Abstract
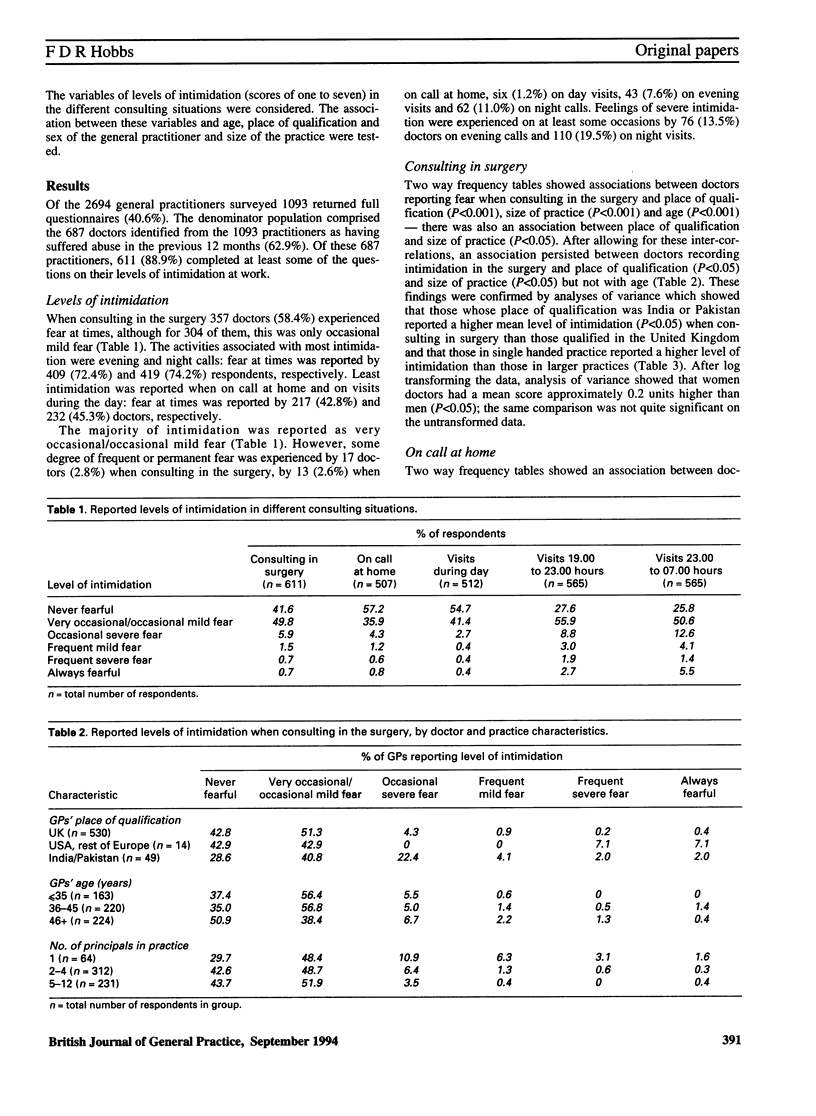
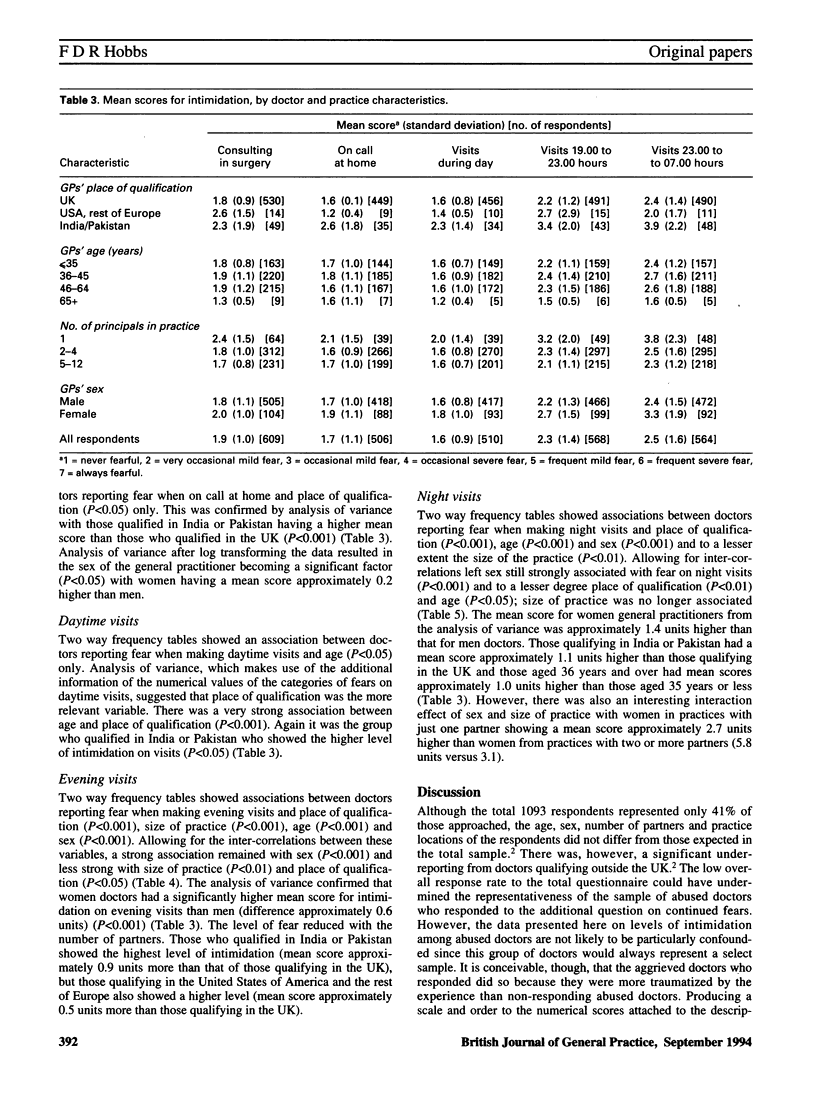
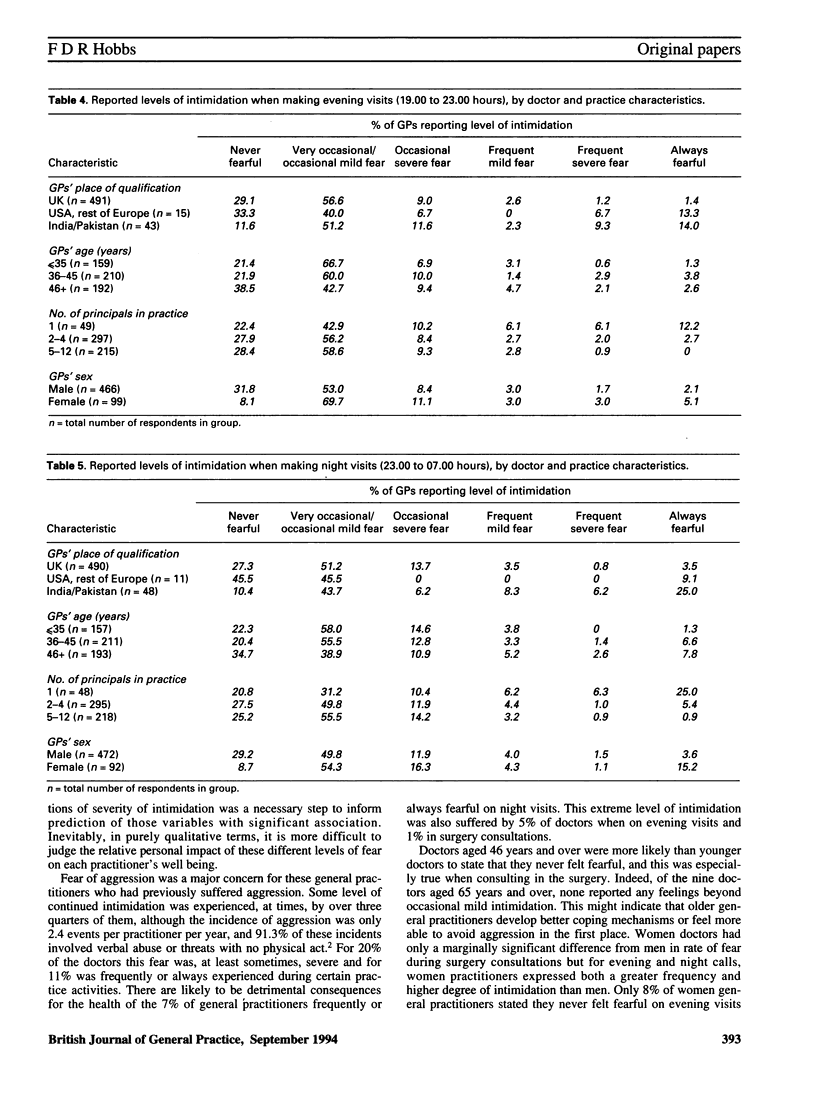
BACKGROUND: Relatively few data exist on the scale of aggression from patients or patients' relatives suffered by doctors at work. Such aggression might be expected to pose considerable risks of continued morbidity among abused practitioners. AIM: This study set out to survey the continued levels of intimidation experienced by general practitioners who had suffered a previous episode of aggression. METHODS: A retrospective survey was carried out of all general practitioners in the West Midlands Health Authority region, using a piloted postal questionnaire. Of the 2694 surveyed 1093 (41%) responded. Among responding doctors, 687 (63%) had suffered some degree of aggression in the previous 12 months, and these respondents reported on the degree of intimidation experienced during specified clinical duties. RESULTS: Nearly three quarters of previously abused doctors did, at times, express ongoing fears for their safety at work. Indeed, 71% of doctors who qualified in India and Pakistan and 57% of doctors who qualified in the United Kingdom experienced some degree of intimidation within their surgery (90% and 73%, respectively, on night visits). Fear was most commonly reported during visits made out of hours with mild fear being occasionally experienced between 19.00 and 23.00 hours by 316 (56%) of the responding abused doctors and after 23.00 hours by 286 (51%). Eleven respondents (2%) were frequently severely fearful on evening visits and 15 (3%) were always fearful. On night visits frequent severe fear was reported by eight respondents (1%), while 31 were always fearful (6%). The differences between men and women doctors were relatively small within the surgery, but during out-of-hours calls women were significantly more likely to report intimidation than men practitioners and to report significantly higher levels of severity of fear. CONCLUSION: These findings support further consideration of the contractual commitment for general practitioners to provide out-of-hours visiting, of investment in safer surgeries and of greater provision of in-service training in handling aggression and its attendant stress.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bollam M. J., McCarthy M., Modell M. Patient's assessment of out of hours care in general practice. Br Med J (Clin Res Ed) 1988 Mar 19;296(6625):829–832. doi: 10.1136/bmj.296.6625.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Urso P., Hobbs R. Aggression and the general practitioner. BMJ. 1989 Jan 14;298(6666):97–98. doi: 10.1136/bmj.298.6666.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris A. Violence in general practice. BMJ. 1989 Jan 14;298(6666):63–64. doi: 10.1136/bmj.298.6666.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs F. D. Violence in general practice: a survey of general practitioners' views. BMJ. 1991 Feb 9;302(6772):329–332. doi: 10.1136/bmj.302.6772.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliffe S., Haug U. Out of hours work in general practice. BMJ. 1991 Jun 29;302(6792):1584–1586. doi: 10.1136/bmj.302.6792.1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myerson S. Investigating stresses in general practice using an open-ended approach in interviews. Fam Pract. 1990 Jun;7(2):91–95. doi: 10.1093/fampra/7.2.91. [DOI] [PubMed] [Google Scholar]
- Myerson S. Violence to general practitioners and fear of violence. Fam Pract. 1991 Jun;8(2):145–147. doi: 10.1093/fampra/8.2.145. [DOI] [PubMed] [Google Scholar]
- Sutherland V. J., Cooper C. L. Job stress, satisfaction, and mental health among general practitioners before and after introduction of new contract. BMJ. 1992 Jun 13;304(6841):1545–1548. doi: 10.1136/bmj.304.6841.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]


