Abstract
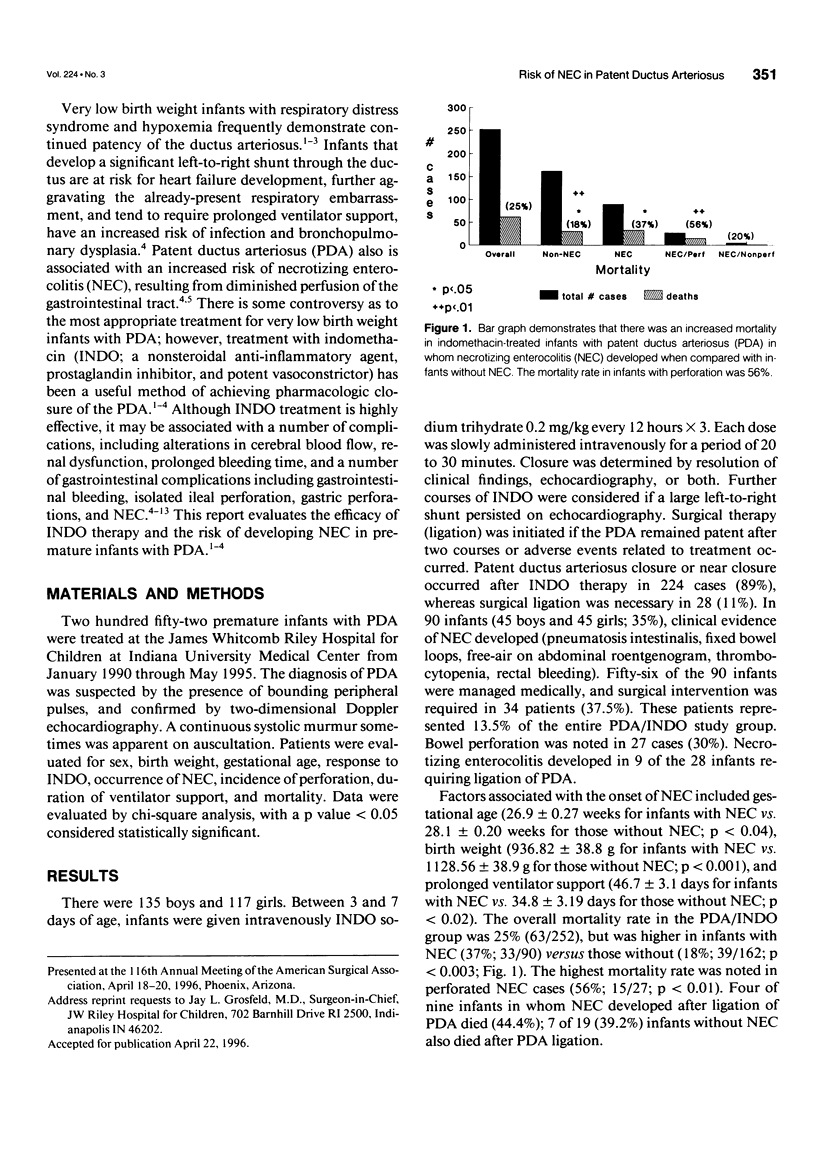
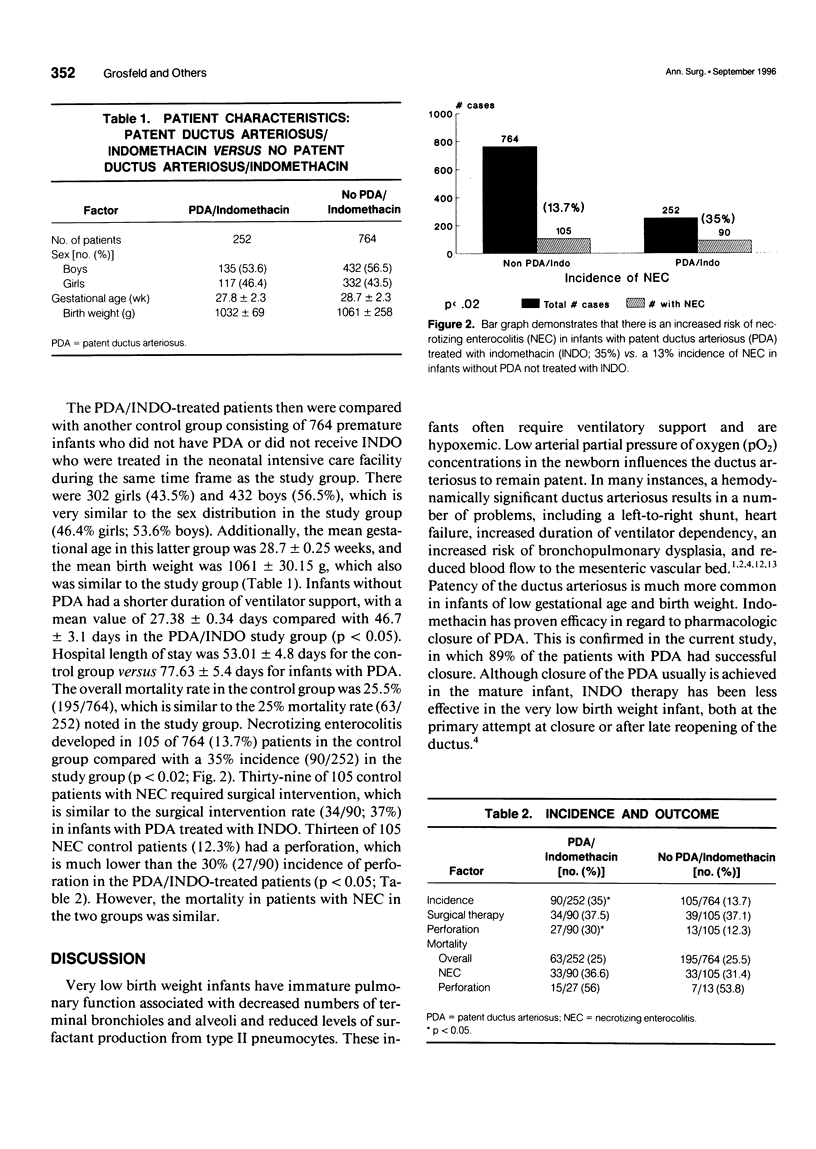
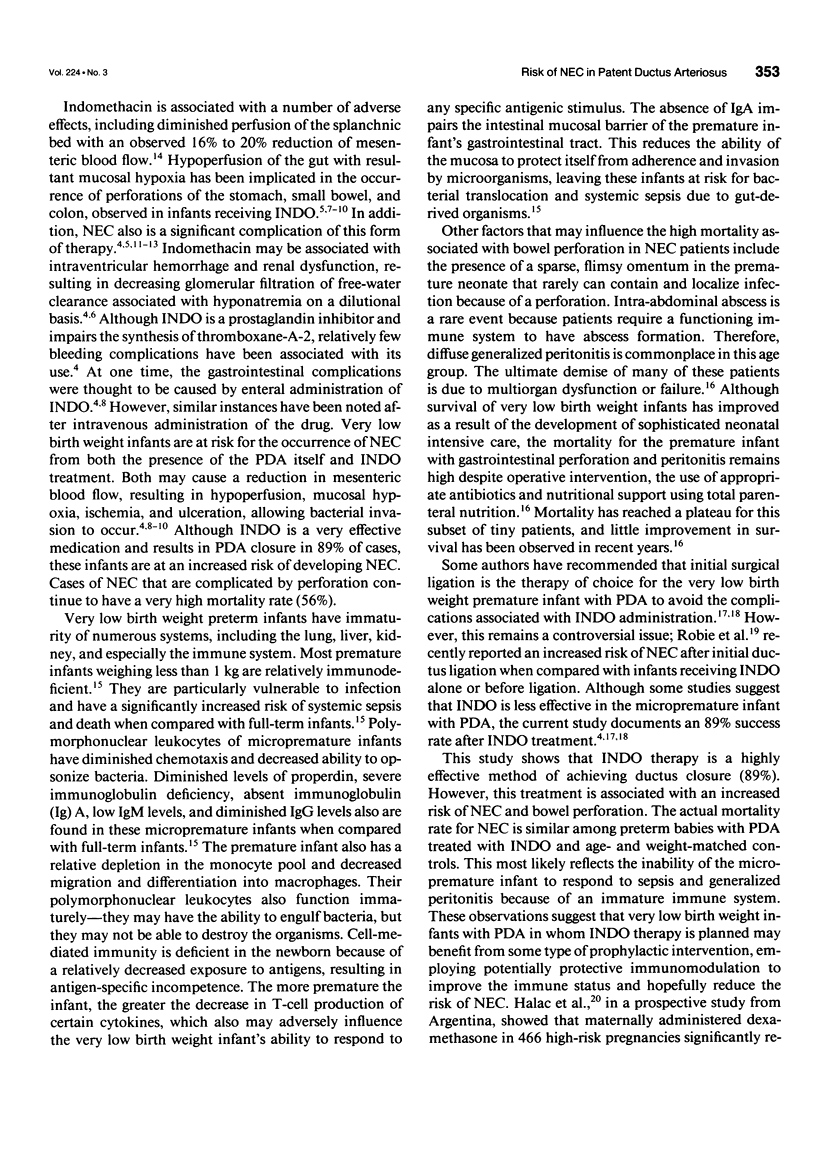
OBJECTIVE: The authors evaluated the risk of necrotizing enterocolitis (NEC) in very low birth weight infants receiving indomethacin (INDO) to close patent ductus arteriosus (PDA). BACKGROUND DATA: Controversy exists regarding the best method of managing very low birth weight infants with PDA and whether to employ medical management using INDO or surgical ligation of the ductus. METHODS: Two hundred fifty-two premature infants with symptomatic PDA were given intravenously INDO 0.2 mg/kg every 12 hours x 3 in an attempt to close the ductus. Patients were evaluated for sex, birth weight, gestational age, ductus closure, occurrence of NEC, bowel perforation, and mortality. RESULTS: There were 135 boys and 117 girls. The PDA closed or became asymptomatic in 224 cases (89%), whereas 28 (11%) required surgical ligation. Ninety infants (35%) developed evidence of NEC after INDO therapy. Fifty-six were managed medically; surgical intervention was required in 34 of 90 cases (37.8%) or 13% of the entire PDA/INDO study group. Bowel perforation was noted in 27 cases (30%). Factors associated with the onset of NEC included gestational age < 28 weeks, birth weight < 1 kg, and prolonged ventilator support. The overall mortality rate was 25.5%, but was higher in infants with NEC versus those without. The highest mortality was noted in perforated NEC cases. The PDA/INDO patients were compared with a control group of 764 infants with similar sex distribution, birth weights, and gestational ages without PDA who did not receive INDO. Necrotizing enterocolitis occurred in 105 of 764 control patients (13.7%), including 13 (12.3%) with perforation. The overall mortality rate of controls was 25%, which was similar to the overall 25.5% mortality rate in the PDA/INDO study group. CONCLUSION: These data indicate that there is increased risk of NEC and bowel perforation in premature infants with PDA receiving INDO. Mortality was higher in the PDA/INDO group with NEC than those PDA/INDO infants without NEC.
Full text
PDF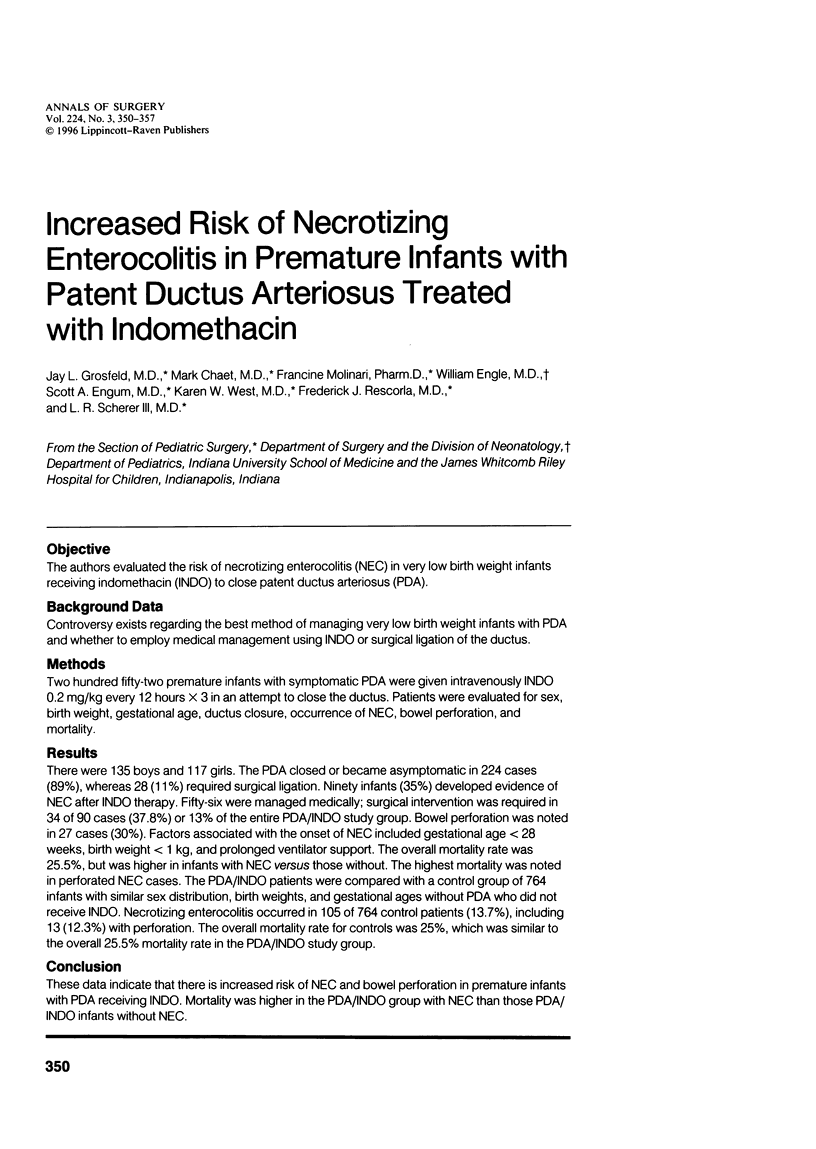


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alpan G., Eyal F., Vinograd I., Udassin R., Amir G., Mogle P., Glick B. Localized intestinal perforations after enteral administration of indomethacin in premature infants. J Pediatr. 1985 Feb;106(2):277–281. doi: 10.1016/s0022-3476(85)80305-x. [DOI] [PubMed] [Google Scholar]
- Buchheit J. Q., Stewart D. L. Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics. 1994 Jan;93(1):32–36. [PubMed] [Google Scholar]
- Coceani F., White E., Bodach E., Olley P. M. Age-dependent changes in the response of the lamb ductus arteriosus to oxygen and ibuprofen. Can J Physiol Pharmacol. 1979 Aug;57(8):825–831. doi: 10.1139/y79-126. [DOI] [PubMed] [Google Scholar]
- Du X. X., Doerschuk C. M., Orazi A., Williams D. A. A bone marrow stromal-derived growth factor, interleukin-11, stimulates recovery of small intestinal mucosal cells after cytoablative therapy. Blood. 1994 Jan 1;83(1):33–37. [PubMed] [Google Scholar]
- Eibl M. M., Wolf H. M., Fürnkranz H., Rosenkranz A. Prevention of necrotizing enterocolitis in low-birth-weight infants by IgA-IgG feeding. N Engl J Med. 1988 Jul 7;319(1):1–7. doi: 10.1056/NEJM198807073190101. [DOI] [PubMed] [Google Scholar]
- Gennari R., Alexander J. W., Gianotti L., Eaves-Pyles T., Hartmann S. Granulocyte macrophage colony-stimulating factor improves survival in two models of gut-derived sepsis by improving gut barrier function and modulating bacterial clearance. Ann Surg. 1994 Jul;220(1):68–76. doi: 10.1097/00000658-199407000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gersony W. M., Peckham G. J., Ellison R. C., Miettinen O. S., Nadas A. S. Effects of indomethacin in premature infants with patent ductus arteriosus: results of a national collaborative study. J Pediatr. 1983 Jun;102(6):895–906. doi: 10.1016/s0022-3476(83)80022-5. [DOI] [PubMed] [Google Scholar]
- Gillan E. R., Christensen R. D., Suen Y., Ellis R., van de Ven C., Cairo M. S. A randomized, placebo-controlled trial of recombinant human granulocyte colony-stimulating factor administration in newborn infants with presumed sepsis: significant induction of peripheral and bone marrow neutrophilia. Blood. 1994 Sep 1;84(5):1427–1433. [PubMed] [Google Scholar]
- Gray P. H., Pemberton P. J. Gastric perforation associated with indomethacin therapy in a pre-term infant. Aust Paediatr J. 1980 Mar;16(1):65–66. doi: 10.1111/j.1440-1754.1980.tb02490.x. [DOI] [PubMed] [Google Scholar]
- Grosfeld J. L., Cheu H., Schlatter M., West K. W., Rescorla F. J. Changing trends in necrotizing enterocolitis. Experience with 302 cases in two decades. Ann Surg. 1991 Sep;214(3):300–307. doi: 10.1097/00000658-199109000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosfeld J. L., Kamman K., Gross K., Cikrit D., Ross D., Wolfe M., Katz S., Weber T. R. Comparative effects of indomethacin, prostaglandin E1, and ibuprofen on bowel ischemia. J Pediatr Surg. 1983 Dec;18(6):738–742. doi: 10.1016/s0022-3468(83)80015-3. [DOI] [PubMed] [Google Scholar]
- Halac E., Halac J., Bégué E. F., Casañas J. M., Indiveri D. R., Petit J. F., Figueroa M. J., Olmas J. M., Rodríguez L. A., Obregón R. J. Prenatal and postnatal corticosteroid therapy to prevent neonatal necrotizing enterocolitis: a controlled trial. J Pediatr. 1990 Jul;117(1 Pt 1):132–138. doi: 10.1016/s0022-3476(05)72461-6. [DOI] [PubMed] [Google Scholar]
- Kosloske A. M. Indications for operation in necrotizing enterocolitis revisited. J Pediatr Surg. 1994 May;29(5):663–666. doi: 10.1016/0022-3468(94)90736-6. [DOI] [PubMed] [Google Scholar]
- Kühl G., Wille L., Bolkenius M., Seyberth H. W. Intestinal perforation associated with indomethacin treatment in premature infants. Eur J Pediatr. 1985 Jan;143(3):213–216. doi: 10.1007/BF00442142. [DOI] [PubMed] [Google Scholar]
- Mahony L., Carnero V., Brett C., Heymann M. A., Clyman R. I. Prophylactic indomethacin therapy for patent ductus arteriosus in very-low-birth-weight infants. N Engl J Med. 1982 Mar 4;306(9):506–510. doi: 10.1056/NEJM198203043060903. [DOI] [PubMed] [Google Scholar]
- Mavroudis C., Cook L. N., Fleischaker J. W., Nagaraj H. S., Shott R. J., Howe W. R., Gray L. A., Jr Management of patent ductus arteriosus in the premature infant: indomethacin versus ligation. Ann Thorac Surg. 1983 Nov;36(5):561–566. doi: 10.1016/s0003-4975(10)60686-8. [DOI] [PubMed] [Google Scholar]
- Maxson R. T., Jackson R. J., Smith S. D. The protective role of enteral IgA supplementation in neonatal gut origin sepsis. J Pediatr Surg. 1995 Feb;30(2):231–234. doi: 10.1016/0022-3468(95)90566-9. [DOI] [PubMed] [Google Scholar]
- Rajadurai V. S., Yu V. Y. Intravenous indomethacin therapy in preterm neonates with patent ductus arteriosus. J Paediatr Child Health. 1991 Dec;27(6):370–375. doi: 10.1111/j.1440-1754.1991.tb00422.x. [DOI] [PubMed] [Google Scholar]
- Reller M. D., Lorenz J. M., Kotagal U. R., Meyer R. A., Kaplan S. Hemodynamically significant PDA: an echocardiographic and clinical assessment of incidence, natural history, and outcome in very low birth weight infants maintained in negative fluid balance. Pediatr Cardiol. 1985;6(1):17–23. doi: 10.1007/BF02265403. [DOI] [PubMed] [Google Scholar]
- Trus T., Winthrop A. L., Pipe S., Shah J., Langer J. C., Lau G. Y. Optimal management of patent ductus arteriosus in the neonate weighing less than 800 g. J Pediatr Surg. 1993 Sep;28(9):1137–1139. doi: 10.1016/0022-3468(93)90148-e. [DOI] [PubMed] [Google Scholar]
- Vanhaesebrouck P., Thiery M., Leroy J. G., Govaert P., de Praeter C., Coppens M., Cuvelier C., Dhont M. Oligohydramnios, renal insufficiency, and ileal perforation in preterm infants after intrauterine exposure to indomethacin. J Pediatr. 1988 Oct;113(4):738–743. doi: 10.1016/s0022-3476(88)80392-5. [DOI] [PubMed] [Google Scholar]


