Abstract
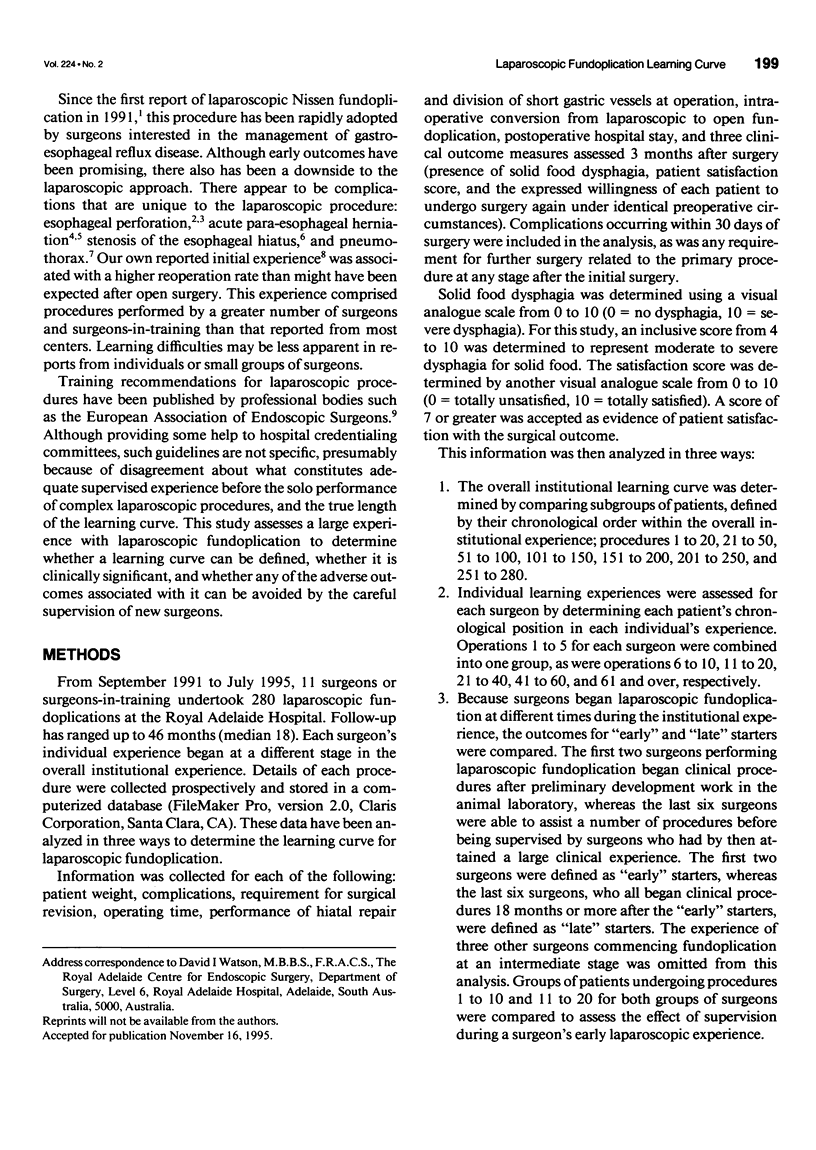
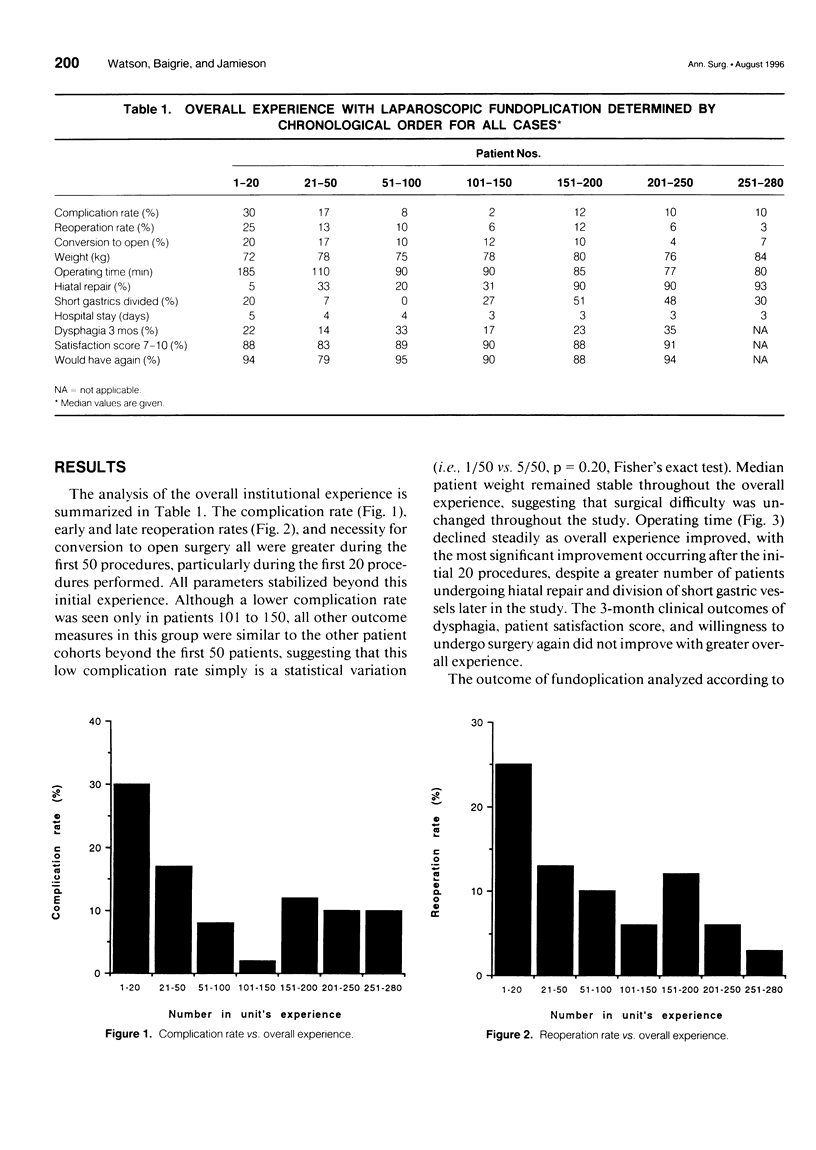
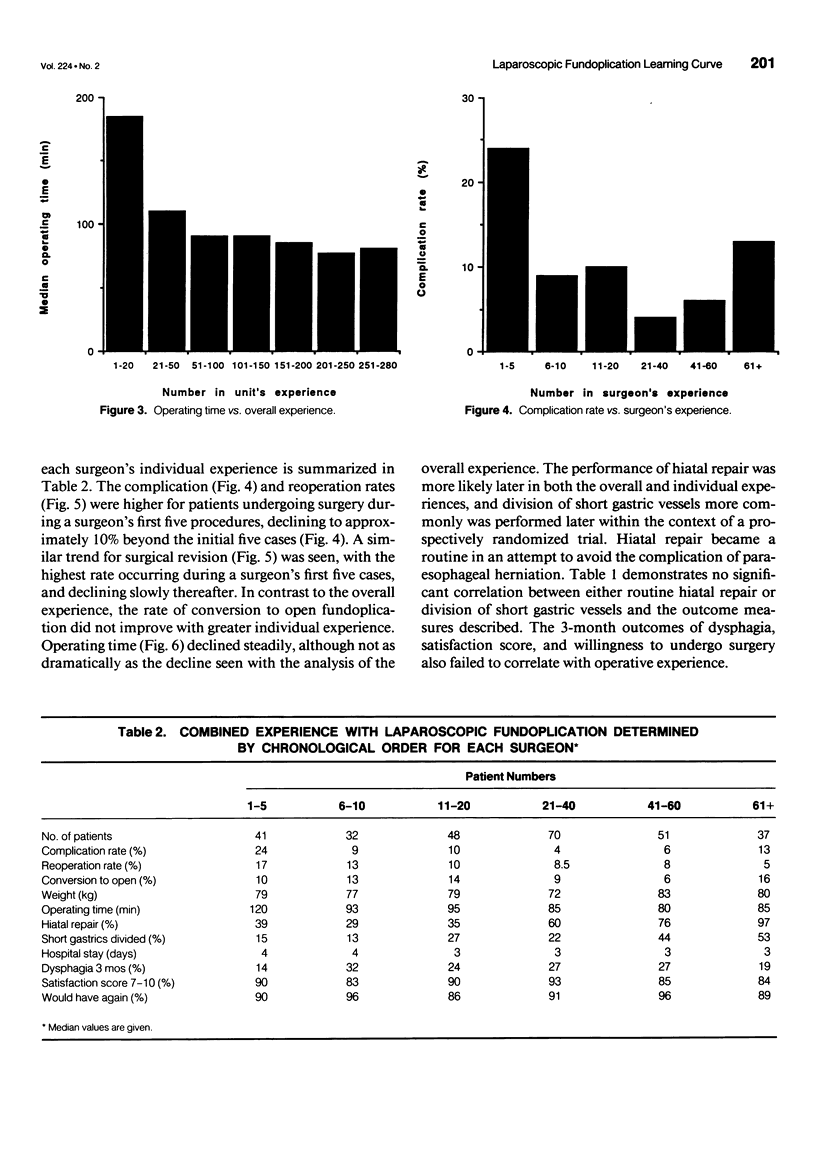
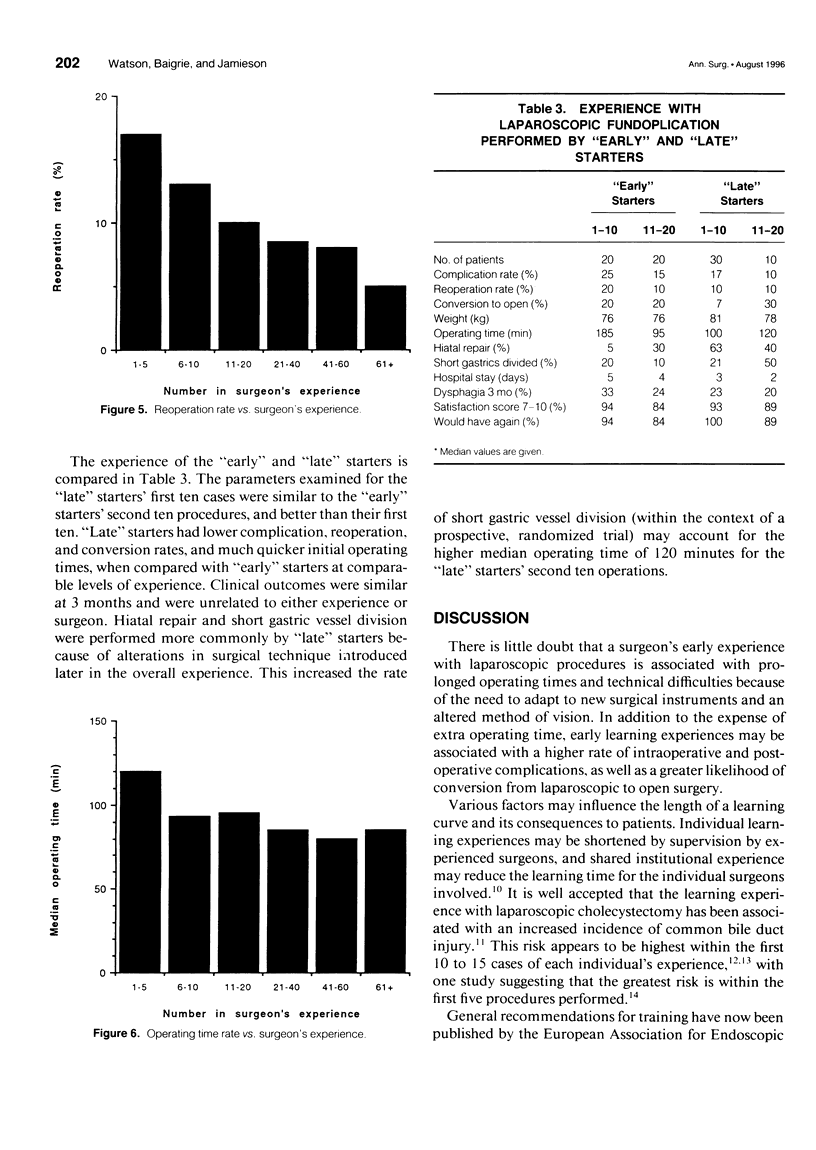
OBJECTIVE: The objective of this study was to determine whether a learning curve for laparoscopic fundoplication can be defined, and whether steps can be taken to avoid any difficulties associated with it. SUMMARY BACKGROUND DATA: Although early outcomes after laparoscopic fundoplication have been promising, complications unique to the procedure have been described. Learning curve problems may contribute to these difficulties. Although training recommendations have been published by some professional bodies, there is disagreement about what constitutes adequate supervised experience before the solo performance of laparoscopic antireflux surgery, and the true length of the learning curve. METHODS: The outcome of 280 laparoscopic fundoplications undertaken by 11 surgeons during a 46-month period was assessed prospectively. The experience was analyzed in three different ways: 1) by an assessment of the overall learning experience within chronologically arranged groups, 2) by an assessment of all individual experiences grouped according to the experience of individual surgeons, and 3) by a comparison of early outcomes of operations performed by the surgeons who initiated laparoscopic fundoplication with the early experience of surgeons beginning laparoscopic fundoplication later in the overall institutional experience. RESULTS: The complication, reoperation, and laparoscopic to open conversion rates all were higher in the first 50 cases performed by the overall group, and in the first 20 cases performed by each individual surgeon. These rates were even higher in the initial first 20 cases, and the first 5 individual cases. However, adverse outcomes were less likely when surgeons began fundoplication later in the overall experience, when experienced supervision could be provided. CONCLUSIONS: A learning curve for laparoscopic fundoplication can be defined. Experienced supervision should be sought by surgeons beginning laparoscopic fundoplication during their first 20 procedures. This should minimize adverse outcomes associated with an individual's learning curve.
Full text
PDF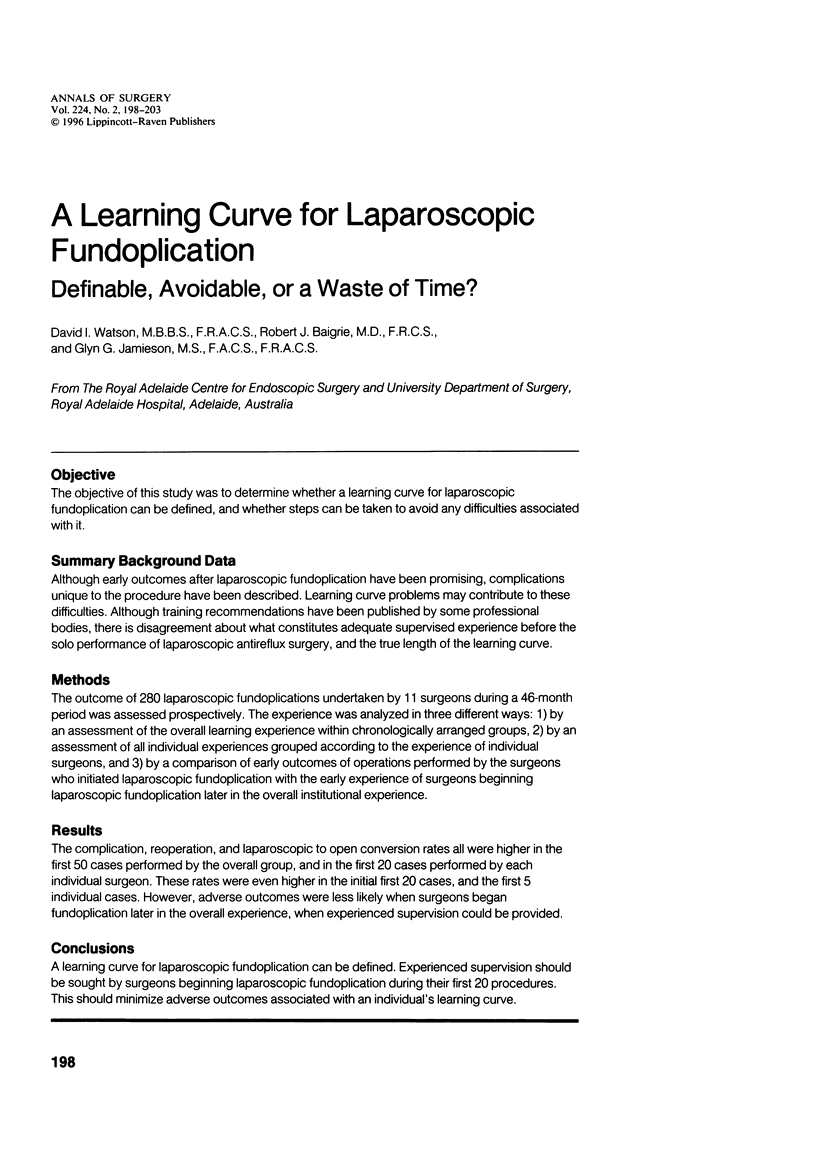

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cadière G. B. La chirurgie anti-reflux: indication, principe et apport de la coelioscopie. Rev Med Brux. 1994 Jan-Feb;15(1):25–30. [PubMed] [Google Scholar]
- Cuschieri A., Hunter J., Wolfe B., Swanstrom L. L., Hutson W. Multicenter prospective evaluation of laparoscopic antireflux surgery. Preliminary report. Surg Endosc. 1993 Nov-Dec;7(6):505–510. doi: 10.1007/BF00316690. [DOI] [PubMed] [Google Scholar]
- Dallemagne B., Weerts J. M., Jehaes C., Markiewicz S., Lombard R. Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc. 1991 Sep;1(3):138–143. [PubMed] [Google Scholar]
- Huang S. M., Wu C. W., Hong H. T., Ming-Liu, King K. L., Lui W. Y. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg. 1993 Dec;80(12):1590–1592. doi: 10.1002/bjs.1800801232. [DOI] [PubMed] [Google Scholar]
- Jamieson G. G., Watson D. I., Britten-Jones R., Mitchell P. C., Anvari M. Laparoscopic Nissen fundoplication. Ann Surg. 1994 Aug;220(2):137–145. doi: 10.1097/00000658-199408000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters J. H., Ellison E. C., Innes J. T., Liss J. L., Nichols K. E., Lomano J. M., Roby S. R., Front M. E., Carey L. C. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991 Jan;213(1):3–12. doi: 10.1097/00000658-199101000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid D. B., Winning T., Bell G. Pneumothorax during laparoscopic dissection of the diaphragmatic hiatus. Br J Surg. 1993 May;80(5):670–670. doi: 10.1002/bjs.1800800537. [DOI] [PubMed] [Google Scholar]
- Schlumpf R., Klotz H. P., Wehrli H., Herzog U. A nation's experience in laparoscopic cholecystectomy. Prospective multicenter analysis of 3722 cases. Surg Endosc. 1994 Jan;8(1):35–41. doi: 10.1007/BF02909491. [DOI] [PubMed] [Google Scholar]
- Watson D. I., Jamieson G. G., Devitt P. G., Mitchell P. C., Game P. A. Paraoesophageal hiatus hernia: an important complication of laparoscopic Nissen fundoplication. Br J Surg. 1995 Apr;82(4):521–523. doi: 10.1002/bjs.1800820428. [DOI] [PubMed] [Google Scholar]
- Watson D. I., Jamieson G. G., Mitchell P. C., Devitt P. G., Britten-Jones R. Stenosis of the esophageal hiatus following laparoscopic fundoplication. Arch Surg. 1995 Sep;130(9):1014–1016. doi: 10.1001/archsurg.1995.01430090100029. [DOI] [PubMed] [Google Scholar]
- Weerts J. M., Dallemagne B., Hamoir E., Demarche M., Markiewicz S., Jehaes C., Lombard R., Demoulin J. C., Etienne M., Ferron P. E. Laparoscopic Nissen fundoplication: detailed analysis of 132 patients. Surg Laparosc Endosc. 1993 Oct;3(5):359–364. [PubMed] [Google Scholar]
- Zucker K. A., Bailey R. W., Gadacz T. R., Imbembo A. L. Laparoscopic guided cholecystectomy. Am J Surg. 1991 Jan;161(1):36–44. doi: 10.1016/0002-9610(91)90358-k. [DOI] [PubMed] [Google Scholar]


