Abstract
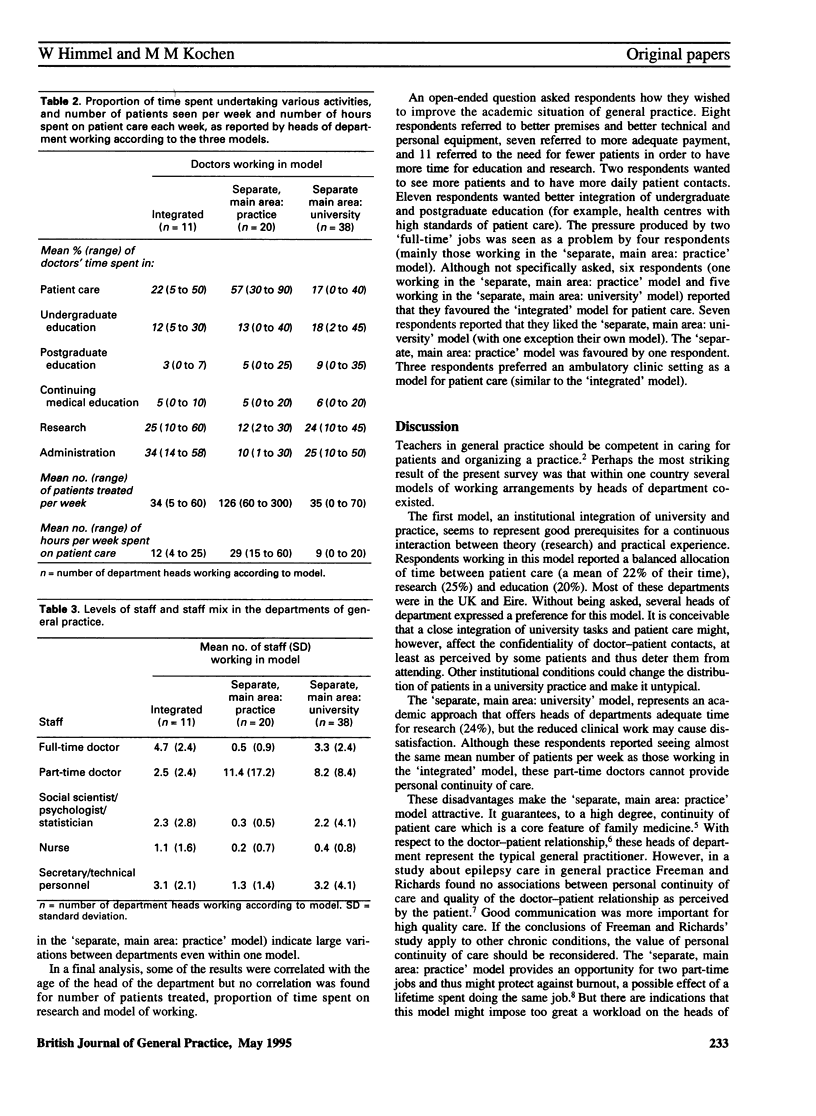
BACKGROUND. Compared with other clinical disciplines, academic general practice is in a difficult situation with respect to patient care. There are at least three different possible models of working arrangements for heads of departments of general practice: to work in a surgery in a medical school; to work in a surgery in the community, separate from a part-time university post; or to work part-time in a surgery in the community, separate from a university post. AIM. A study was undertaken to explore these models and to gain an understanding of academic teachers' organization of patient care in Europe. METHOD. A total of 77 heads of departments in universities in 12 European countries were sent a questionnaire enquiring about important characteristics of their department, the number of patients they treated per week and how they allocated their time. RESULTS. Sixty nine heads of department (90%) responded. Of respondents, 55% worked part-time in a surgery, separate from a university post, nearly one third worked mainly in a surgery, separate from a part-time university post, and 16% worked in a surgery in a medical school. Those working in a surgery with only a part-time university post spent most time in patient care compared with those working in other models (mean of 57%). Respondents working in a surgery in a medical school spent most time on administration (34%); they spent 22% of their time on patient care and 20% on education. Respondents working in a surgery in a medical school spent 25% of their time on research, those working in a surgery separate from a part-time university post spent 12% of their time on research, and those working mainly in a university with a part-time practice post spent 24% of their time on research. Those working mainly in a university post spent only 17% of their time in patient care. CONCLUSION. Working in a surgery in a medical school represented a well-balanced model of time allocation between patient care, research and education and seemed to be a good approach for the integration of general practice into medical schools. Working part-time in a surgery with a university post is an appropriate model for academic integration, but patient care seemed to be neglected. Those doctors working mainly in the community with a part-time university post were able to provide continuity of care and to come into close contact with the everyday problems of general practitioners. However, they might have to struggle for academic recognition.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allen J., Wilson A., Fraser R., Gray D. P. The academic base for general practice: the case for change. BMJ. 1993 Sep 18;307(6906):719–722. doi: 10.1136/bmj.307.6906.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis P. Academic base for general practice. BMJ. 1994 Jan 1;308(6920):64–64. doi: 10.1136/bmj.308.6920.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans P. R. The changing scene in general practice in Europe. BMJ. 1994 Mar 5;308(6929):645–648. doi: 10.1136/bmj.308.6929.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman G. K., Richards S. C. Personal continuity and the care of patients with epilepsy in general practice. Br J Gen Pract. 1994 Sep;44(386):395–399. [PMC free article] [PubMed] [Google Scholar]
- Geyman J. P. Family medicine as an academic discipline: progress, challenges, and opportunities. J Fam Pract. 1990 Sep;31(3):297–303. [PubMed] [Google Scholar]
- Handysides S. Building morale through personal development. BMJ. 1994 Jan 8;308(6921):114–116. doi: 10.1136/bmj.308.6921.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murata P. J., Lynch W. D., Puffer J. C., Green L. A. Attitudes toward and experience in research among family medicine chairs. J Fam Pract. 1992 Oct;35(4):417–421. [PubMed] [Google Scholar]
- Taylor R. B., Colwill J. M., Puffer J. C., Heffron W. A., Marsland D. W., Rakel R. E., Geyman J. P. Success strategies for departments of family medicine. J Am Board Fam Pract. 1991 Nov-Dec;4(6):427–436. [PubMed] [Google Scholar]


