Abstract
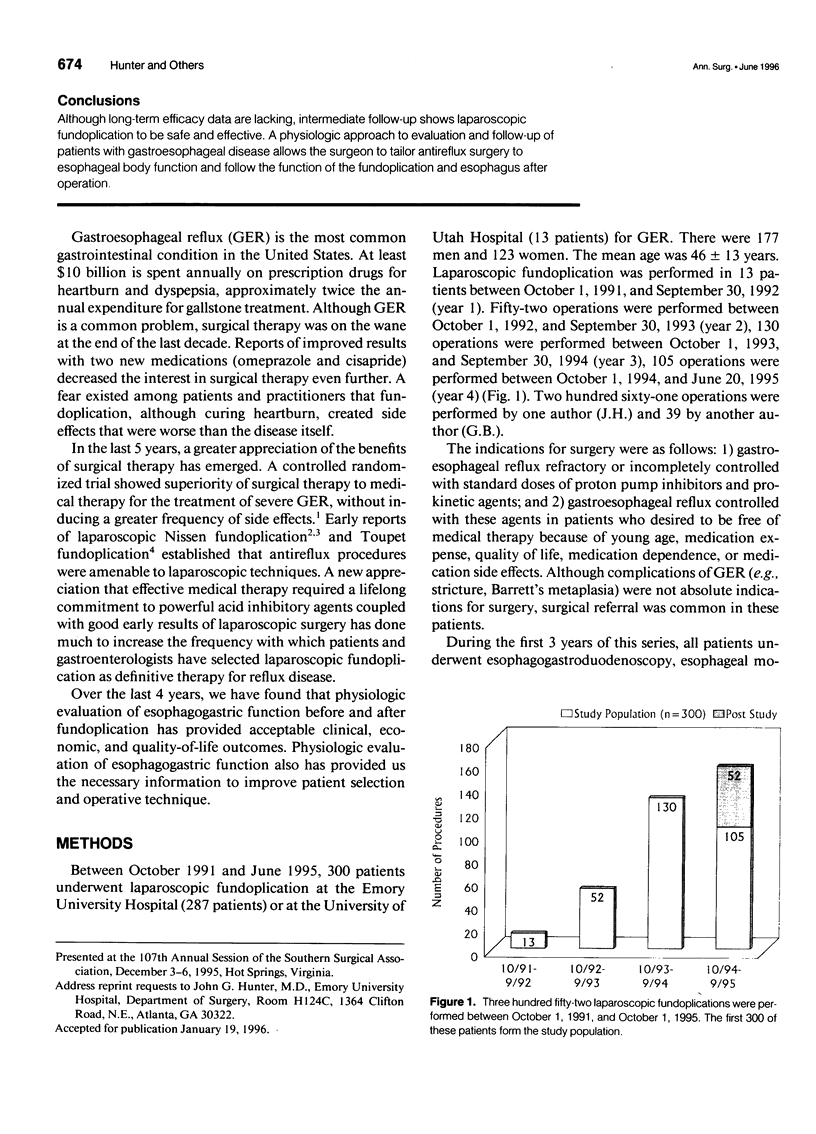
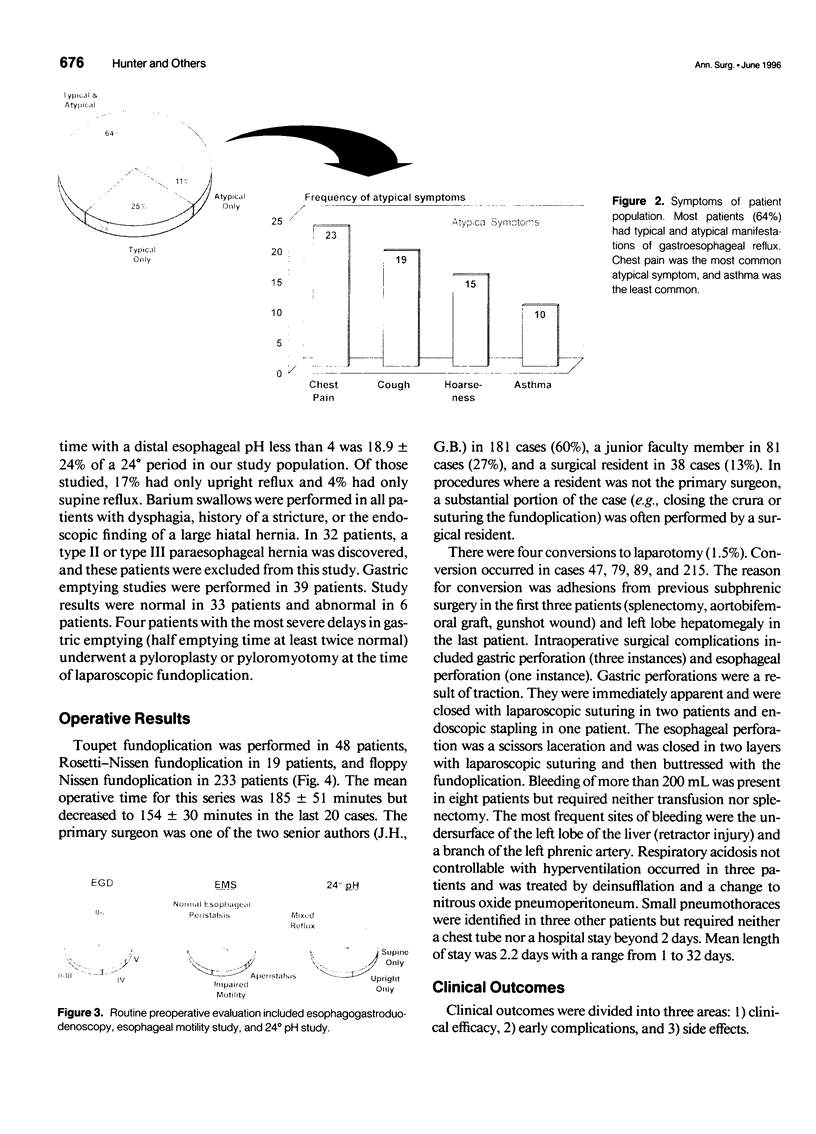
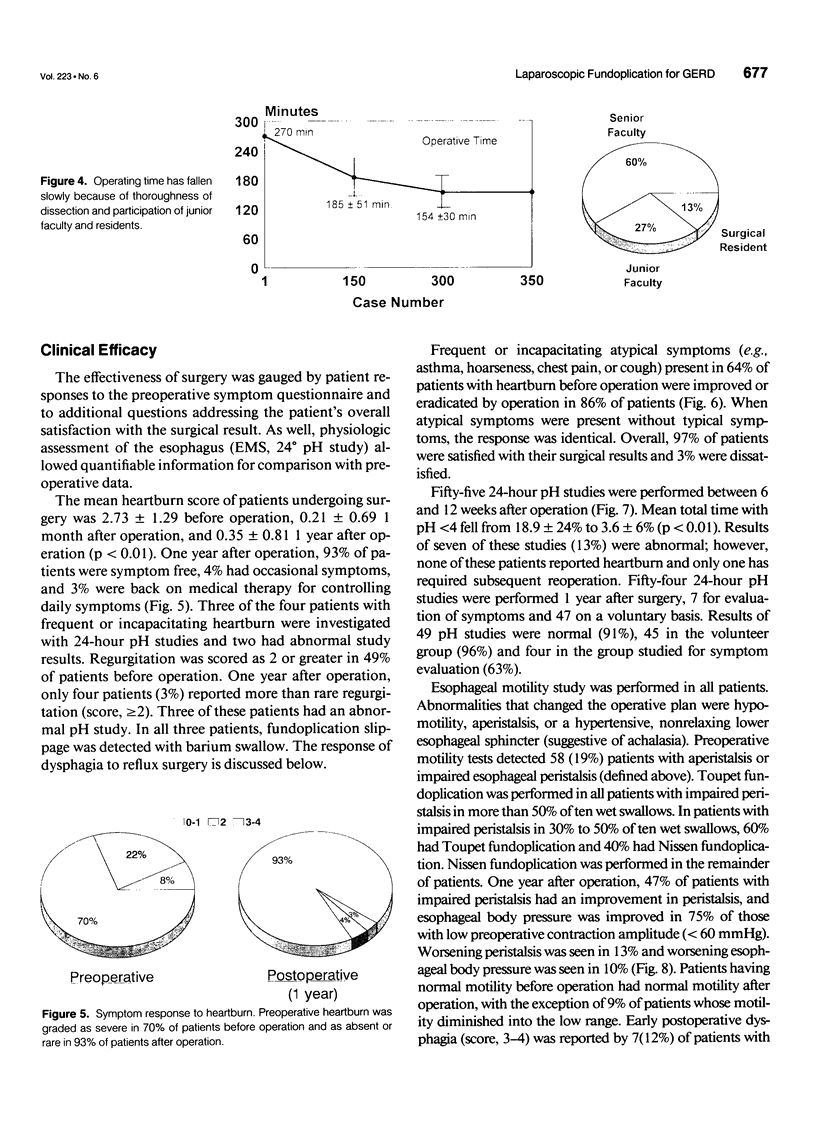
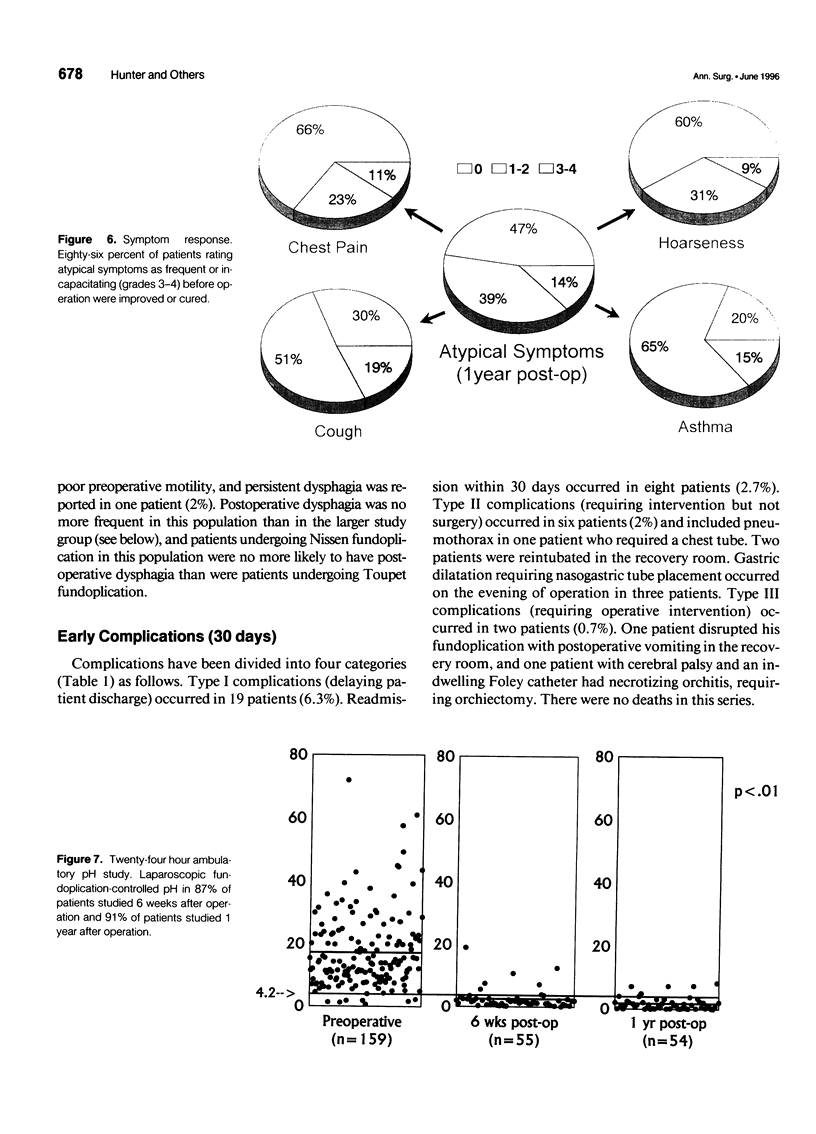
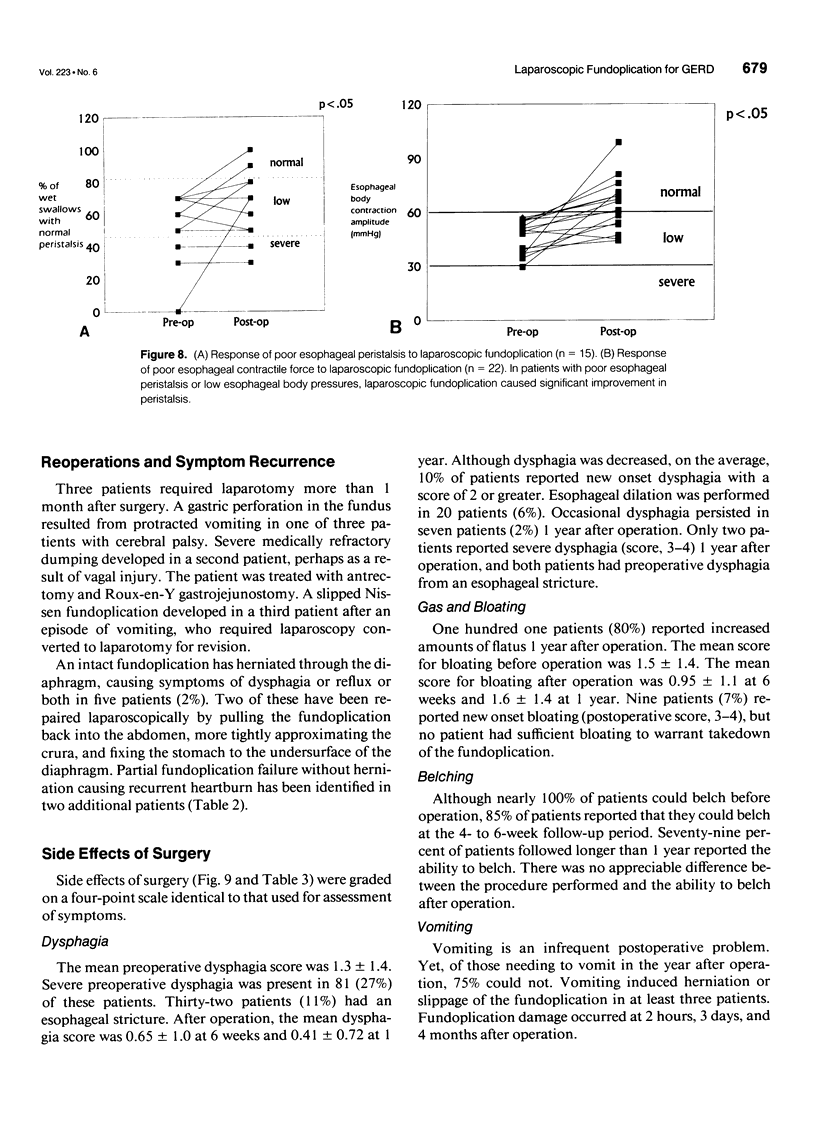
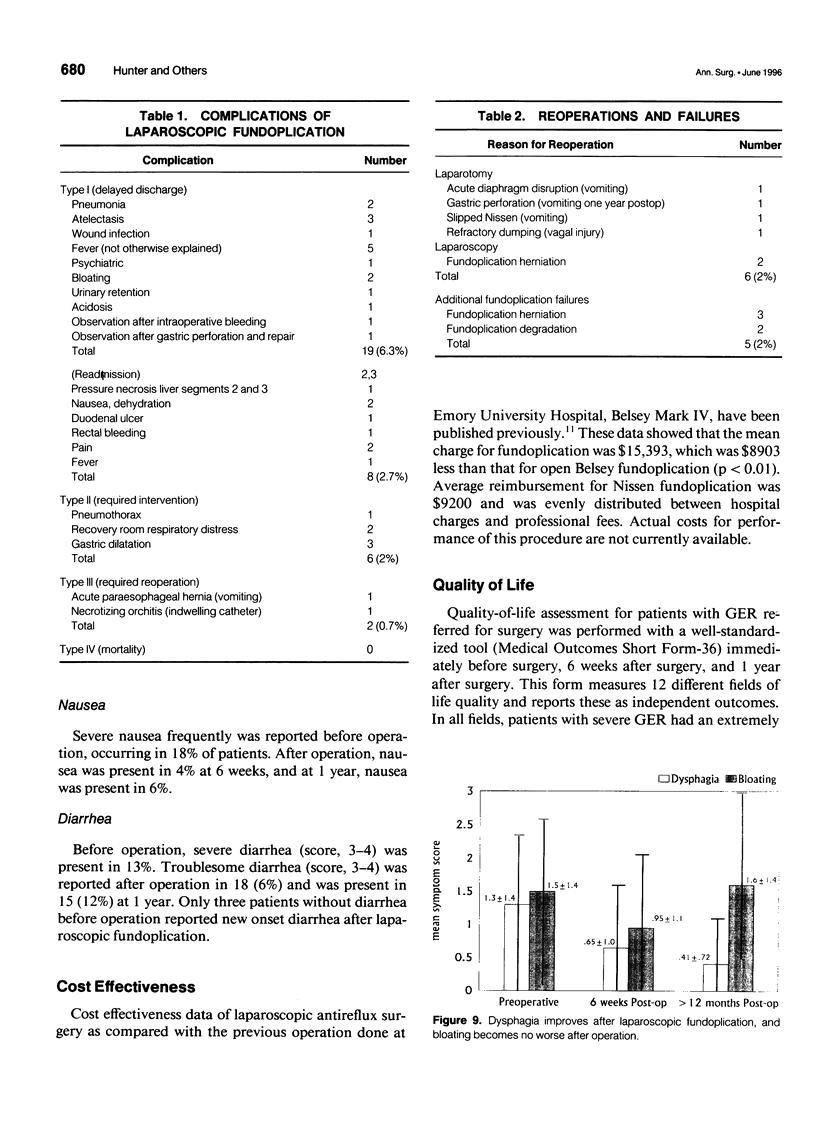
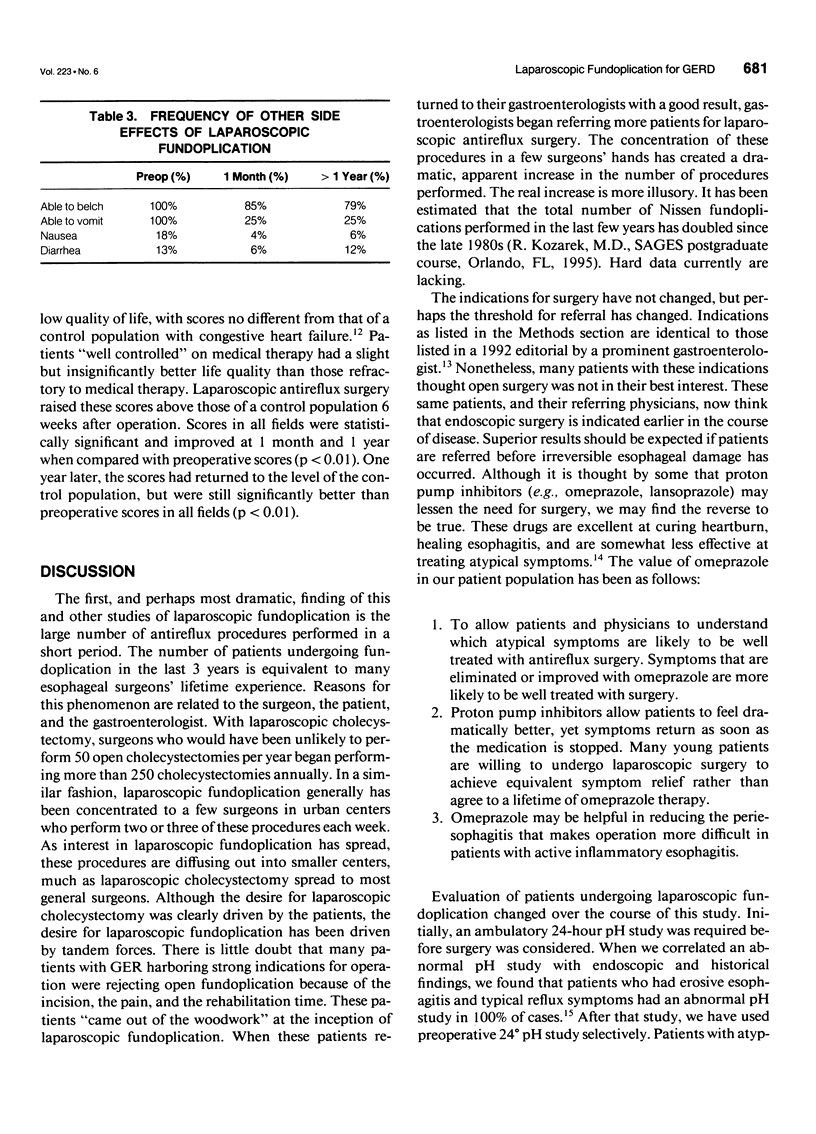
OBJECTIVE: The authors examined indications, evaluations, and outcomes after laparoscopic fundoplication in patients with gastroesophageal reflux through this single-institution study. SUMMARY OF BACKGROUND DATA: Laparoscopic fundoplication has been performed for less than 5 years, yet the early and intermediate results suggest that this operation is safe and equivalent in efficacy to open techniques of antireflux surgery. METHODS: Over a 4-year period, 300 patients underwent laparoscopic Nissen fundoplication (252) or laparoscopic Toupet fundoplication (48) for gastroesophageal reflux refractory to medical therapy or requiring daily therapy with omeprazole or high-dose H2 antagonists. Preoperative evaluation included symptom assessment, esophagogastroduodenoscopy, 24-hour pH evaluation, and esophageal motility study. Physiologic follow-up included 24-hour pH study and esophageal motility study performed 6 weeks and 1 to 3 years after operation. RESULTS: The most frequent indication for surgery was the presence of residual typical and atypical gastroesophageal reflux symptoms (64%) despite standard doses of proton pump inhibitors. At preoperative evaluation, 51% of patients had erosive esophagitis, stricture, or Barrett's metaplasia. Ninety-eight percent of patients had an abnormal 24-hour pH study. Seventeen percent had impaired esophageal motility and 2% had aperistalsis. There were four conversions to open fundoplication (adhesions, three; large liver, one). Intraoperative technical difficulties occurred in 19(6%) patients and were dealt with intraoperatively in all but 1 patient (bleeding from enlarged left liver lobe). Minor complications occurred in 6% and major complications in 2%. There was no mortality. Median follow-up was 17 months. One year after operation, heartburn was absent in 93%. Four percent took occasional H2 antagonists, and 3% were back on daily therapy. Atypical reflux symptoms (e.g., asthma, hoarseness, chest pain, or cough) were eliminated or improved in 87% and no better in 13%. Overall patient satisfaction was 97%. Four patients have subsequently undergone laparotomy for repair of gastric perforation (1 year after operation), severe dumping, "slipped" Nissen, and repair of acute paraesophageal herniation. Two patients had laparoscopic revision of herniated fundoplications. Results of follow-up 24-hour pH studies were normal in 91% of patients more than 1 year after operation. In patients with poor esophageal motility, esophageal body pressure improved 1 year after operation in 75% and worsened in 10%. CONCLUSIONS: Although long-term efficacy data are lacking, intermediate follow-up shows laparoscopic fundoplication to be safe and effective. A physiologic approach to evaluation and follow-up of patients with gastroesophageal disease allows the surgeon to tailor antireflux surgery to esophageal body function and follow the function of the fundoplication and esophagus after operation.
Full text
PDF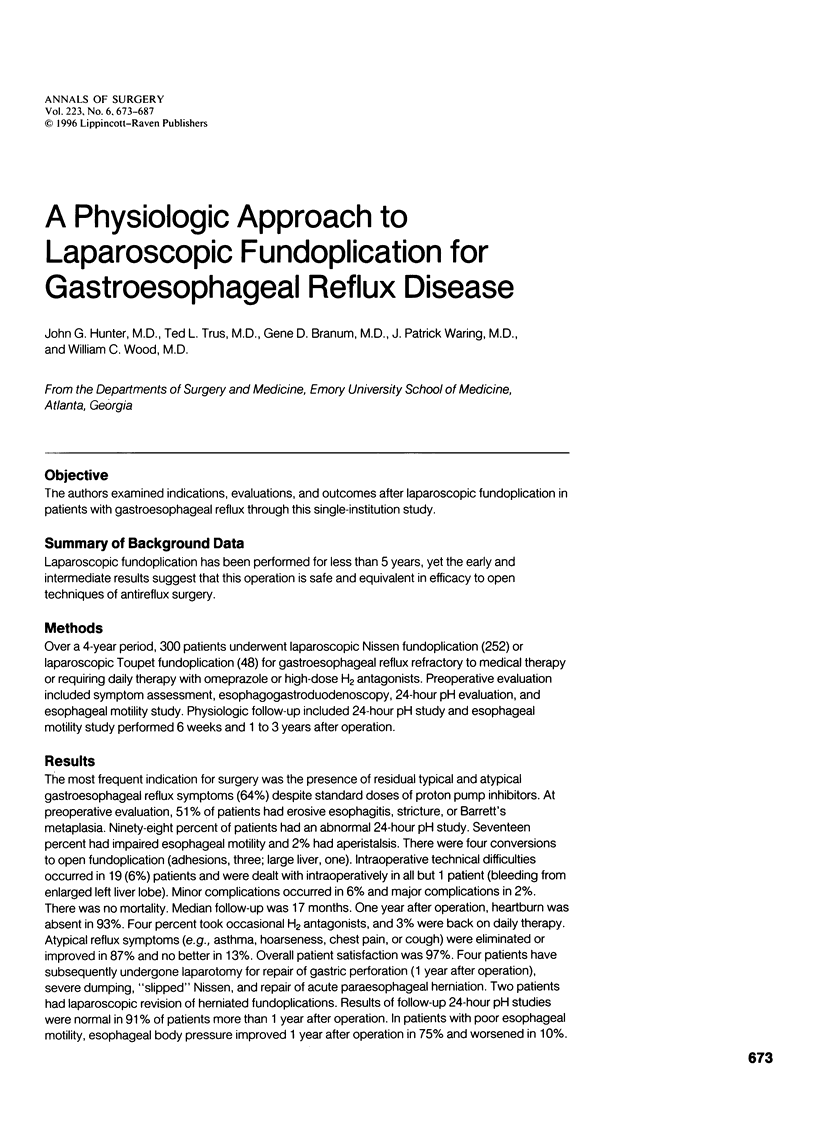


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boutelier P., Jonsell G. An alternative fundoplicative maneuver for gastroesophageal reflux. Am J Surg. 1982 Feb;143(2):260–264. doi: 10.1016/0002-9610(82)90083-6. [DOI] [PubMed] [Google Scholar]
- Bremner R. M., DeMeester T. R., Crookes P. F., Costantini M., Hoeft S. F., Peters J. H., Hagen J. The effect of symptoms and nonspecific motility abnormalities on outcomes of surgical therapy for gastroesophageal reflux disease. J Thorac Cardiovasc Surg. 1994 May;107(5):1244–1250. [PubMed] [Google Scholar]
- Cadière G. B., Houben J. J., Bruyns J., Himpens J., Panzer J. M., Gelin M. Laparoscopic Nissen fundoplication: technique and preliminary results. Br J Surg. 1994 Mar;81(3):400–403. doi: 10.1002/bjs.1800810327. [DOI] [PubMed] [Google Scholar]
- Champault G. Reflux gastro-oesophagien. Traitement par laparoscopie. 940 cas--Expérience française. Ann Chir. 1994;48(2):159–164. [PubMed] [Google Scholar]
- Cuschieri A., Hunter J., Wolfe B., Swanstrom L. L., Hutson W. Multicenter prospective evaluation of laparoscopic antireflux surgery. Preliminary report. Surg Endosc. 1993 Nov-Dec;7(6):505–510. doi: 10.1007/BF00316690. [DOI] [PubMed] [Google Scholar]
- Dallemagne B., Weerts J. M., Jehaes C., Markiewicz S., Lombard R. Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc. 1991 Sep;1(3):138–143. [PubMed] [Google Scholar]
- Donahue P. E., Samelson S., Nyhus L. M., Bombeck C. T. The floppy Nissen fundoplication. Effective long-term control of pathologic reflux. Arch Surg. 1985 Jun;120(6):663–668. doi: 10.1001/archsurg.1985.01390300013002. [DOI] [PubMed] [Google Scholar]
- Fonkalsrud E. W., Ellis D. G., Shaw A., Mann C. M., Jr, Black T. L., Miller J. P., Snyder C. L. A combined hospital experience with fundoplication and gastric emptying procedure for gastroesophageal reflux in children. J Am Coll Surg. 1995 Apr;180(4):449–455. [PubMed] [Google Scholar]
- Geagea T. Laparoscopic Nissen's fundoplication: preliminary report on ten cases. Surg Endosc. 1991;5(4):170–173. doi: 10.1007/BF02653255. [DOI] [PubMed] [Google Scholar]
- Hillman A. L. Economic analysis of alternative treatments for persistent gastro-oesophageal reflux disease. Scand J Gastroenterol Suppl. 1994;201:98–102. doi: 10.3109/00365529409105374. [DOI] [PubMed] [Google Scholar]
- Hinder R. A., Filipi C. J., Wetscher G., Neary P., DeMeester T. R., Perdikis G. Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg. 1994 Oct;220(4):472–483. doi: 10.1097/00000658-199410000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinder R. A., Stein H. J., Bremner C. G., DeMeester T. R. Relationship of a satisfactory outcome to normalization of delayed gastric emptying after Nissen fundoplication. Ann Surg. 1989 Oct;210(4):458–465. doi: 10.1097/00000658-198910000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson G. G., Watson D. I., Britten-Jones R., Mitchell P. C., Anvari M. Laparoscopic Nissen fundoplication. Ann Surg. 1994 Aug;220(2):137–145. doi: 10.1097/00000658-199408000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinkenberg-Knol E. C., Festen H. P., Jansen J. B., Lamers C. B., Nelis F., Snel P., Lückers A., Dekkers C. P., Havu N., Meuwissen S. G. Long-term treatment with omeprazole for refractory reflux esophagitis: efficacy and safety. Ann Intern Med. 1994 Aug 1;121(3):161–167. doi: 10.7326/0003-4819-121-3-199408010-00001. [DOI] [PubMed] [Google Scholar]
- Laycock W. S., Oddsdottir M., Franco A., Mansour K., Hunter J. G. Laparoscopic Nissen fundoplication is less expensive than open Belsey Mark IV. Surg Endosc. 1995 Apr;9(4):426–430. doi: 10.1007/BF00187166. [DOI] [PubMed] [Google Scholar]
- Lundell L. R., Myers J. C., Jamieson G. G. Delayed gastric emptying and its relationship to symptoms of "gas float" after antireflux surgery. Eur J Surg. 1994 Mar;160(3):161–166. [PubMed] [Google Scholar]
- Peters J. H., Heimbucher J., Kauer W. K., Incarbone R., Bremner C. G., DeMeester T. R. Clinical and physiologic comparison of laparoscopic and open Nissen fundoplication. J Am Coll Surg. 1995 Apr;180(4):385–393. [PubMed] [Google Scholar]
- Poirier N. C., Taillefer R., Topart P., Duranceau A. Antireflux operations in patients with scleroderma. Ann Thorac Surg. 1994 Jul;58(1):66–73. doi: 10.1016/0003-4975(94)91073-1. [DOI] [PubMed] [Google Scholar]
- Richter J. E. Surgery for reflux disease: reflections of a gastroenterologist. N Engl J Med. 1992 Mar 19;326(12):825–827. doi: 10.1056/NEJM199203193261209. [DOI] [PubMed] [Google Scholar]
- Rossetti M., Hell K. Fundoplication for the treatment of gastroesophageal reflux in hiatal hernia. World J Surg. 1977 Jul;1(4):439–443. doi: 10.1007/BF01565907. [DOI] [PubMed] [Google Scholar]
- Spechler S. J. Comparison of medical and surgical therapy for complicated gastroesophageal reflux disease in veterans. The Department of Veterans Affairs Gastroesophageal Reflux Disease Study Group. N Engl J Med. 1992 Mar 19;326(12):786–792. doi: 10.1056/NEJM199203193261202. [DOI] [PubMed] [Google Scholar]
- Waring J. P., Hunter J. G., Oddsdottir M., Wo J., Katz E. The preoperative evaluation of patients considered for laparoscopic antireflux surgery. Am J Gastroenterol. 1995 Jan;90(1):35–38. [PubMed] [Google Scholar]