Abstract
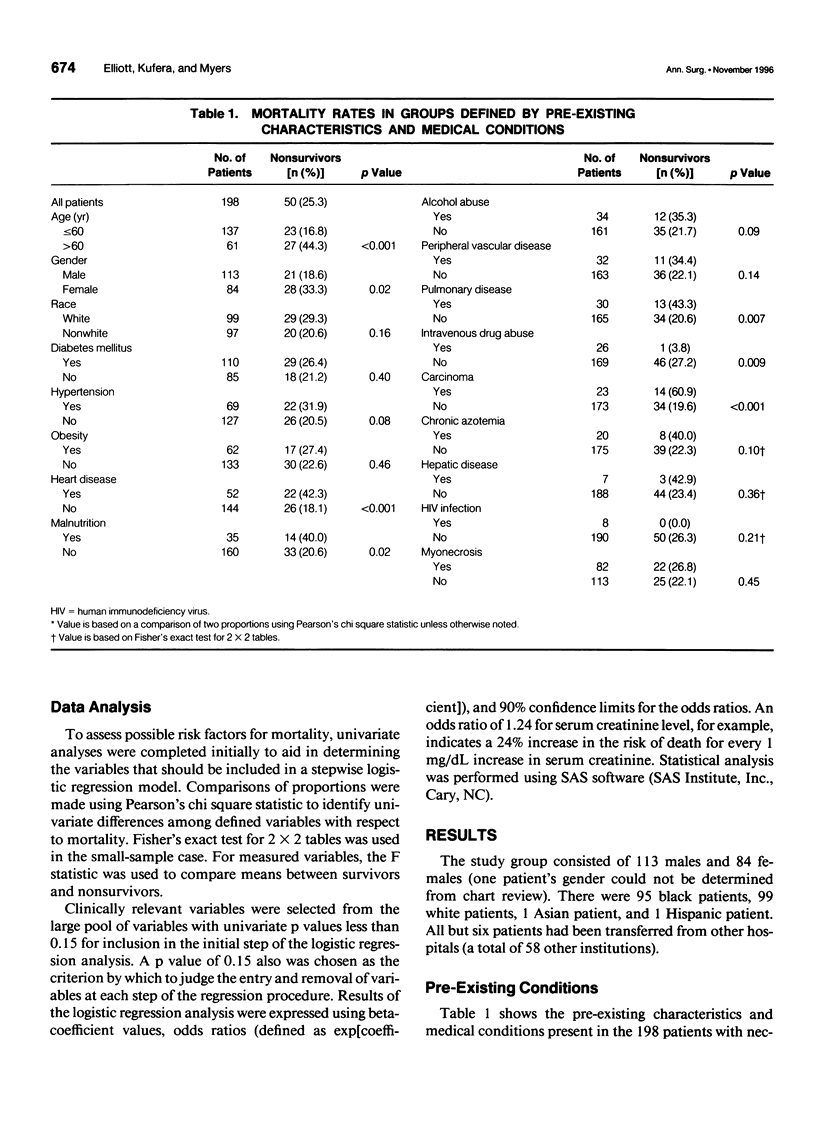
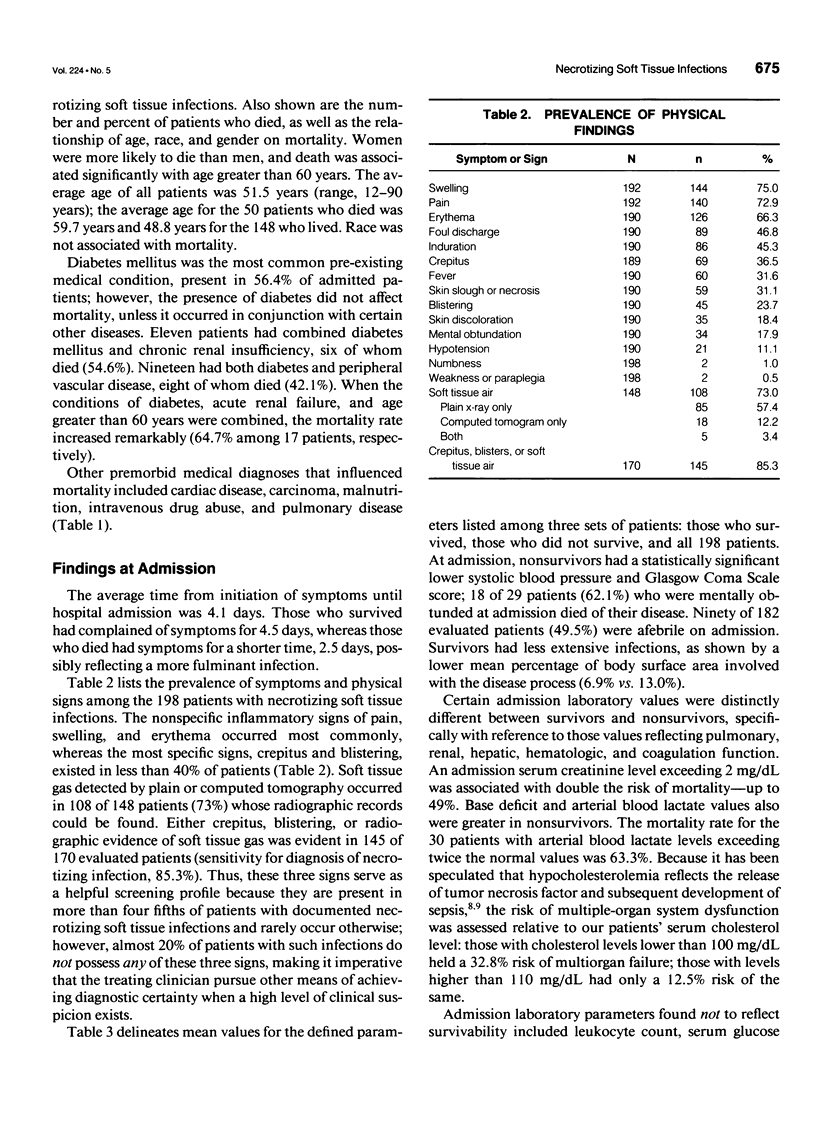
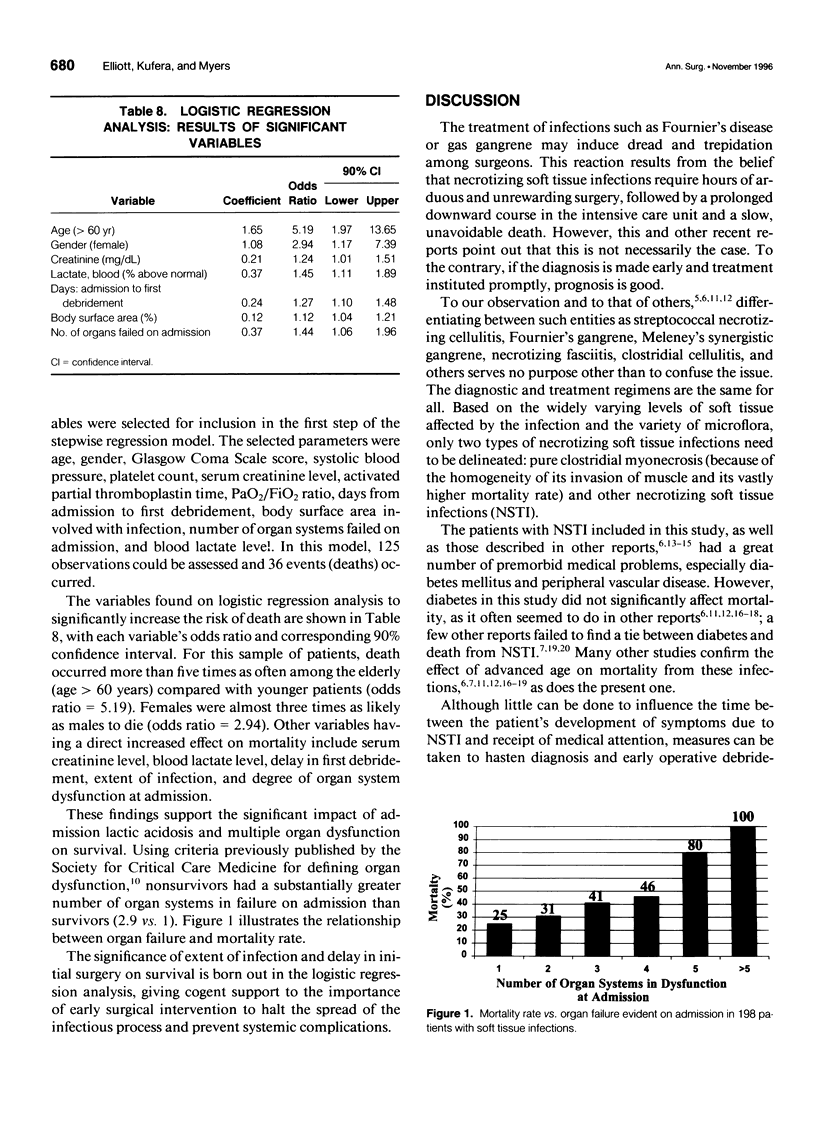
OBJECTIVE: The authors evaluate in a retrospective fashion the factors influencing outcome in a large group of patients presenting with necrotizing soft tissue infections, and, based on this analysis, propose a plan for optimal care of such patients. SUMMARY BACKGROUND DATA: In many smaller series of patients with necrotizing soft tissue infections, similar analyses of risk factors for mortality have been performed, producing conflicting conclusions regarding optimal care. In particular, debate exists regarding the impact of concurrent physiologic derangements, type and extent of infection, and the role of hyperbaric oxygen in treatment. METHODS: A retrospective chart review of 198 consecutive patients with documented necrotizing soft tissue infections, treated at a single institution during an 8-year period, was conducted. Using a model for logistic regression analysis, characteristics of each patient and his/her clinical course were tested for impact on outcome. RESULTS: The mortality rate among the 198 patients was 25.3%. The most common sites of origin of infection were the perineum (Fournier's disease; 36% of cases) and the foot (in diabetics; 15.2%). By logistic regression analysis, risk factors for death included age, female gender, extent of infection, delay in first debridement, elevated serum creatinine level, elevated blood lactate level, and degree of organ system dysfunction at admission. Diabetes mellitus did not predispose patients to death, except in conjunction with renal dysfunction or peripheral vascular disease. Myonecrosis, noted in 41.4% of the patients who underwent surgery, did not influence mortality. CONCLUSIONS: Necrotizing soft tissue infections represent a group of highly lethal infections best treated by early and repeated extensive debridement and broad-spectrum antibiotics. Hyperbaric oxygen appears to offer the advantage of early wound closure. Certain markers predict those individuals at increased risk for multiple-organ failure and death and therefore assist in deciding allocation of intensive care resources.
Full text
PDF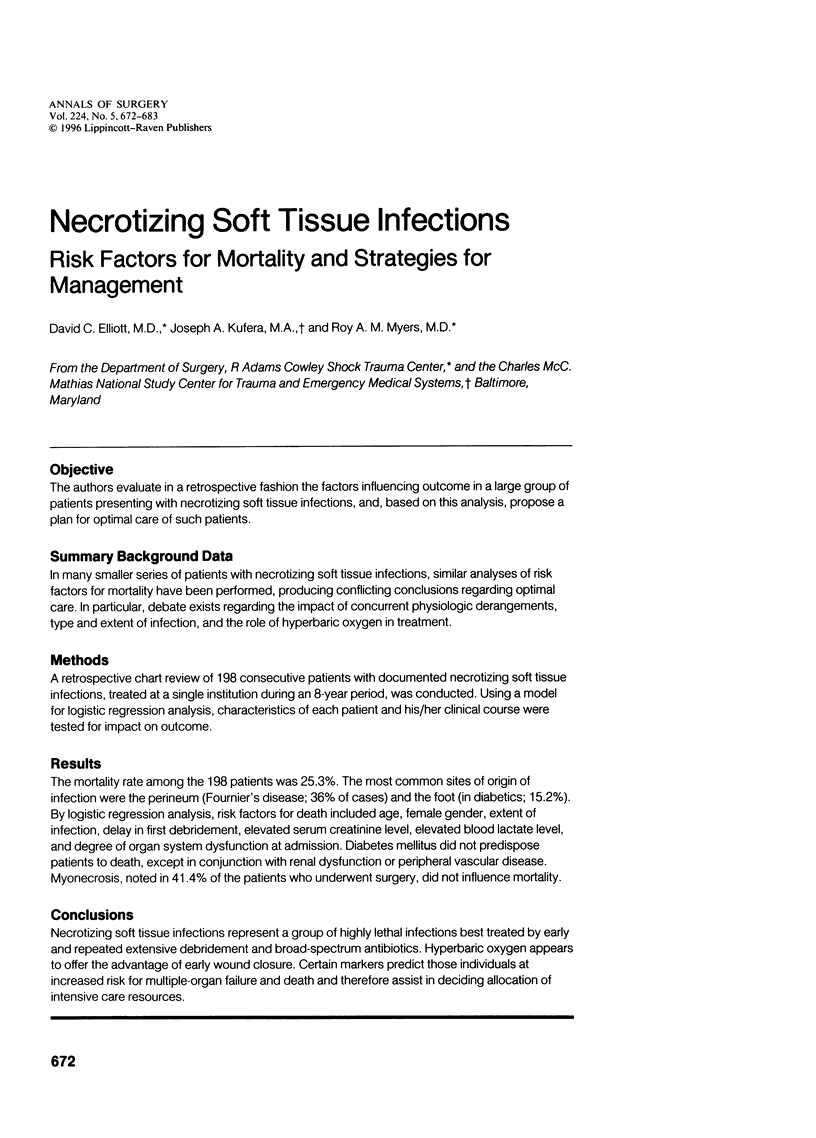


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asfar S. K., Baraka A., Juma T., Ma'Rafie A., Aladeen T., al Sayer H. Necrotizing fasciitis. Br J Surg. 1991 Jul;78(7):838–840. doi: 10.1002/bjs.1800780722. [DOI] [PubMed] [Google Scholar]
- Baskin L. S., Carroll P. R., Cattolica E. V., McAninch J. W. Necrotising soft tissue infections of the perineum and genitalia. Bacteriology, treatment and risk assessment. Br J Urol. 1990 May;65(5):524–529. doi: 10.1111/j.1464-410x.1990.tb14801.x. [DOI] [PubMed] [Google Scholar]
- Clayton M. D., Fowler J. E., Jr, Sharifi R., Pearl R. K. Causes, presentation and survival of fifty-seven patients with necrotizing fasciitis of the male genitalia. Surg Gynecol Obstet. 1990 Jan;170(1):49–55. [PubMed] [Google Scholar]
- Darke S. G., King A. M., Slack W. K. Gas gangrene and related infection: classification, clinical features and aetiology, management and mortality. A report of 88 cases. Br J Surg. 1977 Feb;64(2):104–112. doi: 10.1002/bjs.1800640207. [DOI] [PubMed] [Google Scholar]
- Dellinger E. P. Severe necrotizing soft-tissue infections. Multiple disease entities requiring a common approach. JAMA. 1981 Oct 9;246(15):1717–1721. [PubMed] [Google Scholar]
- Eltorai I. M., Hart G. B., Strauss M. B., Montroy R., Juler G. L. The role of hyperbaric oxygen in the management of Fournier's gangrene. Int Surg. 1986 Jan-Mar;71(1):53–58. [PubMed] [Google Scholar]
- Enriquez J. M., Moreno S., Devesa M., Morales V., Platas A., Vicente E. Fournier's syndrome of urogenital and anorectal origin. A retrospective, comparative study. Dis Colon Rectum. 1987 Jan;30(1):33–37. doi: 10.1007/BF02556919. [DOI] [PubMed] [Google Scholar]
- Freischlag J. A., Ajalat G., Busuttil R. W. Treatment of necrotizing soft tissue infections. The need for a new approach. Am J Surg. 1985 Jun;149(6):751–755. doi: 10.1016/s0002-9610(85)80180-x. [DOI] [PubMed] [Google Scholar]
- Giuliano A., Lewis F., Jr, Hadley K., Blaisdell F. W. Bacteriology of necrotizing fasciitis. Am J Surg. 1977 Jul;134(1):52–57. doi: 10.1016/0002-9610(77)90283-5. [DOI] [PubMed] [Google Scholar]
- Hirn M., Niinikoski J. Management of perineal necrotizing fasciitis (Fournier's gangrene). Ann Chir Gynaecol. 1989;78(4):277–281. [PubMed] [Google Scholar]
- Jackson R. W., Waddell J. P. Hyperbaric oxygen in the management of clostridial myonecrosis (gas gangrene). Clin Orthop Relat Res. 1973 Oct;(96):271–276. [PubMed] [Google Scholar]
- Janevicius R. V., Hann S. E., Batt M. D. Necrotizing fasciitis. Surg Gynecol Obstet. 1982 Jan;154(1):97–102. [PubMed] [Google Scholar]
- Kaiser R. E., Cerra F. B. Progressive necrotizing surgical infections--a unified approach. J Trauma. 1981 May;21(5):349–355. doi: 10.1097/00005373-198105000-00003. [DOI] [PubMed] [Google Scholar]
- Kawakami M., Cerami A. Studies of endotoxin-induced decrease in lipoprotein lipase activity. J Exp Med. 1981 Sep 1;154(3):631–639. doi: 10.1084/jem.154.3.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maderazo E. G., Woronick C. L., Hickingbotham N., Mercier E., Jacobs L., Bhagavan H. Additional evidence of autoxidation as a possible mechanism of neutrophil locomotory dysfunction in blunt trauma. Crit Care Med. 1990 Feb;18(2):141–147. doi: 10.1097/00003246-199002000-00003. [DOI] [PubMed] [Google Scholar]
- Majeski J. A., Alexander J. W. Early diagnosis, nutritional support, and immediate extensive debridement improve survival in necrotizing fasciitis. Am J Surg. 1983 Jun;145(6):784–787. doi: 10.1016/0002-9610(83)90140-x. [DOI] [PubMed] [Google Scholar]
- Patiño J. F., Castro D. Necrotizing lesions of soft tissues: a review. World J Surg. 1991 Mar-Apr;15(2):235–239. doi: 10.1007/BF01659058. [DOI] [PubMed] [Google Scholar]
- Paty R., Smith A. D. Gangrene and Fournier's gangrene. Urol Clin North Am. 1992 Feb;19(1):149–162. [PubMed] [Google Scholar]
- Pessa M. E., Howard R. J. Necrotizing fasciitis. Surg Gynecol Obstet. 1985 Oct;161(4):357–361. [PubMed] [Google Scholar]
- Riseman J. A., Zamboni W. A., Curtis A., Graham D. R., Konrad H. R., Ross D. S. Hyperbaric oxygen therapy for necrotizing fasciitis reduces mortality and the need for debridements. Surgery. 1990 Nov;108(5):847–850. [PubMed] [Google Scholar]
- Stamenkovic I., Lew P. D. Early recognition of potentially fatal necrotizing fasciitis. The use of frozen-section biopsy. N Engl J Med. 1984 Jun 28;310(26):1689–1693. doi: 10.1056/NEJM198406283102601. [DOI] [PubMed] [Google Scholar]
- Umbert I. J., Winkelmann R. K., Oliver G. F., Peters M. S. Necrotizing fasciitis: a clinical, microbiologic, and histopathologic study of 14 patients. J Am Acad Dermatol. 1989 May;20(5 Pt 1):774–781. doi: 10.1016/s0190-9622(89)70089-x. [DOI] [PubMed] [Google Scholar]
- WILSON B. Necrotizing fasciitis. Am Surg. 1952 Apr;18(4):416–431. [PubMed] [Google Scholar]
- Ward R. G., Walsh M. S. Necrotizing fasciitis: 10 years' experience in a district general hospital. Br J Surg. 1991 Apr;78(4):488–489. doi: 10.1002/bjs.1800780431. [DOI] [PubMed] [Google Scholar]


