Abstract
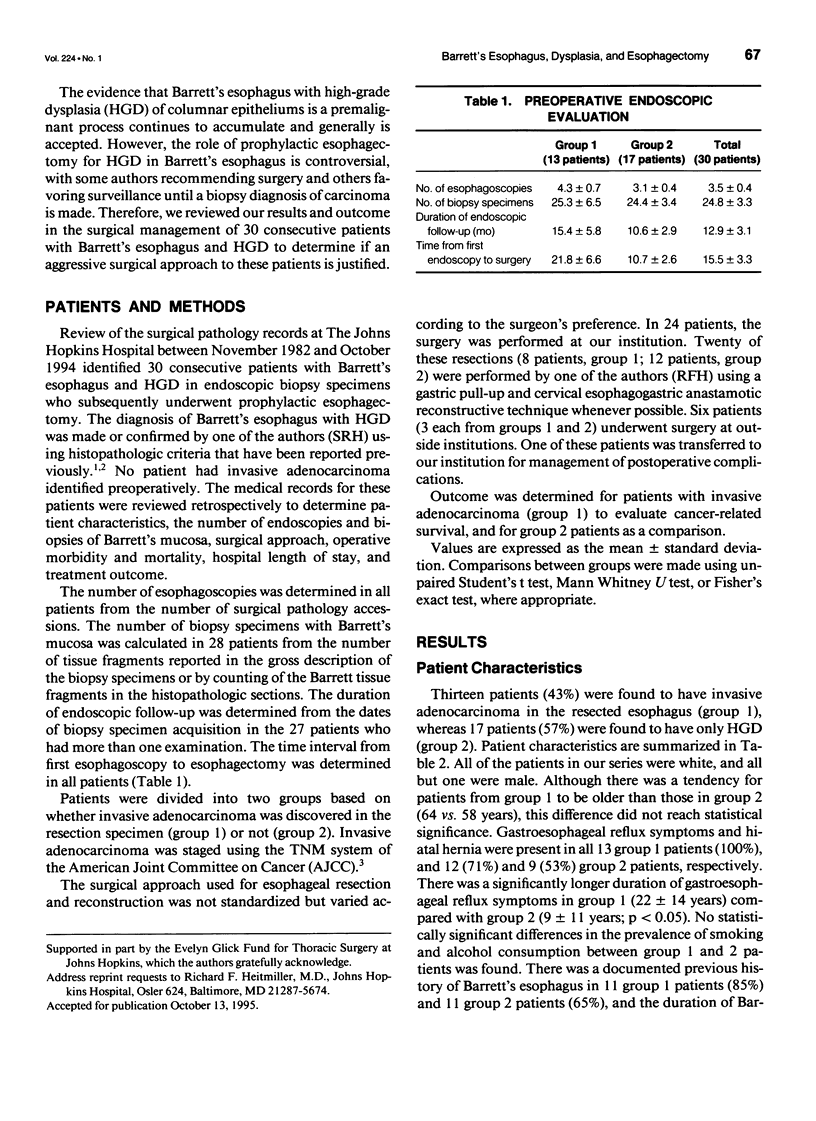
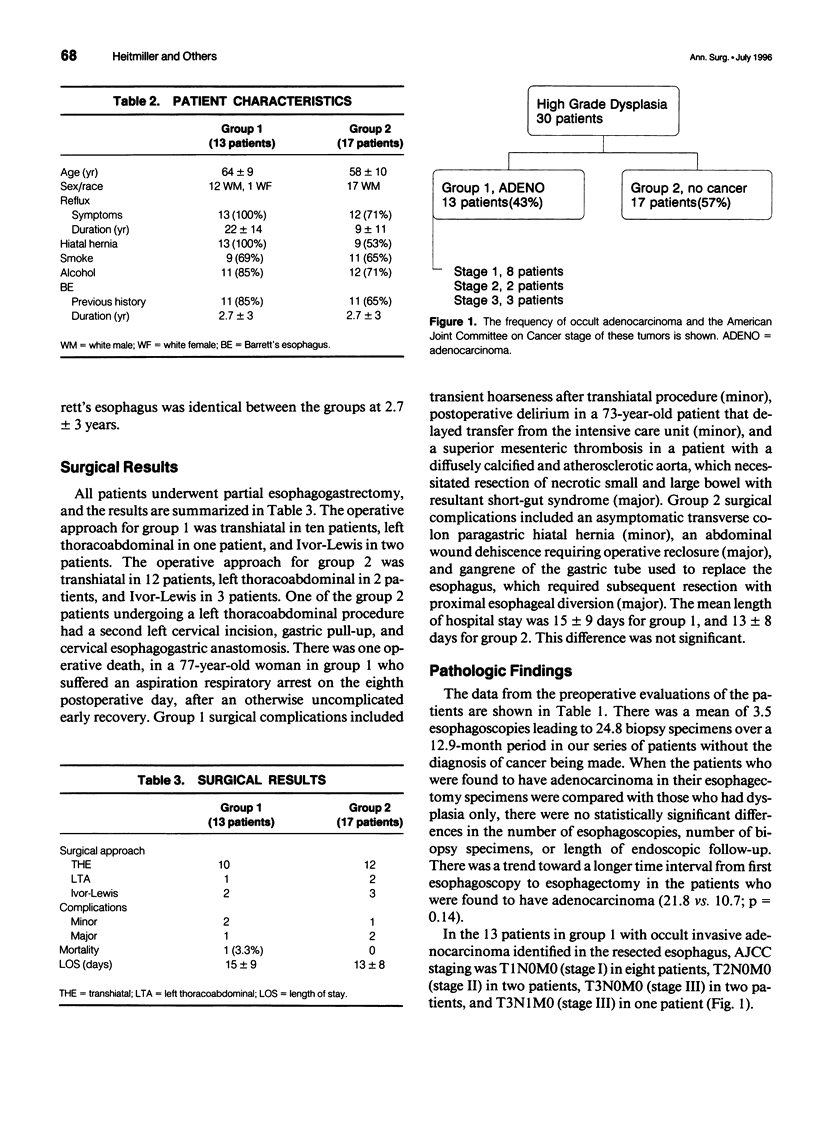
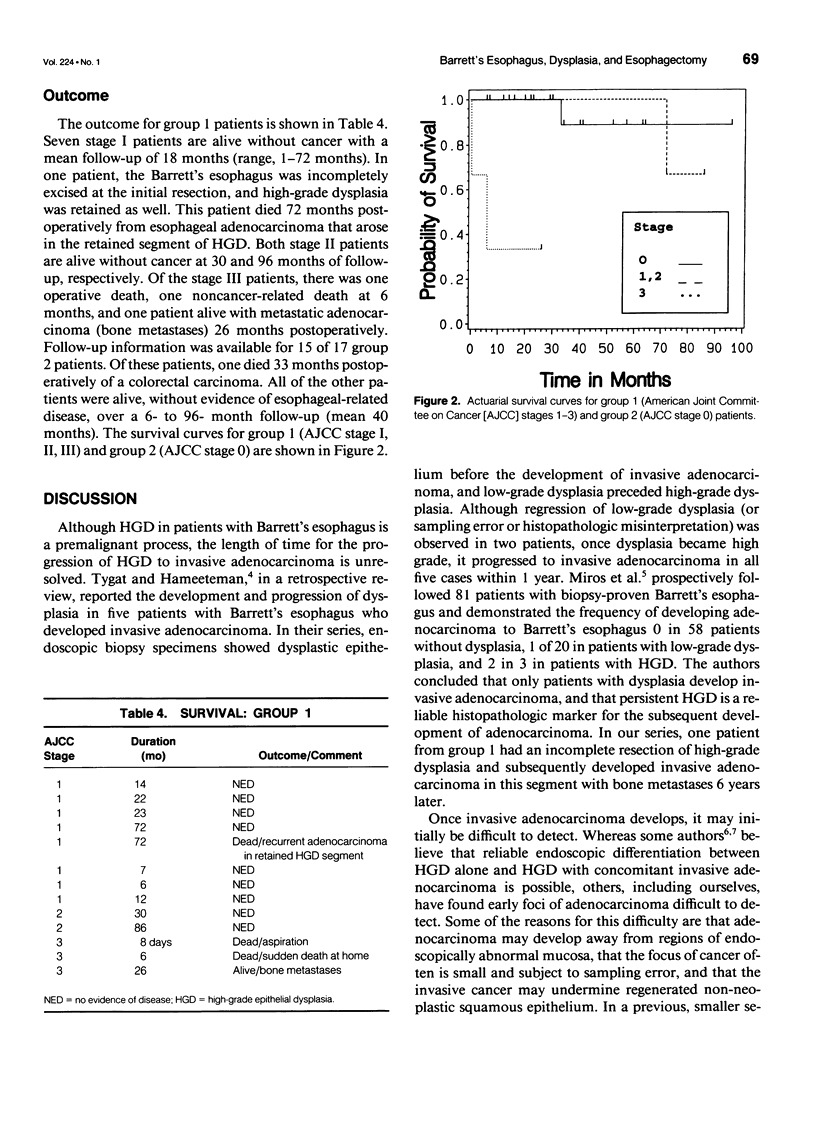
OBJECTIVE. The authors review the results and outcomes of esophagectomy (prophylactic esophagectomy) for patients with Barrett's esophagus and high-grade epithelial dysplasia (HGD). SUMMARY BACKGROUND DATA. The role of prophylactic esophagectomy for Barrett's esophagus with HGD is controversial, with some authors recommending surgery and others favoring endoscopic surveillance until biopsy diagnosis of carcinoma is made. METHODS. Between 1982 and 1994, 30 consecutive patients with HGD underwent esophagectomy and had the pre- and postoperative pathology reviewed at our institution. The medical records were reviewed to determine patient characteristics, preoperative endoscopic data, surgical approach, operative morbidity and mortality, length of hospitalization, and treatment outcome. Patients were divided into two groups based on whether invasive adenocarcinoma was found in the resection specimen (group 1) or not (group 2). RESULTS. The duration of reflux symptoms was 22 +/- 14 years for group 1 and 9 +/- 11 years for group 2 (p = 0.05). There was one operative death (3.3%) and six complications (20%). In 13 patients (43%, group 1), invasive adenocarcinoma was found in the resected esophagus. The American Joint Committee on Cancer stage for these patients was stage I (8 patients), stage II (2 patients), and stage III (3 patients). One stage I patient died of adenocarcinoma (72 months) in an incompletely excised HGD segment. Other stage I and II patients are alive without adenocarcinoma with an 18-and 63-month mean follow-up, respectively. Outcome for stage III patients was one operative death, one noncancer death (6 months), and one patient with metastatic adenocarcinoma (26 months). For group 2 (57%), there were no adenocarcinoma deaths (40 months). CONCLUSIONS. High-grade epithelial dysplasia is an indication for esophagectomy because of the prevalence of occult adenocarcinoma (43%). Esophagectomy can be performed safely, and survival in patients with completely resected Barrett's esophagus and early-stage adenocarcinoma is excellent.
Full text
PDF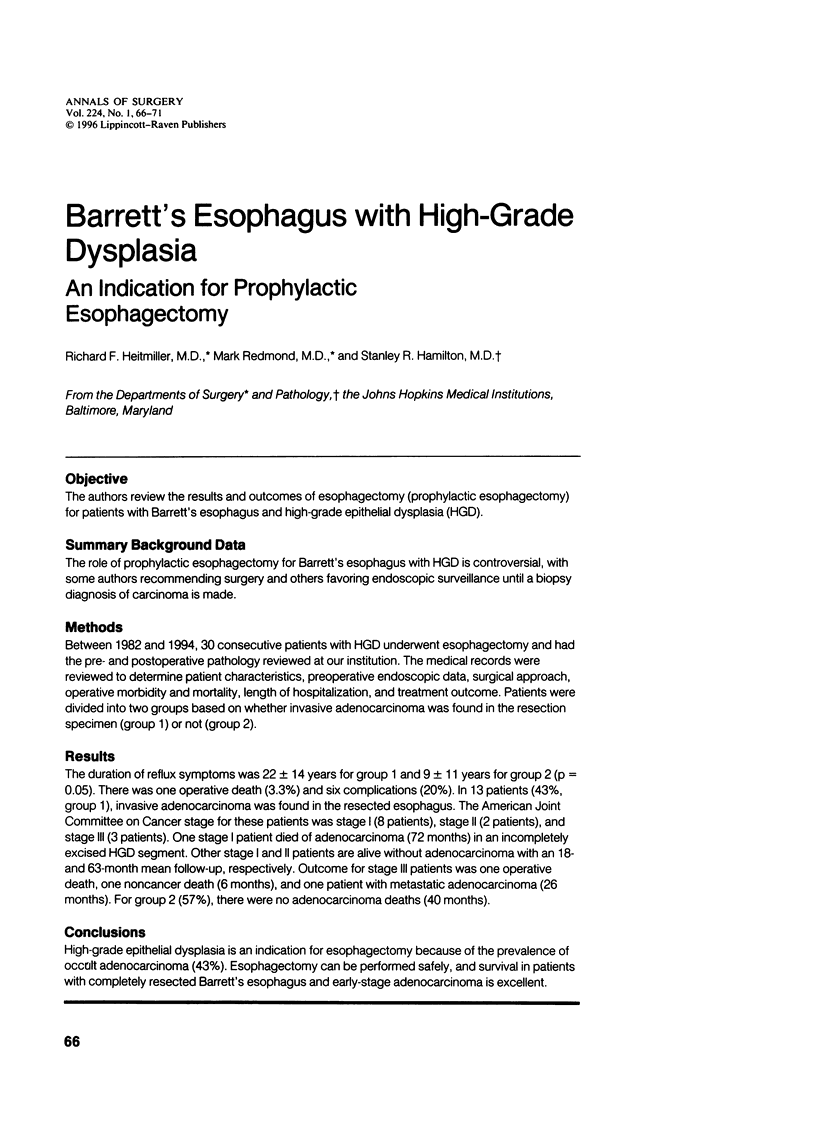


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Altorki N. K., Sunagawa M., Little A. G., Skinner D. B. High-grade dysplasia in the columnar-lined esophagus. Am J Surg. 1991 Jan;161(1):97–100. doi: 10.1016/0002-9610(91)90367-m. [DOI] [PubMed] [Google Scholar]
- Falk G. W., Catalano M. F., Sivak M. V., Jr, Rice T. W., Van Dam J. Endosonography in the evaluation of patients with Barrett's esophagus and high-grade dysplasia. Gastrointest Endosc. 1994 Mar-Apr;40(2 Pt 1):207–212. doi: 10.1016/s0016-5107(94)70168-7. [DOI] [PubMed] [Google Scholar]
- Hamilton S. R., Hutcheon D. F., Ravich W. J., Cameron J. L., Paulson M. Adenocarcinoma in Barrett's esophagus after elimination of gastroesophageal reflux. Gastroenterology. 1984 Feb;86(2):356–360. [PubMed] [Google Scholar]
- Hamilton S. R., Smith R. R. The relationship between columnar epithelial dysplasia and invasive adenocarcinoma arising in Barrett's esophagus. Am J Clin Pathol. 1987 Mar;87(3):301–312. doi: 10.1093/ajcp/87.3.301. [DOI] [PubMed] [Google Scholar]
- Levine D. S., Haggitt R. C., Blount P. L., Rabinovitch P. S., Rusch V. W., Reid B. J. An endoscopic biopsy protocol can differentiate high-grade dysplasia from early adenocarcinoma in Barrett's esophagus. Gastroenterology. 1993 Jul;105(1):40–50. doi: 10.1016/0016-5085(93)90008-z. [DOI] [PubMed] [Google Scholar]
- Miros M., Kerlin P., Walker N. Only patients with dysplasia progress to adenocarcinoma in Barrett's oesophagus. Gut. 1991 Dec;32(12):1441–1446. doi: 10.1136/gut.32.12.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pera M., Trastek V. F., Carpenter H. A., Allen M. S., Deschamps C., Pairolero P. C. Barrett's esophagus with high-grade dysplasia: an indication for esophagectomy? Ann Thorac Surg. 1992 Aug;54(2):199–204. doi: 10.1016/0003-4975(92)91370-o. [DOI] [PubMed] [Google Scholar]
- Reid B. J., Weinstein W. M., Lewin K. J., Haggitt R. C., VanDeventer G., DenBesten L., Rubin C. E. Endoscopic biopsy can detect high-grade dysplasia or early adenocarcinoma in Barrett's esophagus without grossly recognizable neoplastic lesions. Gastroenterology. 1988 Jan;94(1):81–90. doi: 10.1016/0016-5085(88)90613-0. [DOI] [PubMed] [Google Scholar]
- Tytgat G. N., Hameeteman W. The neoplastic potential of columnar-lined (Barrett's) esophagus. World J Surg. 1992 Mar-Apr;16(2):308–312. doi: 10.1007/BF02071538. [DOI] [PubMed] [Google Scholar]


