Abstract
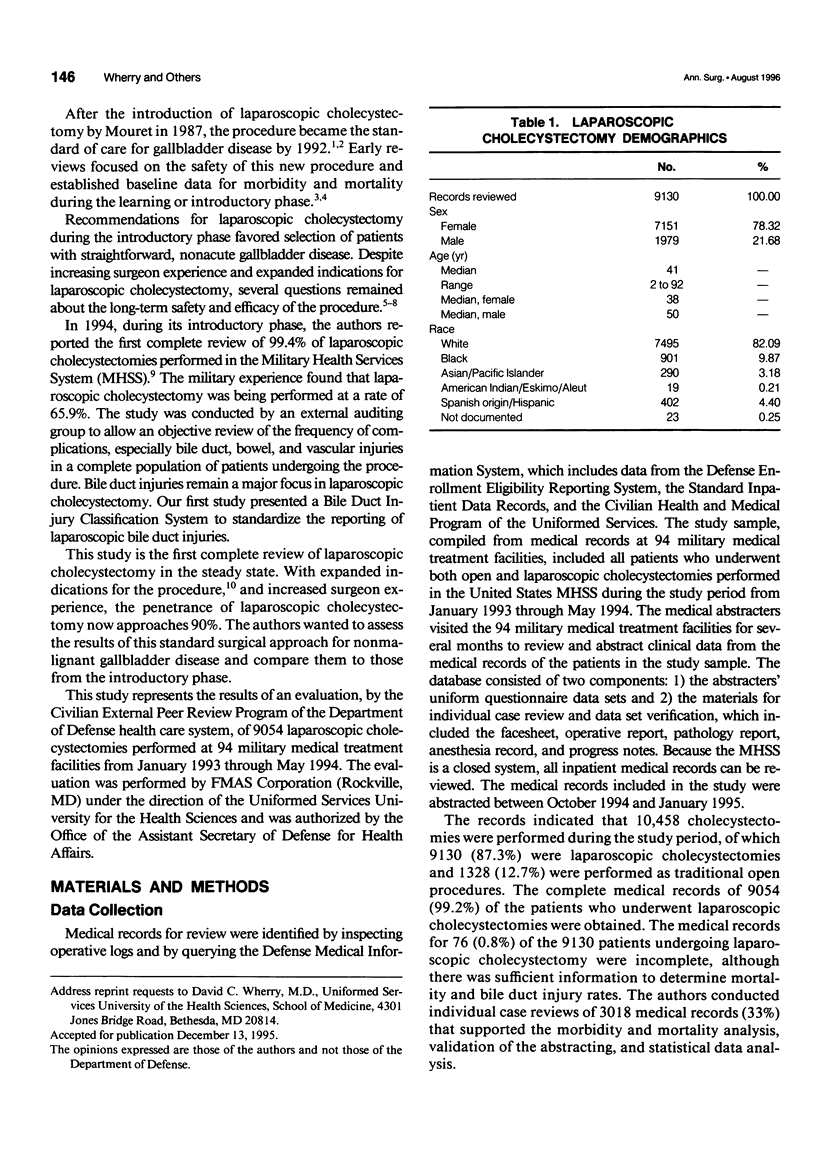
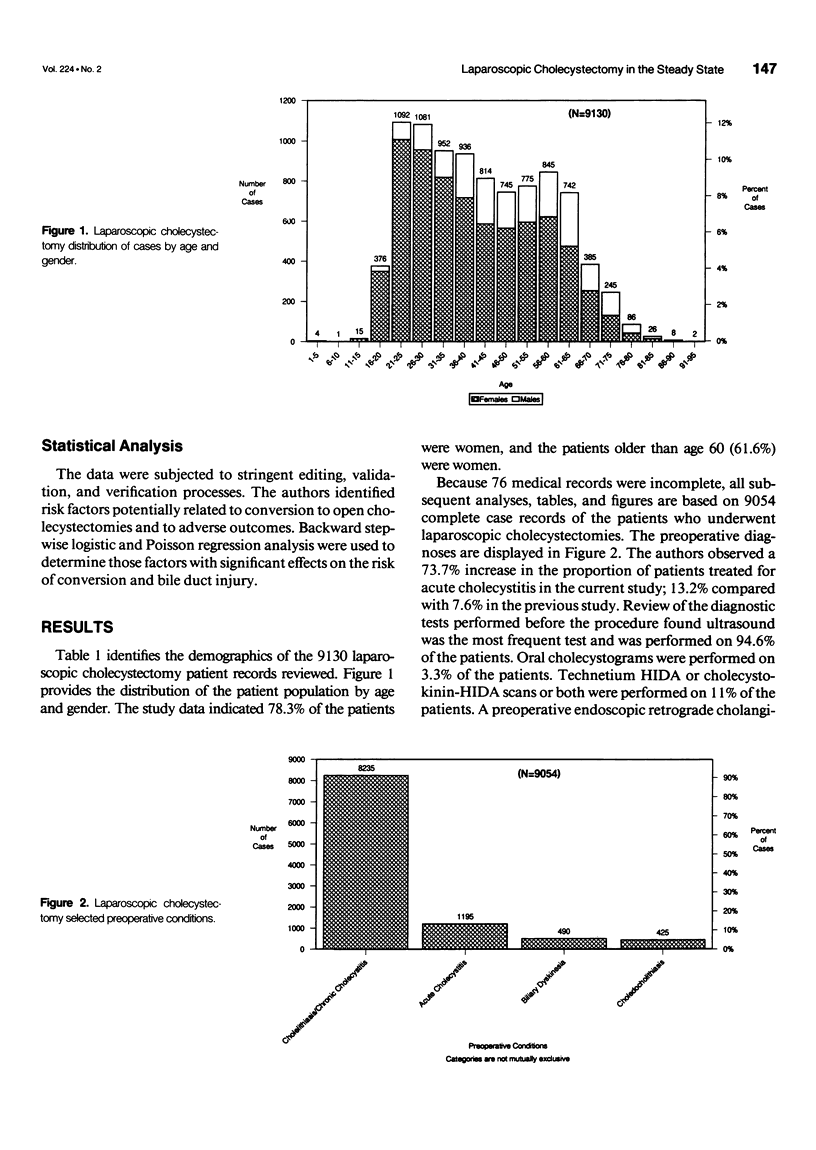
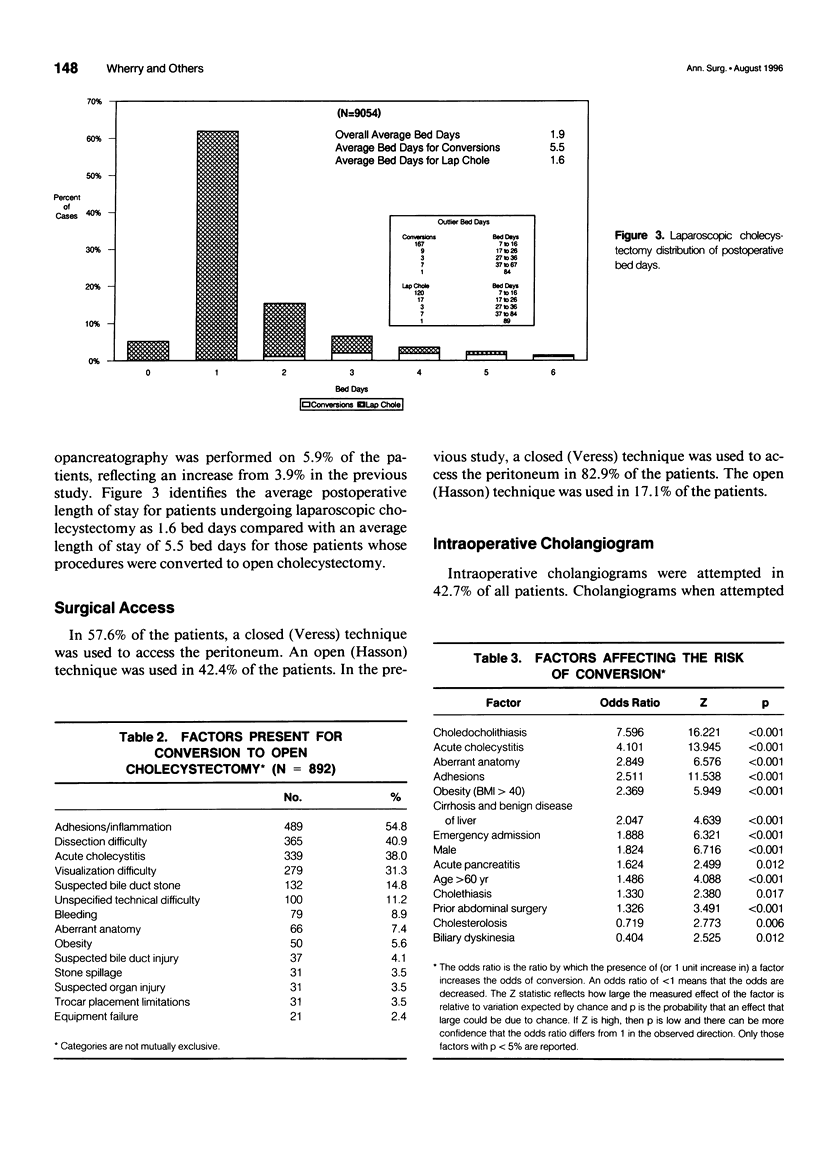
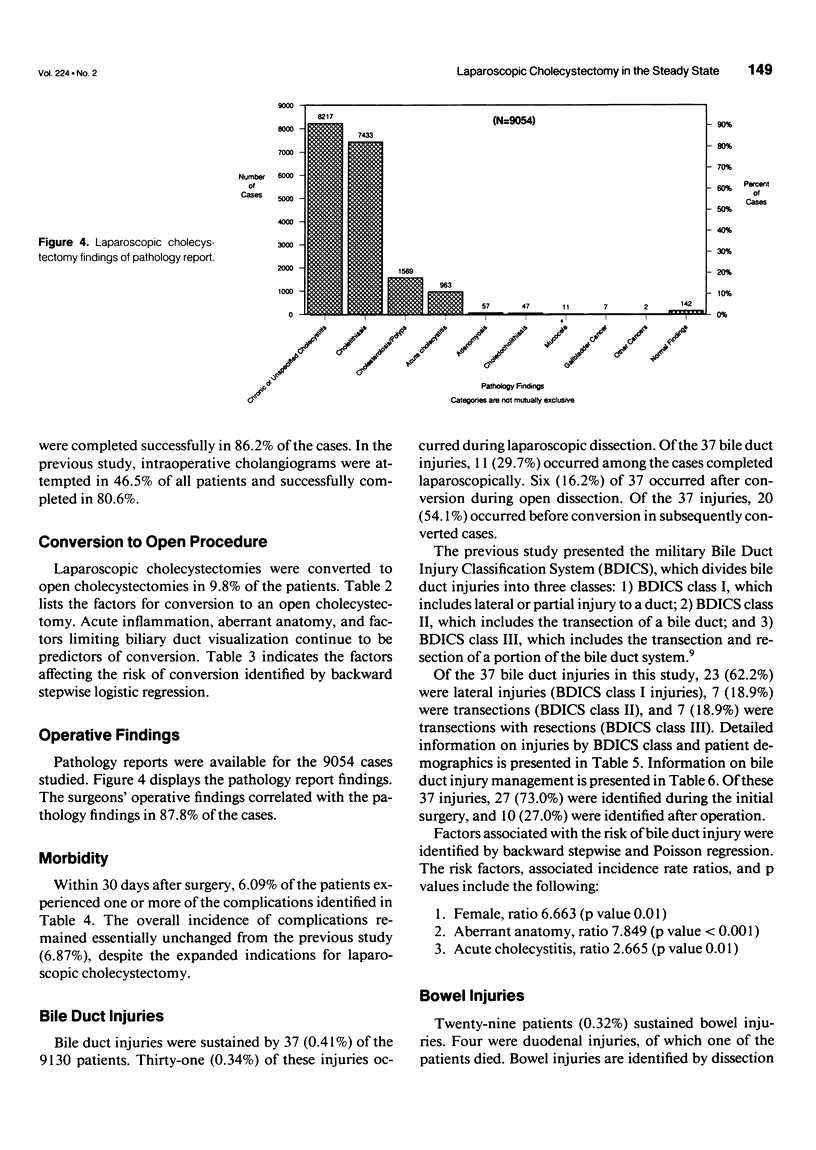
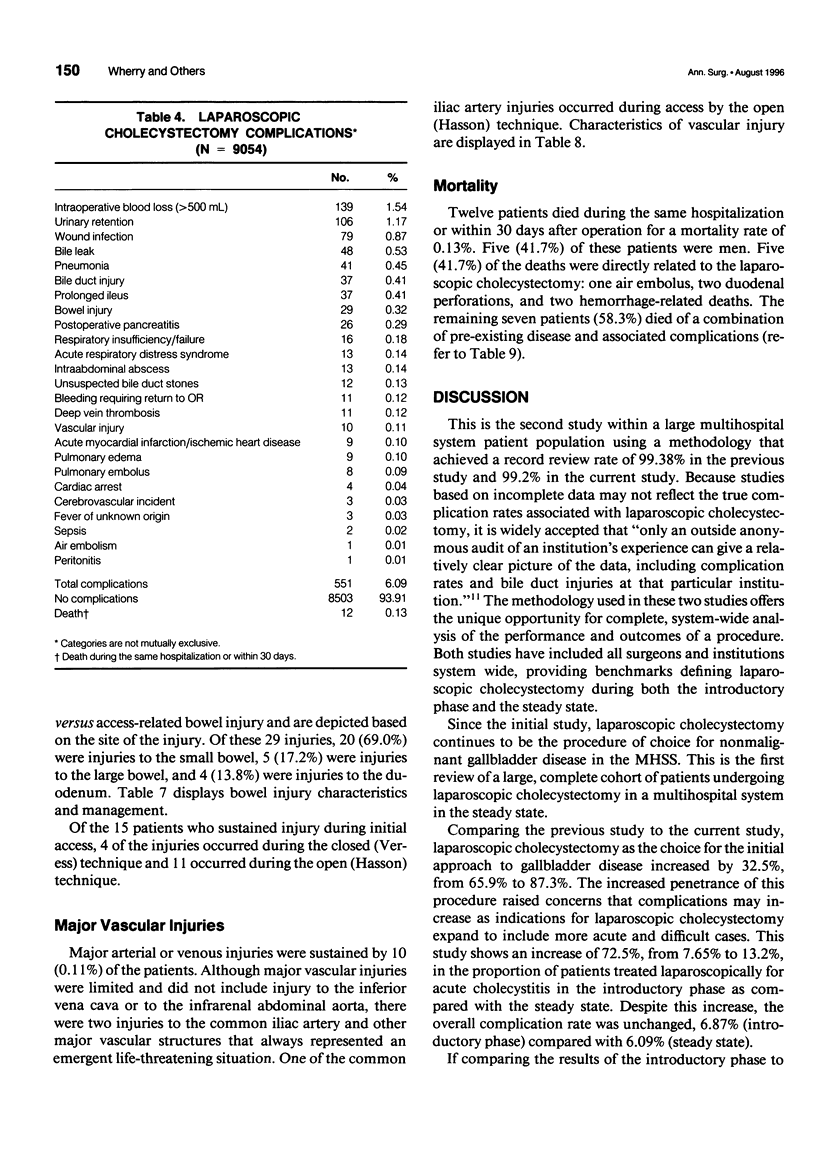
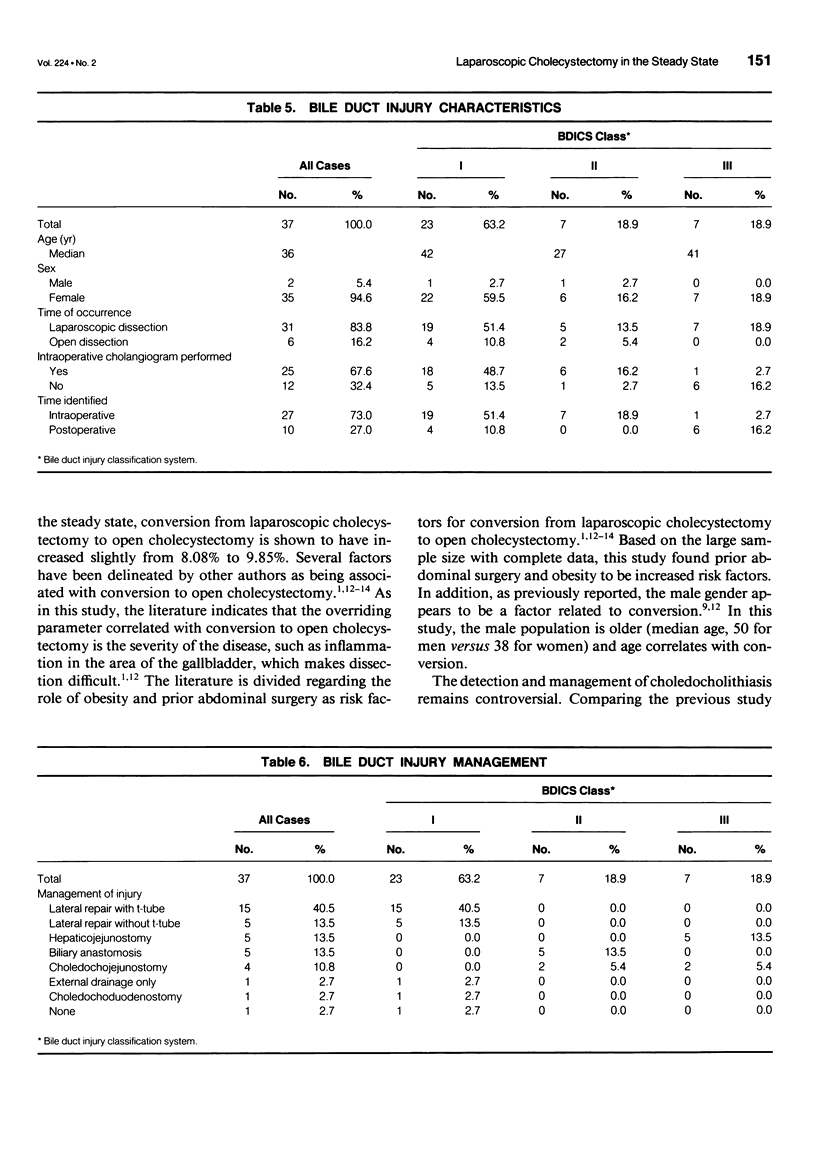
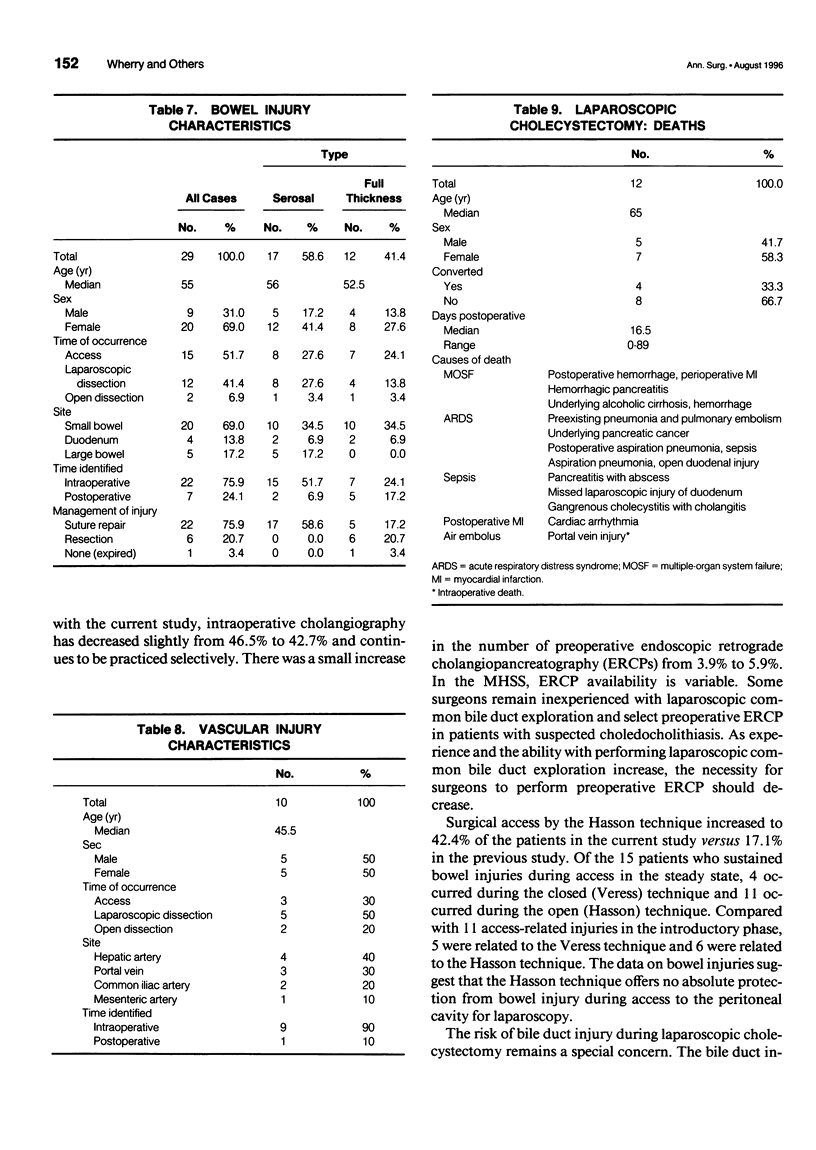
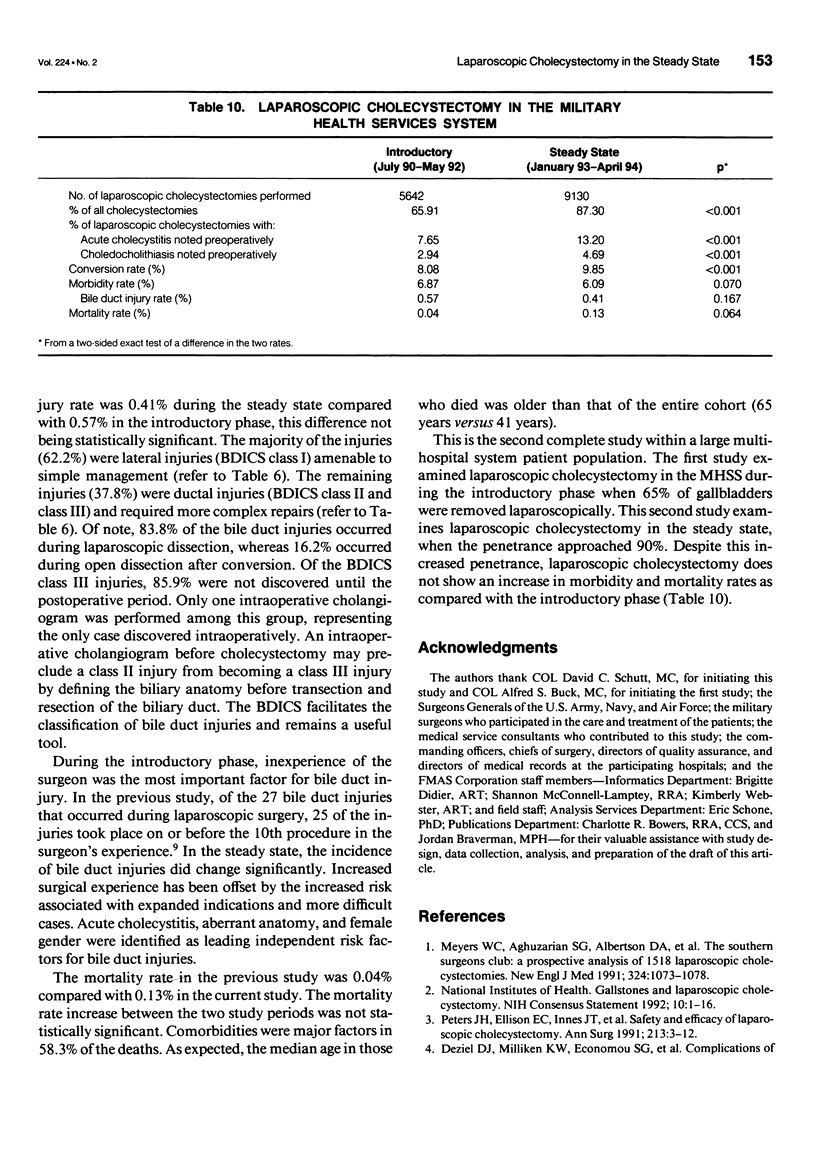
OBJECTIVE: This study provides the first objective assessment of a complete patient population undergoing laparoscopic cholecystectomy in the steady state. The authors determined the frequency of complications, particularly bile duct, bowel, vascular injuries, and deaths. SUMMARY BACKGROUND DATA: This retrospective study, conducted for the Department of Defense healthcare system by the Civilian External Peer Review Program, is the second complete audit of laparoscopic cholecystectomy. Data were collected on 9130 patients undergoing laparoscopic cholecystectomy between January 1993 and May 1994. METHODS: The study sample consisted of clinical data abstracted from the complete records of 9054 (99.2%) of the 9130 laparoscopic cholecystectomies performed at 94 military medical treatment facilities. RESULTS: Of 10,458 cholecystectomies performed in the Military Health Services System, 9130 (87.3%) were laparoscopic and 1328 (12.7%) were traditional open procedures. Seventy-six medical records were incomplete: however, there was sufficient data to determine mortality and bile duct injury rates. Of the remaining 9054 cases, 6.09% experienced complications, including bile duct (0.41%), bowel (0.32%), and vascular injuries (0.10 percent). The mortality rate was 0.13%. Access via Veress technique was used in 57.6% and Hasson technique in 42.4% of patients. Intraoperative cholangiograms were performed in 42.7% of the cases with a success rate of 86.2%. Eight hundred ninety-two (9.8%) patients were converted to open cholecystectomies. CONCLUSIONS: In the steady state, despite an increase in the percentage of laparoscopic cholecystectomies performed for nonmalignant gallbladder disease, there continues to be minimal complications and low mortality.
Full text
PDF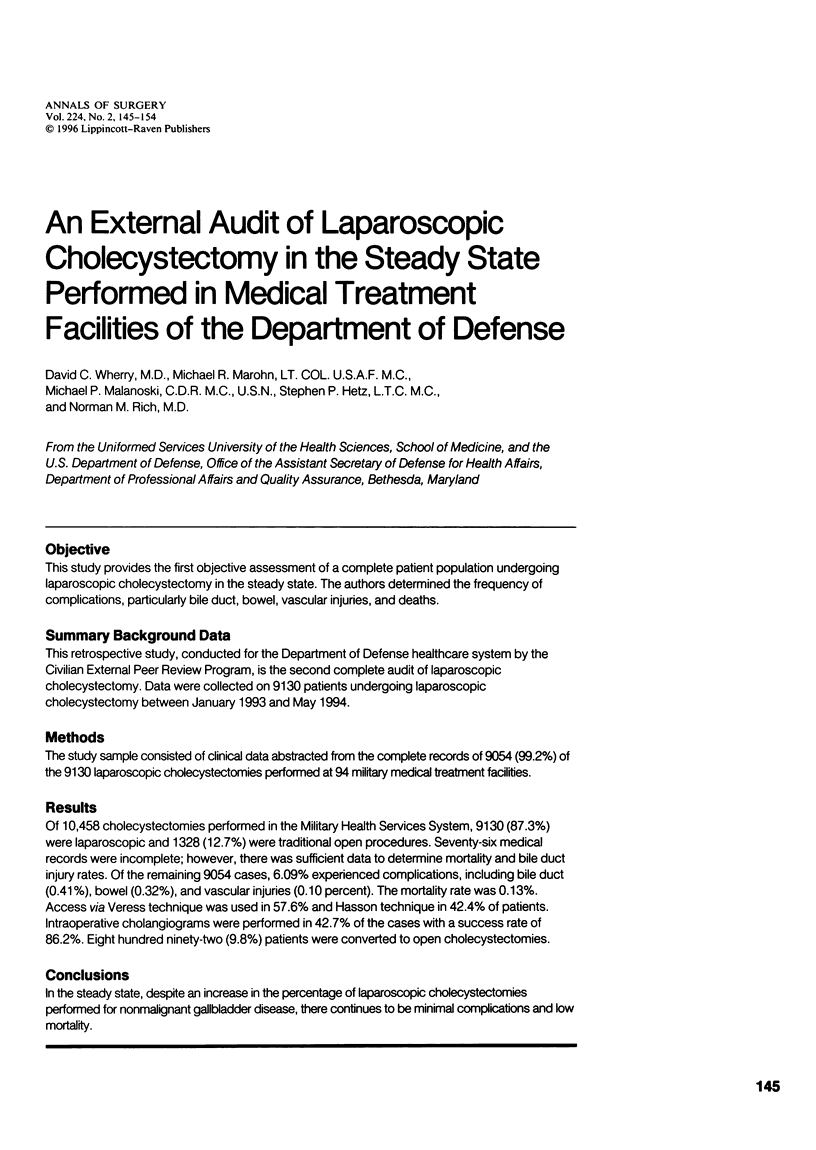

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med. 1991 Apr 18;324(16):1073–1078. doi: 10.1056/NEJM199104183241601. [DOI] [PubMed] [Google Scholar]
- Airan M., Appel M., Berci G., Coburg A. J., Cohen M., Cuschieri A., Dent T., Duppler D., Easter D., Greene F. Retrospective and prospective multi-institutional laparoscopic cholecystectomy study organized by the Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc. 1992 Jul-Aug;6(4):169–178. doi: 10.1007/BF02210874. [DOI] [PubMed] [Google Scholar]
- Cates J. A., Tompkins R. K., Zinner M. J., Busuttil R. W., Kallman C., Roslyn J. J. Biliary complications of laparoscopic cholecystectomy. Am Surg. 1993 Apr;59(4):243–247. [PubMed] [Google Scholar]
- Deziel D. J., Millikan K. W., Economou S. G., Doolas A., Ko S. T., Airan M. C. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993 Jan;165(1):9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- Kern K. A. Medicolegal analysis of bile duct injury during open cholecystectomy and abdominal surgery. Am J Surg. 1994 Sep;168(3):217–222. doi: 10.1016/s0002-9610(05)80189-8. [DOI] [PubMed] [Google Scholar]
- Miller K., Hölbling N., Hutter J., Junger W., Moritz E., Speil T. Laparoscopic cholecystectomy for patients who have had previous abdominal surgery. Surg Endosc. 1993 Sep-Oct;7(5):400–403. doi: 10.1007/BF00311729. [DOI] [PubMed] [Google Scholar]
- Moossa A. R., Easter D. W., Van Sonnenberg E., Casola G., D'Agostino H. Laparoscopic injuries to the bile duct. A cause for concern. Ann Surg. 1992 Mar;215(3):203–208. doi: 10.1097/00000658-199203000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters J. H., Ellison E. C., Innes J. T., Liss J. L., Nichols K. E., Lomano J. M., Roby S. R., Front M. E., Carey L. C. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991 Jan;213(1):3–12. doi: 10.1097/00000658-199101000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters J. H., Krailadsiri W., Incarbone R., Bremner C. G., Froes E., Ireland A. P., Crookes P., Ortega A. E., Anthone G. A., Stain S. A. Reasons for conversion from laparoscopic to open cholecystectomy in an urban teaching hospital. Am J Surg. 1994 Dec;168(6):555–559. doi: 10.1016/s0002-9610(05)80121-7. [DOI] [PubMed] [Google Scholar]
- Schirmer B. D., Dix J., Edge S. B., Hyser M. J., Hanks J. B., Aguilar M. Laparoscopic cholecystectomy in the obese patient. Ann Surg. 1992 Aug;216(2):146–152. doi: 10.1097/00000658-199208000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner C. A., Bass E. B., Talamini M. A., Pitt H. A., Steinberg E. P. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med. 1994 Feb 10;330(6):403–408. doi: 10.1056/NEJM199402103300607. [DOI] [PubMed] [Google Scholar]
- Wherry D. C., Rob C. G., Marohn M. R., Rich N. M. An external audit of laparoscopic cholecystectomy performed in medical treatment facilities of the department of Defense. Ann Surg. 1994 Nov;220(5):626–634. doi: 10.1097/00000658-199411000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]


