Abstract
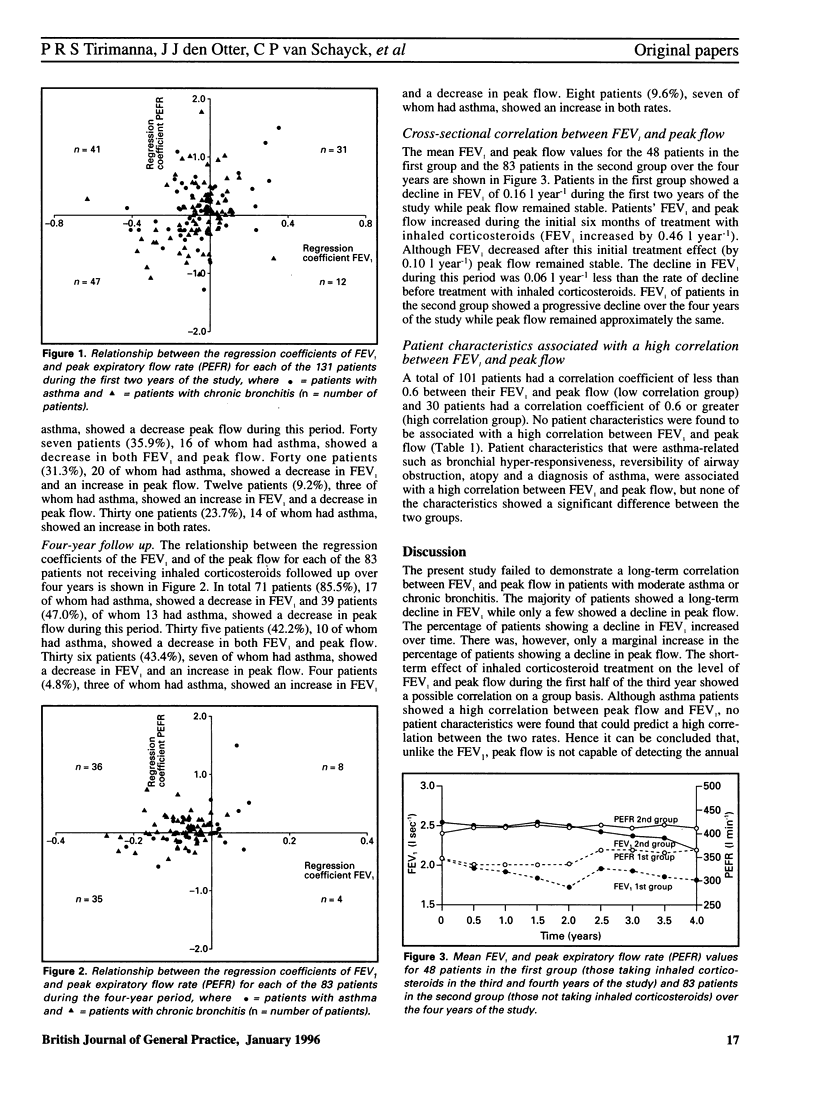
BACKGROUND: Early detection and treatment of patients with asthma or chronic bronchitis who have a rapid annual decline in lung function is essential in order to improve their long-term prognosis. This annual rate of decline can be assessed accurately by monitoring the forced expiratory volume in one second (FEV1) which is a routine procedure in hospital respiratory laboratories but not in general practice. General practitioners usually measure patients' peak expiratory flow rate (peak flow) to evaluate lung function. If annual decline in lung function can be assessed by monitoring peak flow, this method could be used in general practice for detecting patients at an early stage who have a rapid decline. AIM: A study aimed to investigate the long-term correlation between FEV1 and peak flow among a group of patients in Nijmegen, the Netherlands. METHOD: FEV1 and peak flow were monitored in 53 patients with moderate asthma and 78 patients with moderate chronic bronchitis over four years. FEV1 was measured in a laboratory once every six months and peak flow was measured by patients once a week. The correlation between the two sets of measurements was studied for each patient. RESULTS: Four-year data for 83 of the 131 patients were analysed; the other 48 patients received inhaled steroids during the second half of the study period so their data were not considered for all the analyses. Of the 83 patients, 35 (42%) showed a decrease in both FEV1 and peak flow. Thirty six patients (43%) showed a decrease in FEV1 and an increase in peak flow. Four patients (5%) showed an increase in FEV1 and a decrease in peak flow and eight patients (10%) showed an increase in both rates. Approximately similar results were seen in a separate analysis of all 131 patients during the first two years of the study. CONCLUSION: No long-term correlation was found between FEV1 and peak flow. Peak flow is not capable of detecting annual decline in lung function. Therefore it cannot be used to detect patients with asthma or chronic bronchitis who have a rapid annual decline in lung function. Spirometers, which measure peak flow and FEV1, could be used in general practice. These would allow general practitioners to continue measuring peak flow in order to assess short-term changes in lung function while providing an important means for monitoring FEV1 to assess long-term changes in lung function.
Full text
PDF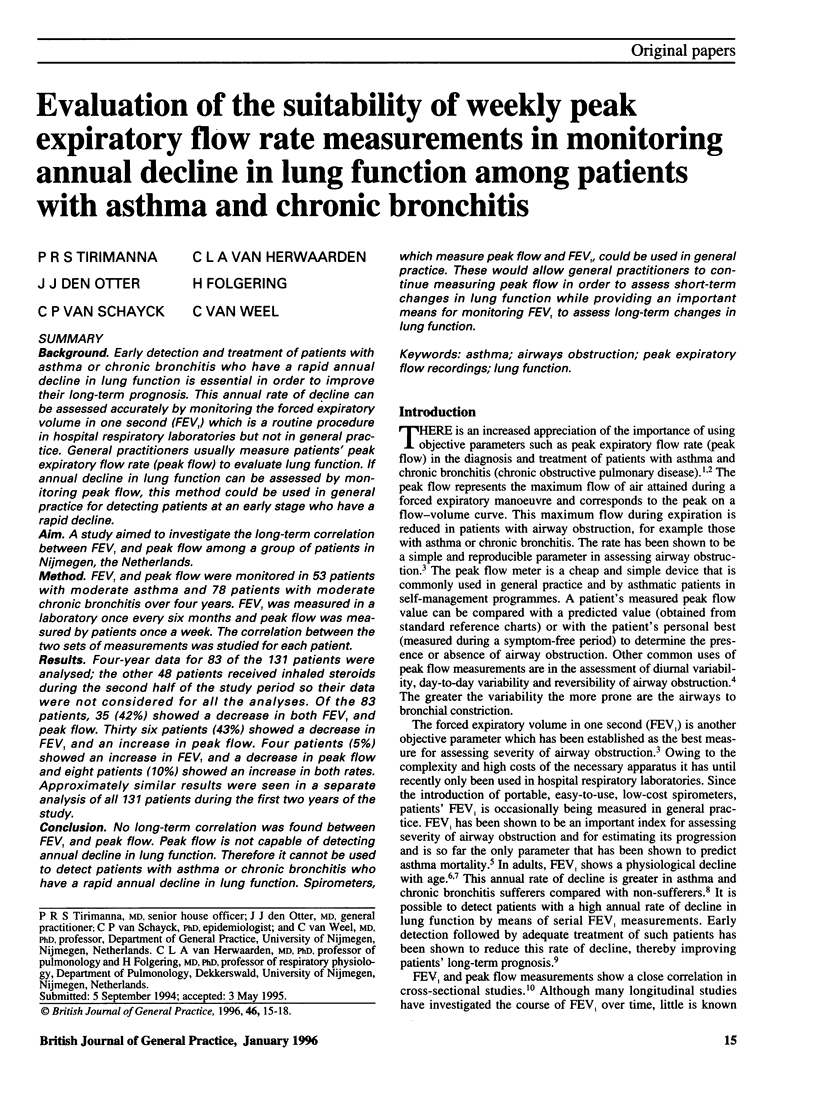


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boman G., Bäcker U., Larsson S., Melander B., Wåhlander L. Oral acetylcysteine reduces exacerbation rate in chronic bronchitis: report of a trial organized by the Swedish Society for Pulmonary Diseases. Eur J Respir Dis. 1983 Aug;64(6):405–415. [PubMed] [Google Scholar]
- Burrows B., Bloom J. W., Traver G. A., Cline M. G. The course and prognosis of different forms of chronic airways obstruction in a sample from the general population. N Engl J Med. 1987 Nov 19;317(21):1309–1314. doi: 10.1056/NEJM198711193172103. [DOI] [PubMed] [Google Scholar]
- Burrows B., Cline M. G., Knudson R. J., Taussig L. M., Lebowitz M. D. A descriptive analysis of the growth and decline of the FVC and FEV1. Chest. 1983 May;83(5):717–724. doi: 10.1378/chest.83.5.717. [DOI] [PubMed] [Google Scholar]
- Dekker F. W., Schrier A. C., Sterk P. J., Dijkman J. H. Validity of peak expiratory flow measurement in assessing reversibility of airflow obstruction. Thorax. 1992 Mar;47(3):162–166. doi: 10.1136/thx.47.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dompeling E., van Schayck C. P., Folgering H., van den Hoogen H. J., van Weel C. Accuracy, precision and linearity of the portable flow-volume meter Microspiro HI-298. Eur Respir J. 1991 May;4(5):612–615. [PubMed] [Google Scholar]
- Dompeling E., van Schayck C. P., van Grunsven P. M., van Herwaarden C. L., Akkermans R., Molema J., Folgering H., van Weel C. Slowing the deterioration of asthma and chronic obstructive pulmonary disease observed during bronchodilator therapy by adding inhaled corticosteroids. A 4-year prospective study. Ann Intern Med. 1993 May 15;118(10):770–778. doi: 10.7326/0003-4819-118-10-199305150-00003. [DOI] [PubMed] [Google Scholar]
- Fletcher C., Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977 Jun 25;1(6077):1645–1648. doi: 10.1136/bmj.1.6077.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly C. A., Gibson G. J. Relation between FEV1 and peak expiratory flow in patients with chronic airflow obstruction. Thorax. 1988 Apr;43(4):335–336. doi: 10.1136/thx.43.4.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz M. D. The use of peak expiratory flow rate measurements in respiratory disease. Pediatr Pulmonol. 1991;11(2):166–174. doi: 10.1002/ppul.1950110215. [DOI] [PubMed] [Google Scholar]
- Peat J. K., Woolcock A. J., Cullen K. Rate of decline of lung function in subjects with asthma. Eur J Respir Dis. 1987 Mar;70(3):171–179. [PubMed] [Google Scholar]
- van Schayck C. P., Dompeling E., van Herwaarden C. L., Folgering H., Verbeek A. L., van der Hoogen H. J., van Weel C. Bronchodilator treatment in moderate asthma or chronic bronchitis: continuous or on demand? A randomised controlled study. BMJ. 1991 Dec 7;303(6815):1426–1431. doi: 10.1136/bmj.303.6815.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Schayck C. P., Dompeling E., van Weel C., Folgering H., van den Hoogen H. J. Accuracy and reproducibility of the Assess peak flow meter. Eur Respir J. 1990 Mar;3(3):338–341. [PubMed] [Google Scholar]


