Abstract
OBJECTIVE AND SUMMARY BACKGROUND: Symptomatic, medically resistant postgastrectomy patients with alkaline reflux gastritis (ARG) have increased enterogastric reflux (EGR) documented by quantitative radionuclide biliary scanning. Even asymptomatic patients after gastrectomy have increased EGR compared with nonoperated control patients. Roux-en-Y biliary diversion, although successfully treats the clinical syndrome of ARG, has a high incidence of early and late postoperative severe gastroparesis, Roux limb retention (the Roux syndrome), or both, which often requires further remedial surgery. As an alternative to Roux-en-Y diversion, this review evaluates the efficacy of the Braun enteroenterostomy (BEE) in diverting bile away from the stomach in patients having gastric operations. Based on previous pilot studies, the BEE is positioned 30 cm from the gastroenterostomy. METHODS: Thirty patients had the following operations and were evaluated: standard pancreatoduodenectomy (8), vagotomy and Billroth II (BII) gastrectomy (6), BII gastrectomy only (10), and palliative gastroenterostomy to an intact stomach (6). All anastomoses were antecolic BII with a long afferent limb and a 30-cm BEE. Four symptomatic patients with medically intractable ARG and chronic gastroparesis had subtotal BII gastric resection with BEE rather than Roux-en-Y diversion. Eight control symptomatic patients and six asymptomatic patients with previous BII gastrectomy and no BEE were evaluated. Radionuclide biliary scanning was performed within 30 days in all patients and at 4 to 6 months in 14 patients. Bile reflux was expressed as an EGR index (%). RESULTS: After operation, 18 of 34 patients (53%) had no demonstrable EGR while in the fasting state for as long as 90 minutes. The range of demonstrable bile reflux (EGR) in the remaining 16 patients was from 2% to 17% (mean, 4.5%). Enterogastric reflux in the 14 control patients (with no BEE) ranged from 5% to 82% (mean, 42%). The four patients with ARG and chronic gastroparesis treated by subtotal gastrectomy and BEE had postoperative EGR of 0%, 2%, 2%, and 4%, respectively. They are asymptomatic with no evidence of bile reflux gastritis. In the 14 patients who had late evaluation, EGR ranged from 0% to 16% (mean, 5.5%). No patient had signs or symptoms of ARG after operation. CONCLUSIONS: Braun enteroenterostomy successfully diverts a substantial amount of bile from the stomach. The ARG syndrome might be prevented by performing BEE during gastric resection or bypass in a variety of operations. Conversion to a BII with BEE may be an alternative to Roux-en-Y diversion in treating medically resistant ARG and subsequent may avoid the Roux syndrome.
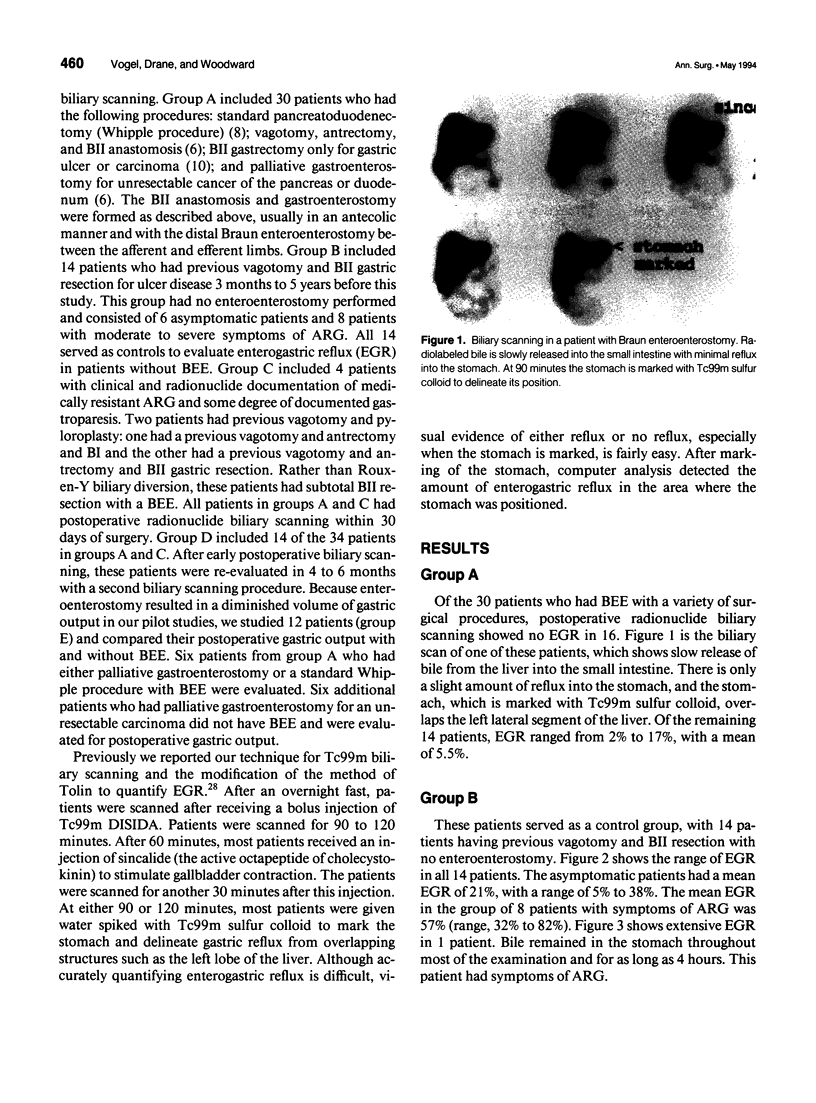
Full text
PDF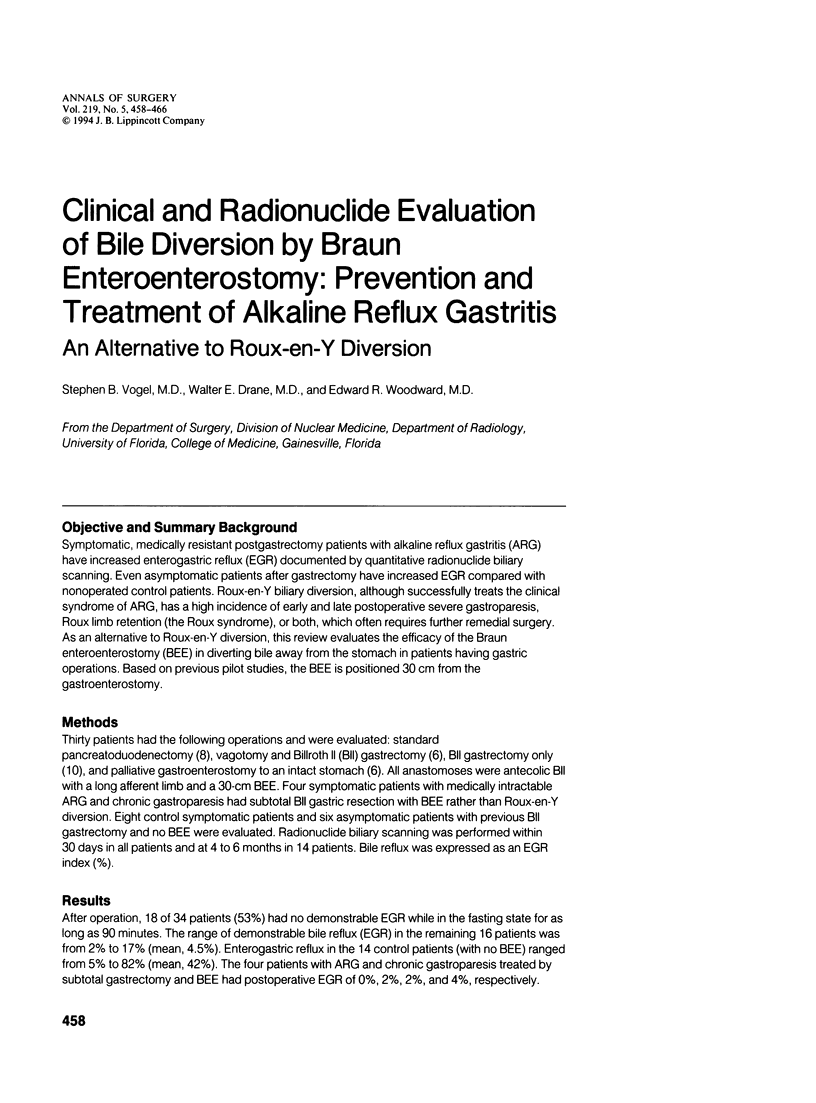



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bartlett M. K., Burrington J. D. Bilious vomiting after gastric surgery. Experience with a modified Roux-Y loop for relief. Arch Surg. 1968 Jul;97(1):34–39. doi: 10.1001/archsurg.1968.01340010064004. [DOI] [PubMed] [Google Scholar]
- Boren C. H., Way L. W. Alkaline reflux gastritis: a reevaluation. Am J Surg. 1980 Jul;140(1):40–46. doi: 10.1016/0002-9610(80)90415-8. [DOI] [PubMed] [Google Scholar]
- Davidson E. D., Hersh T. Bile reflux gastritis. Contribution of inadequate gastric emptying. Am J Surg. 1975 Nov;130(5):514–518. doi: 10.1016/0002-9610(75)90502-4. [DOI] [PubMed] [Google Scholar]
- Davidson E. D., Hersh T. The surgical treatment of bile reflux gastritis: a study of 59 patients. Ann Surg. 1980 Aug;192(2):175–178. doi: 10.1097/00000658-198008000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester T. R., Fuchs K. H., Ball C. S., Albertucci M., Smyrk T. C., Marcus J. N. Experimental and clinical results with proximal end-to-end duodenojejunostomy for pathologic duodenogastric reflux. Ann Surg. 1987 Oct;206(4):414–426. doi: 10.1097/00000658-198710000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckhauser F. E., Knol J. A., Raper S. A., Guice K. S. Completion gastrectomy for postsurgical gastroparesis syndrome. Preliminary results with 15 patients. Ann Surg. 1988 Sep;208(3):345–353. doi: 10.1097/00000658-198809000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths J. M., Smith A. N., Small W. P., Falconer C. W. The results of reoperation for bile vomiting following surgery for peptic ulcer. Br J Surg. 1974 Oct;61(10):838–843. doi: 10.1002/bjs.1800611021. [DOI] [PubMed] [Google Scholar]
- Gustavsson S., Ilstrup D. M., Morrison P., Kelly K. A. Roux-Y stasis syndrome after gastrectomy. Am J Surg. 1988 Mar;155(3):490–494. doi: 10.1016/s0002-9610(88)80120-x. [DOI] [PubMed] [Google Scholar]
- Harrison W. D., Hocking M. P., Vogel S. B. Gastric emptying and myoelectric activity following Roux-en-Y gastrojejunostomy. J Surg Res. 1990 Nov;49(5):385–389. doi: 10.1016/0022-4804(90)90184-4. [DOI] [PubMed] [Google Scholar]
- Herrington J. L., Jr Editorial: Roux-en-Y diversion as an alternate method of reconstruction of the alimentary tract after primary resection of the stomach. Surg Gynecol Obstet. 1976 Jul;143(1):92–93. [PubMed] [Google Scholar]
- Hinder R. A., Esser J., DeMeester T. R. Management of gastric emptying disorders following the Roux-en-Y procedure. Surgery. 1988 Oct;104(4):765–772. [PubMed] [Google Scholar]
- Karlstrom L. H., Soper N. J., Kelly K. A., Phillips S. F. Ectopic jejunal pacemakers and enterogastric reflux after Roux gastrectomy: effect of intestinal pacing. Surgery. 1989 Sep;106(3):486–495. [PubMed] [Google Scholar]
- Karlstrom L., Kelly K. A. Roux-Y gastrectomy for chronic gastric atony. Am J Surg. 1989 Jan;157(1):44–49. doi: 10.1016/0002-9610(89)90418-2. [DOI] [PubMed] [Google Scholar]
- Kennedy T., Green R. Roux diversion for bile reflux following gastric surgery. Br J Surg. 1978 May;65(5):323–325. doi: 10.1002/bjs.1800650510. [DOI] [PubMed] [Google Scholar]
- Mackie C., Hulks G., Cuschieri A. Enterogastric reflux and gastric clearance of refluxate in normal subjects and in patients with and without bile vomiting following peptic ulcer surgery. Ann Surg. 1986 Nov;204(5):537–542. doi: 10.1097/00000658-198611000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malagelada J. R., Phillips S. F., Shorter R. G., Higgins J. A., Magrina C., van Heerden J. A., Adson M. A. Postoperative reflux gastritis: pathophysiology and long-term outcome after Roux-en-Y diversion. Ann Intern Med. 1985 Aug;103(2):178–183. doi: 10.7326/0003-4819-103-2-178. [DOI] [PubMed] [Google Scholar]
- Mathias J. R., Fernandez A., Sninsky C. A., Clench M. H., Davis R. H. Nausea, vomiting, and abdominal pain after Roux-en-Y anastomosis: motility of the jejunal limb. Gastroenterology. 1985 Jan;88(1 Pt 1):101–107. doi: 10.1016/s0016-5085(85)80140-2. [DOI] [PubMed] [Google Scholar]
- Mayo W. J. X. Duodenal Ulcer: A Clinical Review of Fifty-Eight Operated Cases, with Some Remarks on Gastrojejunostomy. Ann Surg. 1904 Dec;40(6):900–908. doi: 10.1097/00000658-190412000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J. H. Reflections on reflux gastritis. Gastroenterology. 1979 Nov;77(5):1143–1145. [PubMed] [Google Scholar]
- Perino L. E., Adcock K. A., Goff J. S. Gastrointestinal symptoms, motility, and transit after the Roux-en-Y operation. Am J Gastroenterol. 1988 Apr;83(4):380–385. [PubMed] [Google Scholar]
- Ritchie W. P. Alkaline reflux gastritis: a critical reappraisal. Gut. 1984 Sep;25(9):975–987. doi: 10.1136/gut.25.9.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Stiegmann G., Goff J. S. An alternative to Roux-en-Y for treatment of bile reflux gastritis. Surg Gynecol Obstet. 1988 Jan;166(1):69–70. [PubMed] [Google Scholar]
- Vogel S. B., Vair D. B., Woodward E. R. Alterations in gastrointestinal emptying of 99m-technetium-labeled solids following sequential antrectomy, truncal vagotomy and Roux-Y gastroenterostomy. Ann Surg. 1983 Oct;198(4):506–515. doi: 10.1097/00000658-198310000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel S. B., Woodward E. R. The surgical treatment of chronic gastric atony following Roux-Y diversion for alkaline reflux gastritis. Ann Surg. 1989 Jun;209(6):756–763. doi: 10.1097/00000658-198906000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickremesinghe P. C., Dayrit P. Q., Manfredi O. L., Fazio R. A., Fagel V. L. Quantitative evaluation of bile diversion surgery utilizing 99mTc HIDA scintigraphy. Gastroenterology. 1983 Feb;84(2):354–363. [PubMed] [Google Scholar]
- van Heerden J. A., Phillips S. F., Adson M. A., McIlrath D. C. Postoperative reflux gastritis. Am J Surg. 1975 Jan;129(1):82–88. doi: 10.1016/0002-9610(75)90172-5. [DOI] [PubMed] [Google Scholar]
- van Heerden J. A., Priestley J. T., Farrow G. M., Phillips S. F. Postoperative alkaline reflux gastritis. Surgical implications. Am J Surg. 1969 Sep;118(3):427–433. doi: 10.1016/0002-9610(69)90150-0. [DOI] [PubMed] [Google Scholar]
- van Heerden J. A., Priestley J. T., Farrow G. M., Phillips S. F. Postoperative alkaline reflux gastritis. Surgical implications. Am J Surg. 1969 Sep;118(3):427–433. doi: 10.1016/0002-9610(69)90150-0. [DOI] [PubMed] [Google Scholar]