Abstract
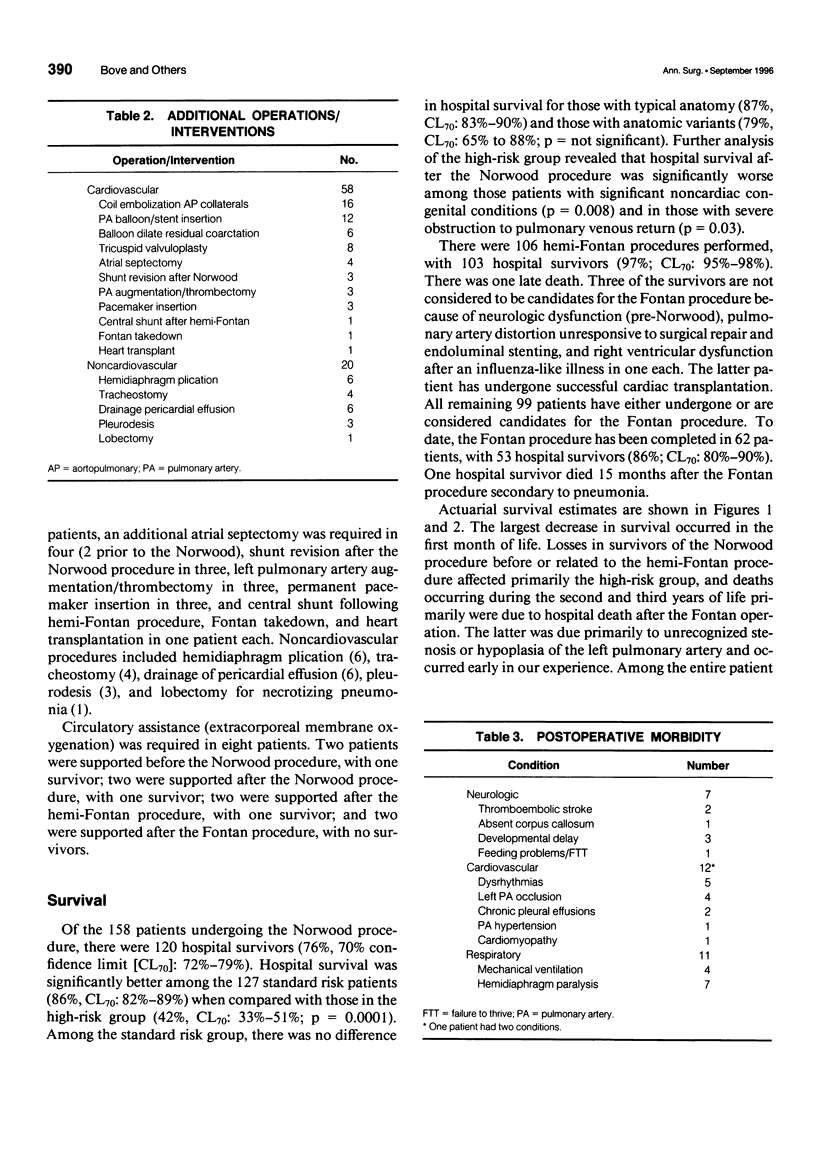
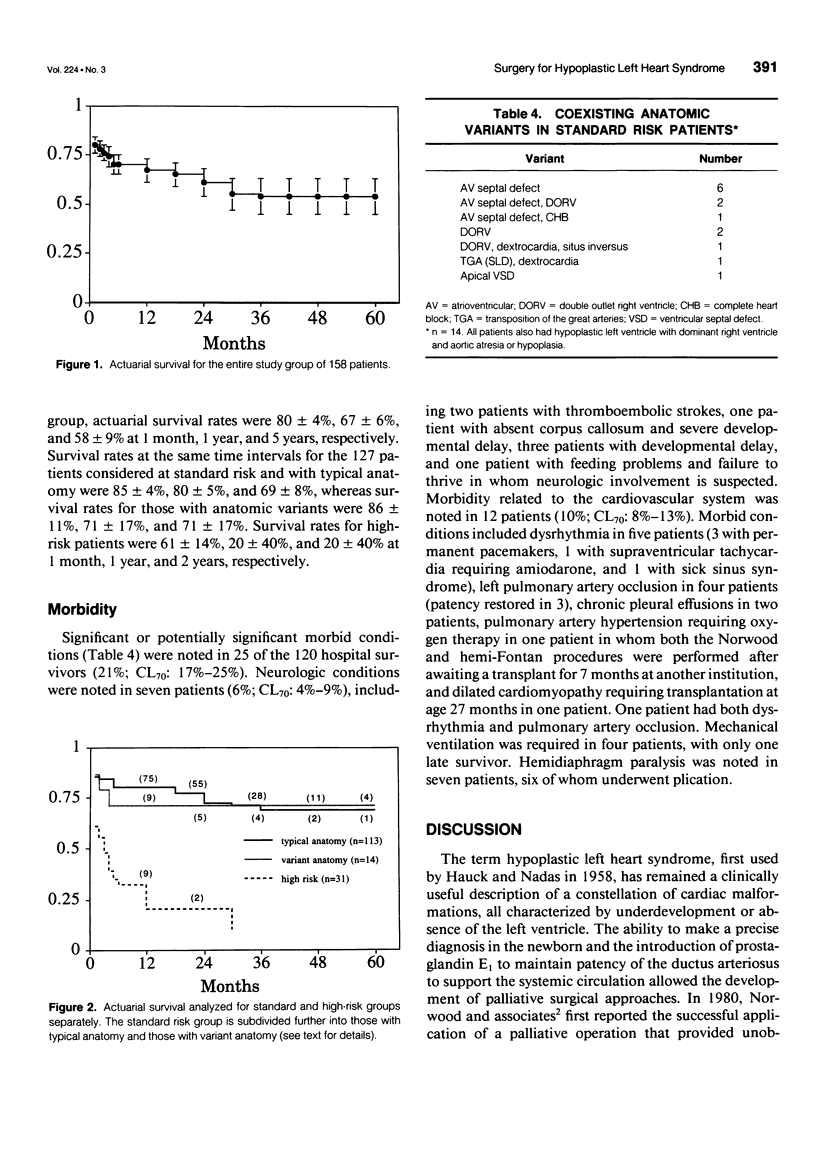
OBJECTIVE: The authors review their experience with staged reconstructive surgery for hypoplastic left heart syndrome (HLHS) and assess current outcome for this condition. SUMMARY BACKGROUND DATA: Once considered a uniformly fatal condition, the outlook for newborns with HLHS has been altered dramatically with staged reconstructive procedures. Refinements in operative technique and perioperative management have been largely responsible for this improved outlook. METHODS: The authors reviewed their experience with 158 consecutive patients undergoing stage 1 reconstruction with a Norwood procedure from January 1990 to August 1995. All patients had classic HLHS, defined as a right ventricular dependent circulation in association with atresia or severe hypoplasia of the aortic valve. RESULTS: There were 120 hospital survivors. Among the 127 patients considered at standard risk, survival was significantly higher than that for the 31 patients with important risk factors. Adverse survival was associated most strongly with significant associated noncardiac congenital conditions and severe preoperative obstruction to pulmonary venous return. Second-stage reconstruction with the hemi-Fontan procedure was performed in 106 patients, with 103 hospital survivors and one late death. Three of the late survivors were not considered candidates for the Fontan procedure. To date, the Fontan procedure has been completed in 62 patients, with 53 survivors. Deaths after the Fontan procedure occurred early in our experience and were mostly secondary to left pulmonary artery stenosis or hypoplasia. Significant or potentially significant morbid conditions were noted in 25 of the 120 hospital survivors. Neurologic conditions were found in 6% and cardiovascular conditions in 10%, including dysrhythmia, left pulmonary artery thrombosis, and chronic pleural effusions. Among the patients considered at standard risk with typical anatomy, actuarial survival was 69 +/- 8% at 5 years. Survival was 71 +/- 17% at 5 years for standard risk patients with variant anatomy and 58 +/- 9% for the entire cohort of 158 patients. The largest decrease in survival occurred in the first month of life and late deaths primarily affected those patients in the high-risk group. CONCLUSIONS: Staged reconstruction has significantly improved the intermediate-term outlook for patients with HLHS. Factors addressing improvements in early (< 1 month) first-stage survival would be expected to add significantly to an overall improved late outcome. Currently employed refinements in operative technique are associated with eliminating or reducing pulmonary artery distortion and dysrhythmia.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alboliras E. T., Chin A. J., Barber G., Helton J. G., Pigott J. D., Norwood W. I. Pulmonary artery configuration after palliative operations for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 1989 Jun;97(6):878–885. [PubMed] [Google Scholar]
- Barnea O., Austin E. H., Richman B., Santamore W. P. Balancing the circulation: theoretic optimization of pulmonary/systemic flow ratio in hypoplastic left heart syndrome. J Am Coll Cardiol. 1994 Nov 1;24(5):1376–1381. doi: 10.1016/0735-1097(94)90123-6. [DOI] [PubMed] [Google Scholar]
- Farrell P. E., Jr, Chang A. C., Murdison K. A., Baffa J. M., Norwood W. I., Murphy J. D. Outcome and assessment after the modified Fontan procedure for hypoplastic left heart syndrome. Circulation. 1992 Jan;85(1):116–122. doi: 10.1161/01.cir.85.1.116. [DOI] [PubMed] [Google Scholar]
- Glauser T. A., Rorke L. B., Weinberg P. M., Clancy R. R. Acquired neuropathologic lesions associated with the hypoplastic left heart syndrome. Pediatrics. 1990 Jun;85(6):991–1000. [PubMed] [Google Scholar]
- Glauser T. A., Rorke L. B., Weinberg P. M., Clancy R. R. Congenital brain anomalies associated with the hypoplastic left heart syndrome. Pediatrics. 1990 Jun;85(6):984–990. [PubMed] [Google Scholar]
- Gutgesell H. P., Massaro T. A. Management of hypoplastic left heart syndrome in a consortium of university hospitals. Am J Cardiol. 1995 Oct 15;76(11):809–811. doi: 10.1016/s0002-9149(99)80232-x. [DOI] [PubMed] [Google Scholar]
- Iannettoni M. D., Bove E. L., Mosca R. S., Lupinetti F. M., Dorostkar P. C., Ludomirsky A., Crowley D. C., Kulik T. J., Rosenthal A. Improving results with first-stage palliation for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 1994 Mar;107(3):934–940. [PubMed] [Google Scholar]
- Jonas R. A., Lang P., Hansen D., Hickey P., Castaneda A. R. First-stage palliation of hypoplastic left heart syndrome. The importance of coarctation and shunt size. J Thorac Cardiovasc Surg. 1986 Jul;92(1):6–13. [PubMed] [Google Scholar]
- Norwood W. I., Jr, Jacobs M. L., Murphy J. D. Fontan procedure for hypoplastic left heart syndrome. Ann Thorac Surg. 1992 Dec;54(6):1025–1030. doi: 10.1016/0003-4975(92)90065-c. [DOI] [PubMed] [Google Scholar]
- Norwood W. I., Kirklin J. K., Sanders S. P. Hypoplastic left heart syndrome: experience with palliative surgery. Am J Cardiol. 1980 Jan;45(1):87–91. doi: 10.1016/0002-9149(80)90224-6. [DOI] [PubMed] [Google Scholar]
- Pigott J. D., Murphy J. D., Barber G., Norwood W. I. Palliative reconstructive surgery for hypoplastic left heart syndrome. Ann Thorac Surg. 1988 Feb;45(2):122–128. doi: 10.1016/s0003-4975(10)62420-4. [DOI] [PubMed] [Google Scholar]
- Pridjian A. K., Mendelsohn A. M., Lupinetti F. M., Beekman R. H., 3rd, Dick M., 2nd, Serwer G., Bove E. L. Usefulness of the bidirectional Glenn procedure as staged reconstruction for the functional single ventricle. Am J Cardiol. 1993 Apr 15;71(11):959–962. doi: 10.1016/0002-9149(93)90914-x. [DOI] [PubMed] [Google Scholar]
- Rogers B. T., Msall M. E., Buck G. M., Lyon N. R., Norris M. K., Roland J. M., Gingell R. L., Cleveland D. C., Pieroni D. R. Neurodevelopmental outcome of infants with hypoplastic left heart syndrome. J Pediatr. 1995 Mar;126(3):496–498. doi: 10.1016/s0022-3476(95)70478-7. [DOI] [PubMed] [Google Scholar]


