Abstract
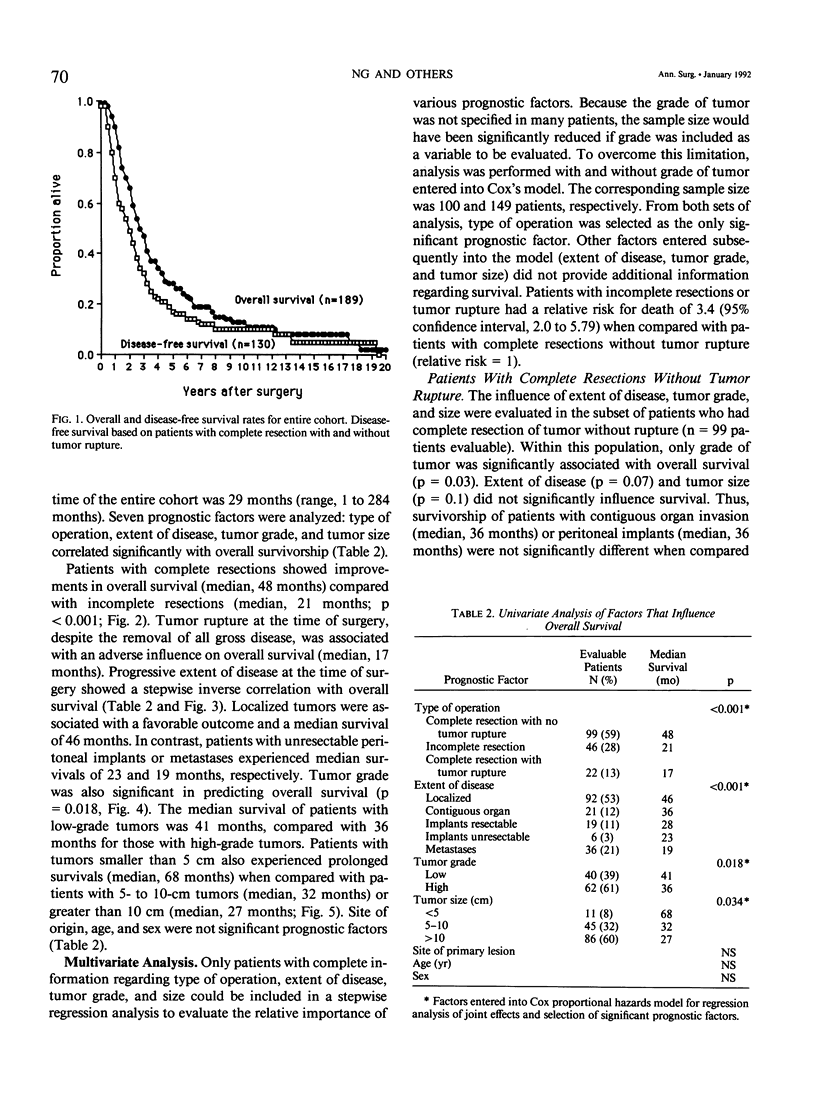
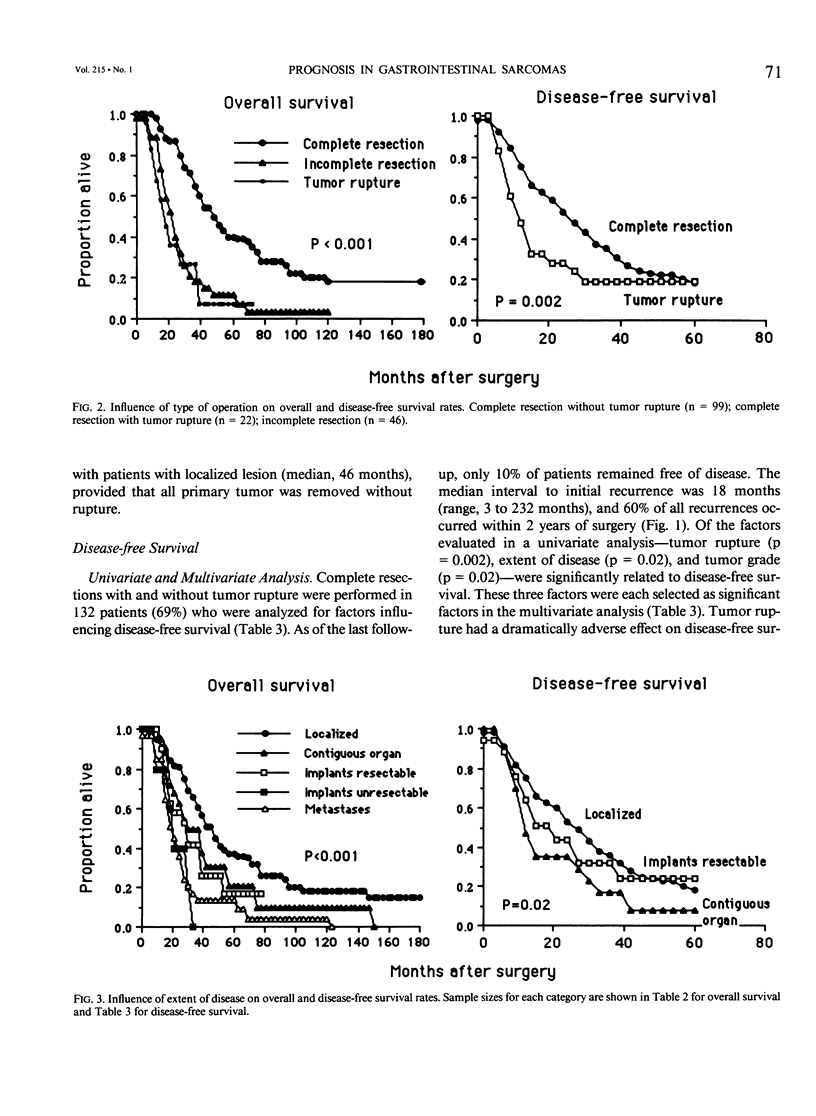
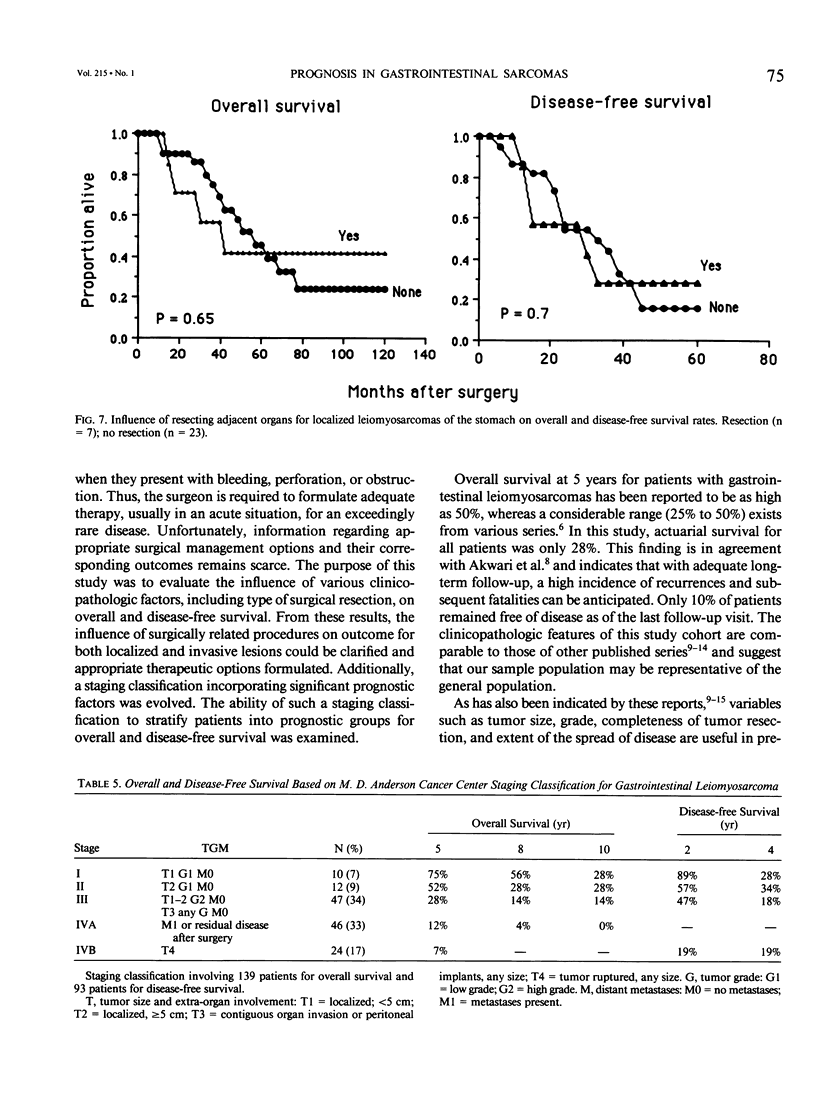
The appropriate surgical therapeutic options for either localized or more advanced disease in patients with gastrointestinal leiomyosarcomas remain unclear. A staging classification for this disease has not been adopted nor risk factors identifying patients at risk for recurrence defined. To address these issues, this study evaluated the influence of various clinicopathologic variables on overall and disease-free survival. In an univariate analysis of overall survival involving 191 patients, the Cox proportional hazards model identified four factors that were associated with a significantly better outcome: complete resection without tumor rupture (p less than 0.001), localized lesions (p less than 0.001), low grade of tumor (p = 0.02), and tumors smaller than 5 cm (p = 0.03). When interactive effects of these factors were taken into account, however, type of resection of the tumor was selected as the only significant prognostic factor in a multivariate analysis. Complete resection without tumor rupture improved overall survival of patients with localized disease (median, 46 months) as well as those with contiguous organ invasion (median, 36 months) or peritoneal implants (median, 36 months). In contrast, patients with incomplete resections survived for a median of 21 months. Patients with tumor rupture, despite removal of all gross disease, behaved similarly to those with incomplete resections; median survival was only 17 months. For disease-free survival, important determinants selected from a multivariate analysis were tumor rupture (p = 0.002), contiguous organ invasion (p = 0.02) and high tumor grade (p = 0.02). A staging classification incorporating these prognostic factors of significance was evaluated using a TGM system: T1 (less than 5 cm), T2 (greater than or equal to 5 cm), T3 (contiguous organ invasion or peritoneal implants), T4 (tumor rupture); G: G1 (low grade), G2 (high grade); M: M0 (no metastases), M1 (metastases present). The corresponding 5-year overall survivals for stages I, II, III, IVA, and IVB were 75%, 52%, 28%, 12%, and 7%. Disease-free survival at 2 years after surgery was 89%, 57%, and 47% for stages I, II, and III, respectively. In conclusion, surgery remains the primary modality of treatment for patients with gastrointestinal leiomyosarcomas, and complete resection of all disease without tumor rupture, even of locally advanced disease, improves overall and disease-free survival. A staging classification appears feasible and is recommended to determine outcome in patients with leiomyosarcomas arising from the gastrointestinal tract.
Full text
PDF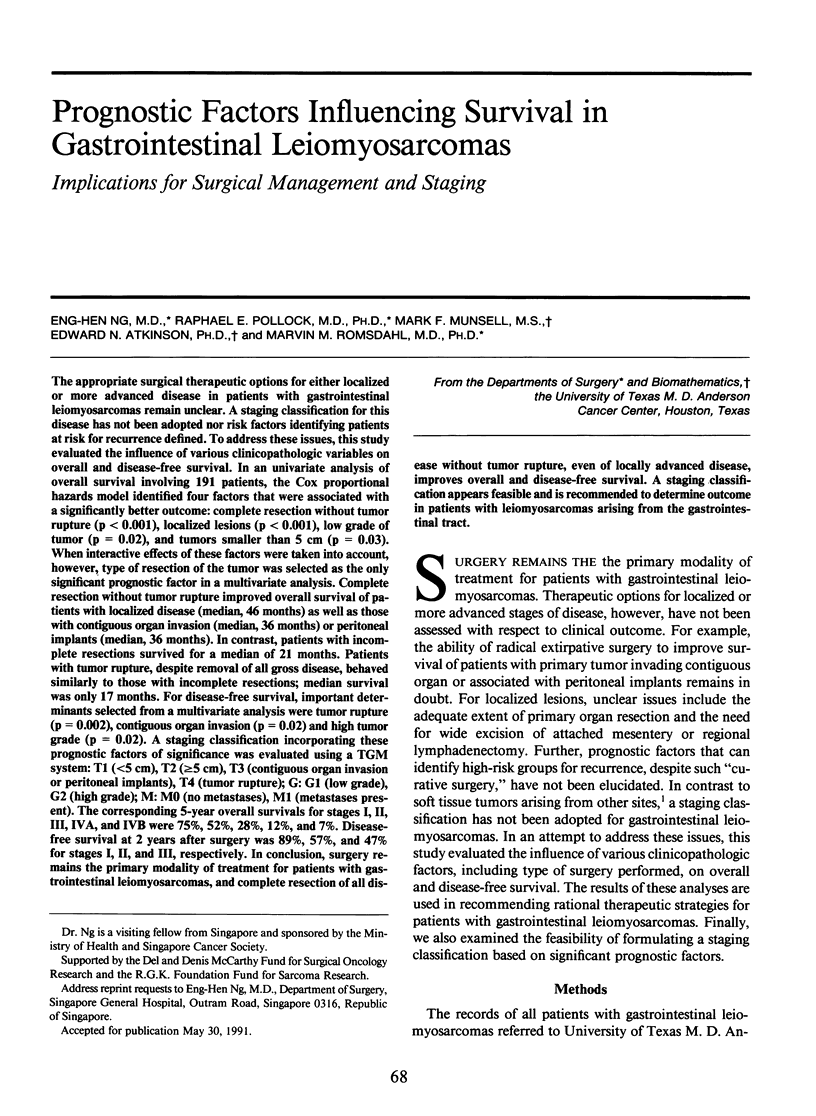






Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akwari O. E., Dozois R. R., Weiland L. H., Beahrs O. H. Leiomyosarcoma of the small and large bowel. Cancer. 1978 Sep;42(3):1375–1384. doi: 10.1002/1097-0142(197809)42:3<1375::aid-cncr2820420348>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Appelman H. D., Helwig E. B. Sarcomas of the stomach. Am J Clin Pathol. 1977 Jan;67(1):2–10. [PubMed] [Google Scholar]
- Appelman H. D. Smooth muscle tumors of the gastrointestinal tract. What we know now that Stout didn't know. Am J Surg Pathol. 1986;10 (Suppl 1):83–99. [PubMed] [Google Scholar]
- BERKSON J., GAGE R. P. Calculation of survival rates for cancer. Proc Staff Meet Mayo Clin. 1950 May 24;25(11):270–286. [PubMed] [Google Scholar]
- Chiotasso P. J., Fazio V. W. Prognostic factors of 28 leiomyosarcomas of the small intestine. Surg Gynecol Obstet. 1982 Aug;155(2):197–202. [PubMed] [Google Scholar]
- Evans H. L. Smooth muscle tumors of the gastrointestinal tract. A study of 56 cases followed for a minimum of 10 years. Cancer. 1985 Nov 1;56(9):2242–2250. doi: 10.1002/1097-0142(19851101)56:9<2242::aid-cncr2820560918>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Lee E. T., Desu M. M. A computer program for comparing K samples with right-censored data. Comput Programs Biomed. 1972 Nov;2(4):315–321. doi: 10.1016/0010-468x(72)90019-0. [DOI] [PubMed] [Google Scholar]
- Lee Y. T. Leiomyosarcoma of the gastro-intestinal tract: general pattern of metastasis and recurrence. Cancer Treat Rev. 1983 Jun;10(2):91–101. doi: 10.1016/0305-7372(83)90007-5. [DOI] [PubMed] [Google Scholar]
- Licht J. D., Weissmann L. B., Antman K. Gastrointestinal sarcomas. Semin Oncol. 1988 Apr;15(2):181–188. [PubMed] [Google Scholar]
- Lindsay P. C., Ordonez N., Raaf J. H. Gastric leiomyosarcoma: clinical and pathological review of fifty patients. J Surg Oncol. 1981;18(4):399–421. doi: 10.1002/jso.2930180409. [DOI] [PubMed] [Google Scholar]
- McGrath P. C., Neifeld J. P., Lawrence W., Jr, Kay S., Horsley J. S., 3rd, Parker G. A. Gastrointestinal sarcomas. Analysis of prognostic factors. Ann Surg. 1987 Dec;206(6):706–710. doi: 10.1097/00000658-198712000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer S., Peretz T., Gaynor J. J., Tan C., Hajdu S. I., Brennan M. F. Primary colorectal sarcoma. A retrospective review and prognostic factor study of 50 consecutive patients. Arch Surg. 1990 Sep;125(9):1163–1168. doi: 10.1001/archsurg.1990.01410210089014. [DOI] [PubMed] [Google Scholar]
- SKANDALAKIS J. E., GRAY S. W. SMOOTH MUSCLE TUMORS OF THE ALIMENTARY TRACT. Prog Clin Cancer. 1965;10:692–708. [PubMed] [Google Scholar]
- Shiu M. H., Farr G. H., Egeli R. A., Quan S. H., Hajdu S. I. Myosarcomas of the small and large intestine: a clinicopathologic study. J Surg Oncol. 1983 Sep;24(1):67–72. doi: 10.1002/jso.2930240116. [DOI] [PubMed] [Google Scholar]
- Shiu M. H., Farr G. H., Papachristou D. N., Hajdu S. I. Myosarcomas of the stomach: natural history, prognostic factors and management. Cancer. 1982 Jan 1;49(1):177–187. doi: 10.1002/1097-0142(19820101)49:1<177::aid-cncr2820490136>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]


