosclerotic cardiovascular disease: evidence from a 15-year follow-up of Kailuan cohort. Cardiovasc Diabetol. 2024;23:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang B, Li L, Tang Y, Ran X. Joint association of triglyceride glucose index (TyG) and body roundness index (BRI) with stroke incidence: a national cohort study. Cardiovasc Diabetol. 2025;24:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ren X, Chen M, Lian L, Xia H, Chen W, Ge S, et al. The triglyceride-glucose index is associated with a higher risk of hypertension: evidence from a cross-sectional study of Chinese adults and meta-analysis of epidemiology studies. Front Endocrinol. 2025;16:1516328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dakota I, Huang W, Wijayanto MA, Nurhafizah A, Khairunnisa AR, Rachmayanti S, et al. Prognostic value of triglyceride-glucose index on predicting major adverse cardiovascular events in hypertensive patients: a systematic review and meta-analysis. Am J Prev Cardiol. 2025;22: 100996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li C, Zhao S, Li Y, He S, Jian W, Liu Y, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with H-type hypertension combined with coronary heart disease: a retrospective cohort study. Cardiovasc Diabetol. 2025;24:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho JE, Chen ZZ, Lau ES. Insulin resistance and diabetes in HFpEF: bystander or instigator? J Am Coll Cardiol. 2025;85:1789–91. [DOI] [PubMed] [Google Scholar]
- 26.Aroor AR, Mandavia CH, Sowers JR. Insulin resistance and heart failure: molecular mechanisms. Heart Fail Clin. 2012;8:609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khalaji A, Behnoush AH, Khanmohammadi S, Ghanbari MK, Sharifkashani S, Sahebkar A, et al. Triglyceride-glucose index and heart failure: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;22:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ni W, Jiang R, Xu D, Zhu J, Chen J, Lin Y, et al. Association between insulin resistance indices and outcomes in patients with heart failure with preserved ejection fraction. Cardiovasc Diabetol. 2025;24:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou Q, Yang J, Tang H, Guo Z, Dong W, Wang Y, et al. High triglyceride-glucose (TyG) index is associated with poor prognosis of heart failure with preserved ejection fraction. Cardiovasc Diabetol. 2023;22:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng H, Wu K, Wu W, Huang Z, Wang X, Fu P, et al. Relationship of the trajectory of the triglyceride-glucose index with heart failure: the Kailuan study. Lipids Health Dis. 2024;23:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chambers JC, Eda S, Bassett P, Karim Y, Thompson SG, Gallimore JR, et al. C-reactive protein, insulin resistance, central obesity, and coronary heart disease risk in Indian Asians from the United Kingdom compared with European whites. Circulation. 2001;104:145–50. [DOI] [PubMed] [Google Scholar]
- 32.Nigro J, Osman N, Dart AM, Little PJ. Insulin resistance and atherosclerosis. Endocr Rev. 2006;27:242–59. [DOI] [PubMed] [Google Scholar]
- 33.Lovren F, Teoh H, Verma S. Obesity and atherosclerosis: mechanistic insights. Can J Cardiol. 2015;31:177–83. [DOI] [PubMed] [Google Scholar]
- 34.Campbell DJ, Gong FF, Jelinek MV, Castro JM, Coller JM, McGrady M, et al. Threshold body mass index and sex-specific waist circumference for increased risk of heart failure with preserved ejection fraction. Eur J Prev Cardiol. 2019;26:1594–602. [DOI] [PubMed] [Google Scholar]
- 35.Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation. 2010;121:237–44. [DOI] [PubMed] [Google Scholar]
- 36.Roush K. Obesity should not be defined by BMI alone. Am J Nurs. 2025;125:15. [DOI] [PubMed] [Google Scholar]
- 37.Graham F. Daily briefing: New obesity definition sidelines BMI to focus on health. Nature. 2025. [DOI] [PubMed]
- 38.Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8: 16753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang H, Qin Y, Niu J, Chen H, Lu X, Wang R, et al. Evolving perspectives on evaluating obesity: from traditional methods to cutting-edge techniques. Ann Med. 2025;57: 2472856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH. Associations between weight-adjusted waist index and abdominal fat and muscle mass: multi-ethnic study of atherosclerosis. Diabetes Metab J. 2022;46:747–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu J, Guo J. Is weight-adjusted waist index more strongly associated with diabetes than body mass index and waist circumference?: results from the database large community sample study. PLoS ONE. 2024;19: e0309150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu W, Yang X, Zhan T, Huang M, Tian X, Tian X, et al. Weight-adjusted waist index is positively and linearly associated with all-cause and cardiovascular mortality in metabolic dysfunction-associated steatotic liver disease: findings from NHANES 1999–2018. Front Endocrinol. 2024;15:1457869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tao Z, Zuo P, Ma G. Association of weight-adjusted waist index with cardiovascular disease and mortality among metabolic syndrome population. Sci Rep. 2024;14: 18684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huo G, Tan Z, Tang Y, Huang J, Cao J, Zhou D. Association between triglyceride glucose weight adjusted waist index and stroke risk in different glucose metabolism status. Sci Rep. 2025;15(1): 15813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duan C, Lyu M, Shi J, Shou X, Zhao L, Hu Y. Associations of baseline and changes in the triglyceride glucose-weight adjusted waist index and cardiovascular disease risk: evidence from middle-aged and older individuals. Cardiovasc Diabetol. 2024;23:415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen W, Zhang G, Lei Q, Lu H. Prognostic value of advanced lung cancer inflammation index in heart failure patients: a comprehensive analysis. ESC Heart Fail. 2025;12:2298–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang L, Xu Y, Chen L, Zhang H. Estimated glucose disposal rate mediates the association between life’s Crucial 9 and congestive heart failure: a population-based study. Front Endocrinol. 2025;16:1540794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AR, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf.
- 50.Liu C, Hua L, Xin Z. Synergistic impact of 25-hydroxyvitamin D concentrations and physical activity on delaying aging. Redox Biol. 2024;73: 103188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu H, Xie P, Liu H, Tian Z, Zhang R, Cui M. The relationship between dietary inflammatory index in adults and coronary heart disease: from NHANES 1999–2018. Front Nutr. 2025;12:1564580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang W, Gao B, Wang Y, Cao Y, Wang J. The relationship between hepatic steatosis index and hypertension: NHANES 2011–2018. BMC Cardiovasc Disord. 2025;25:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Standards of medical care in diabetes 2010. Diabetes Care. 2010;33 Suppl 1:S11–61. [DOI] [PMC free article] [PubMed]
- 54.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112:2735–52. [DOI] [PubMed] [Google Scholar]
- 55.Charlson ME, Carrozzino D, Guidi J, Patierno C. Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom. 2022;91:8–35. [DOI] [PubMed] [Google Scholar]
- 56.Cheng Y, Fang Z, Zhang X, Wen Y, Lu J, He S, et al. Association between triglyceride glucose-body mass index and cardiovascular outcomes in patients undergoing percutaneous coronary intervention: a retrospective study. Cardiovasc Diabetol. 2023;22:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95:3347–51. [DOI] [PubMed] [Google Scholar]
- 58.Alotaibi A, Mahapatro A, Mirchandani M, Adla JS, Mohanty E, Marsool MM, et al. Triglyceride-glucose index as a marker in cardiovascular diseases; a bibliometric study and visual analysis. Ann Med Surg. 2025;87:1487–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Q, Zhou K, Li Y, Dong W, Sun Y, Wu H, et al. Associations between the triglyceride-glucose index and the risk of heart failure in patients undergoing maintenance hemodialysis: a retrospective cohort study. Front Endocrinol. 2025;16:1544591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dang K, Wang X, Hu J, Zhang Y, Cheng L, Qi X, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003–2018. Cardiovasc Diabetol. 2024;23:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dui X, Chen X, Zhu L, Han X, Ma T, Lv L, et al. The association between derived TyG index and the risk of heart failure in the elderly population: a prospective cohort study from 2017 to 2023. BMC Public Health. 2025;25:863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xu Z, Yan X, Li D, Huang X. Triglyceride glucose index as a biomarker for heart failure risk in H-type hypertension patients. Sci Rep. 2025;15: 4828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li X, Chan J, Guan B, Peng S, Wu X, Lu X, et al. Triglyceride-glucose index and the risk of heart failure: evidence from two large cohorts and a mendelian randomization analysis. Cardiovasc Diabetol. 2022;21: 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li X, Wang J, Niu L, Tan Z, Ma J, He L, et al. Prevalence estimates of the insulin resistance and associated prevalence of heart failure among United Status adults. BMC Cardiovasc Disord. 2023;23:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang Y, Wang F, Tang J, Shen L, He J, Chen Y. Association of triglyceride glucose-related parameters with all-cause mortality and cardiovascular disease in NAFLD patients: NHANES 1999–2018. Cardiovasc Diabetol. 2024;23:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guo FS, Guo C, Dou JH, Wang JX, Wu RY, Song SF, et al. Association of surrogate adiposity markers with prevalence, all-cause mortality and long-term survival of heart failure: a retrospective study from NHANES database. Front Endocrinol. 2025;16:1430277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang D, Shi W, Ding Z, Park J, Wu S, Zhang J. Association between weight-adjusted-waist index and heart failure: results from National Health and Nutrition Examination Survey 1999–2018. Front Cardiovasc Med. 2022;9:1069146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fang H, Xie F, Li K, Li M, Wu Y. Association between weight-adjusted-waist index and risk of cardiovascular diseases in United States adults: a cross-sectional study. BMC Cardiovasc Disord. 2023;23:435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rabiee RM, Ghasempour DG, Sadri H, Darouei B, Amani-Beni R, Mazaheri-Tehrani S. Triglyceride glucose-waist circumference as a predictor of mortality and subtypes of cardiovascular disease: a systematic review and meta-analysis. Diabetol Metab Syndr. 2025;17:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huang H, Xiong Y, Zhou J, Tang Y, Chen F, Li G, et al. The predictive value of estimated glucose disposal rate and its association with myocardial infarction, heart failure, atrial fibrillation and ischemic stroke. Diabetes Obes Metab. 2025;27:1359–68. [DOI] [PubMed] [Google Scholar]
- 71.Lee AT, Yang MY, Lee YJ, Yang TW, Wang CC, Wang CJ. Gallic acid improves diabetic steatosis by downregulating MicroRNA-34a-5p through targeting NFE2L2 expression in high-fat diet-Fed db/db Mice. Antioxidants-Basel. 2021;11:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ramdas NV, Satheesh P, Shenoy MT, Kalra S. Triglyceride glucose (TyG) index: a surrogate biomarker of insulin resistance. J Pak Med Assoc. 2022;72:986–8. [DOI] [PubMed] [Google Scholar]
- 73.Meng Z, Zhang Z, Zhao J, Liu C, Yao P, Zhang L, et al. Nitrative modification of Caveolin-3: a novel mechanism of cardiac insulin resistance and a potential therapeutic target against ischemic heart failure in prediabetic animals. Circulation. 2023;147:1162–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Erqou S, Adler AI, Challa AA, Fonarow GC, Echouffo-Tcheugui JB. Insulin resistance and incident heart failure: a meta-analysis. Eur J Heart Fail. 2022;24:1139–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zheng L, Li B, Lin S, Chen L, Li H. Role and mechanism of cardiac insulin resistance in occurrence of heart failure caused by myocardial hypertrophy. Aging. 2019;11:6584–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Saotome M, Ikoma T, Hasan P, Maekawa Y. Cardiac insulin resistance in heart failure: the role of mitochondrial dynamics. Int J Mol Sci. 2019;20:3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fujii S. Insulin resistance and heart failure: underlying molecular mechanisms and potential pharmacological solutions. J Cardiovasc Pharm. 2013;62:379–80. [DOI] [PubMed] [Google Scholar]
- 78.Mellor KM, Ritchie RH, Delbridge LM. Reactive oxygen species and insulin-resistant cardiomyopathy. Clin Exp Pharmacol Physiol. 2010;37:222–8. [DOI] [PubMed] [Google Scholar]
- 79.Abel ED. Insulin signaling in the heart. Am J Physiol-Endoc M. 2021;321:E130–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61:151–6. [DOI] [PubMed] [Google Scholar]
- 81.Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Esquivel-Soto J, Morales-González A, Esquivel-Chirino C, et al. Inflammation, oxidative stress, and obesity. Int J Mol Sci. 2011;12:3117–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Qian P, Wang Q, Wang FZ, Dai HB, Wang HY, Gao Q, et al. Adrenomedullin improves cardiac remodeling and function in obese rats with hypertension. Pharmaceuticals. 2022. 10.3390/ph15060719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7. [DOI] [PubMed] [Google Scholar]
- 84.Jia G, Aroor AR, Martinez-Lemus LA, Sowers JR. Overnutrition, mTOR signaling, and cardiovascular diseases. Am J Physiol-Regul Integr Comp Physiol. 2014;307:R1198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sarfaraz S, Singh S, Hawke A, Clarke ST, Ramdath DD. Effects of high-fat diet induced obesity and fructooligosaccharide supplementation on cardiac protein expression. Nutrients. 2020;12:3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.