Abstract
Particle-mediated delivery of a DNA expression vector encoding the hemagglutinin (HA) of an H1N1 influenza virus (A/Swine/Indiana/1726/88) to porcine epidermis elicits a humoral immune response and accelerates the clearance of virus in pigs following a homotypic challenge. Mucosal administration of the HA expression plasmid elicits an immune response that is qualitatively different than that elicited by the epidermal vaccination in terms of inhibition of the initial virus infection. In contrast, delivery of a plasmid encoding an influenza virus nucleoprotein from A/PR/8/34 (H1N1) to the epidermis elicits a strong humoral response but no detectable protection in terms of nasal virus shed. The efficacy of the HA DNA vaccine was compared with that of a commercially available inactivated whole-virus vaccine as well as with the level of immunity afforded by previous infection. The HA DNA and inactivated viral vaccines elicited similar protection in that initial infection was not prevented, but subsequent amplification of the infection is limited, resulting in early clearance of the virus. Convalescent animals which recovered from exposure to virulent swine influenza virus were completely resistant to infection when challenged. The porcine influenza A virus system is a relevant preclinical model for humans in terms of both disease and gene transfer to the epidermis and thus provides a basis for advancing the development of DNA-based vaccines.
Influenza A virus is a highly infectious respiratory pathogen of mammals, including humans, and birds (25). Influenza virus causes significant morbidity and mortality in humans and domestic animals, resulting in a substantial global economic burden. The current method for immunization against influenza A virus is a parenterally administered inactivated influenza virus vaccine. Although this mode of immunization is 70 to 90% effective in preventing disease in healthy young adults, it is much less effective in immunocompromised individuals as well as in the elderly. In addition, it may be associated with adverse reactions such as pain, tenderness, myalgia, and rarely, anaphylactic reactions to chicken egg proteins associated with the vaccine as a result of its production in embryonated eggs. Furthermore, antigenic variation in the hemagglutinin (HA) protein of influenza viruses passaged in eggs can reduce the efficacy of this vaccine in eliciting the desired protective immune responses (16, 18, 32).
Subunit vaccines could ameliorate the side effects associated with the inactivated whole influenza virus vaccine (17, 37). Recombinant DNA technology has made it possible to prepare viral proteins from either prokaryotic or eukaryotic cells. Subunit vaccines typically produce fewer undesirable side effects but exhibit less protection against influenza A virus infection than the conventional flu vaccine (30). The decreased efficacy of the exogenously produced viral proteins may be due to the route of administration, changes in protein conformation that could result in the loss of protective epitopes, or presentation of only one viral protein when several are needed for complete protection.
DNA-based vaccines, or the intracellular delivery of DNA vectors that induce antigen expression in vivo, may prove to be more efficacious than the recombinant proteins because the expression of an immunizing protein in the host’s cells mimics aspects of natural infection (22). Presentation of the viral antigen in its native form should function as a better immunogen and enhance the immune response. Nucleic acid immunization induces antigen production that is presented to the immune system associated with major histocompatibility complex class I and class II molecules (29). Antigens presented with major histocompatibility complex class I molecules are recognized by CD8+ cytotoxic T lymphocytes, which destroy virus-infected cells. CD8+ T cells are an integral part of acquired immunity and important in viral clearance (44). DNA vaccines have been successfully used to confer protection against influenza virus in mice, chickens, and ferrets (7, 10, 23, 40); lymphocytic choriomeningitis virus, Plasmodium yoelli, and Mycobacterium tuberculosis in mice (2, 13, 20, 35, 39, 43); and bovine herpesvirus 1 in cattle (6).
Particle-mediated gene delivery is a technology whereby DNA-coated gold microparticles are used to transfect various tissues in vivo (33). Accell gene gun technology utilizes a helium jet to accelerate the DNA-coated gold particles into target tissues. The gene gun DNA vaccine strategy targets gene transfer to the epidermis, which is under constant immune surveillance and is the body’s first defense against pathogens. Swine epidermis is morphologically similar to human epidermis and is widely used as a model for human skin (1, 26). Swine are also similar in scale to humans and are therefore relevant for evaluating gene gun technology for human vaccination.
In the present study, we report the effectiveness of a particle-mediated DNA vaccine, which induces the expression of an influenza A virus HA protein in the epidermis, or the mucosal epithelium of the inferior surface of the tongue, of pigs. This vaccine elicits an immune response and confers protection against a homotypic virus challenge.
MATERIALS AND METHODS
Animal source and maintenance.
Seven to eight-week-old pigs (10 to 15 kg) seronegative for swine influenza virus by hemagglutination inhibition (HI) (28) and enzyme-linked immunosorbent assay (ELISA) (36) were obtained from a commercial source. The pigs were housed at the University of Wisconsin—Madison in biosafety level 2-N rooms for immunizations and then moved to biosafety level 3-N rooms for virus challenge. The animals were maintained in accordance with the guidelines prescribed by the University of Wisconsin Research Animal Resource Center.
Viruses.
A/Swine/Indiana/1726/88 (H1N1) (Sw/IN) was obtained from the influenza virus repository at the University of Wisconsin School of Veterinary Medicine. The virus was cultured in 10-day-old embryonated hens’ eggs and stored at −70°C as previously described (28). Purified Sw/IN was prepared as described elsewhere (36), except that the allantoic fluid was concentrated by the addition of PEG 8000 to 8%; precipitated virus was centrifuged at 8,000 × g prior to purification on 30 to 60% sucrose gradients at 24,000 rpm in an SW28 rotor (Beckman). All manipulations with live virus were conducted under biosafety level 2 or level 3 containment.
Plasmids and DNA preparation.
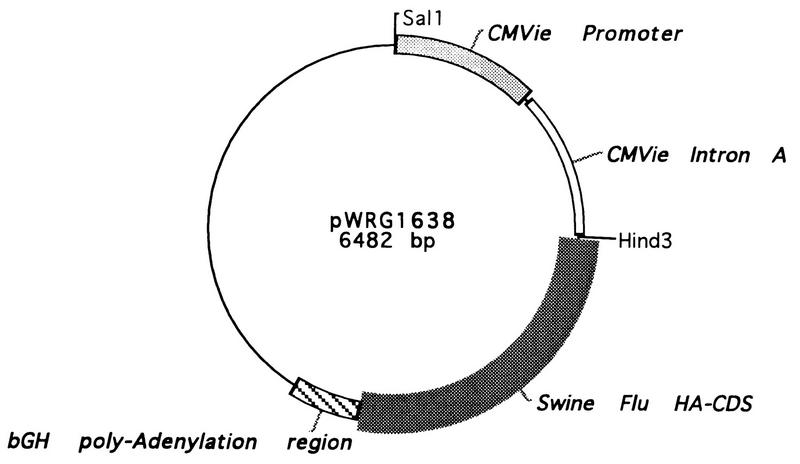
The HA expression plasmid pWRG1638 (Fig. 1) was constructed by ligating the cloned cDNA encoding the HA of Sw/IN into the mammalian expression cassette pWRG7054 (kindly provided by James Fuller, PowderJect Vaccines, Inc.). The cDNA synthesis of the HA gene was done by a one-step PCR method (41). pWRG1638 is a pUC19-based vector and includes the human cytomegalovirus immediate-early enhancer/promoter (CMVie) to drive transcription of the HA coding region. The plasmid also contains the polyadenylation region from the bovine growth hormone gene (4). An influenza nucleoprotein (NP) expression plasmid, pFluNP, that encodes the NP of influenza A virus strain PR/8/34 was kindly provided by K. Irvine (National Cancer Institute). All plasmids were propagated in Escherichia coli XL1-Blue MR. Supercoiled plasmid DNA was prepared on Qiagen columns according to the manufacturer’s instructions.
FIG. 1.
Schematic representation of the HA expression vector pWRG1638. The plasmid was constructed from pWRG7054, a mammalian expression vector containing the CMVie transcriptional enhancer, promoter and intron A regulatory elements and the poly(A) signal of the bovine growth hormone (bGH) in a pUC19 backbone, and a full-length cDNA encoding the HA gene from Sw/IN (H1N1).
Accell cartridge preparation.
Plasmid DNA was coated onto 1- to 3-μm gold particles (DeGussa Corp., South Plainfield, N.J.) as described elsewhere (8). The DNA-coated gold particles were loaded into Tefzel tubing as described elsewhere (29), and the tubing was then cut into 1.27-cm lengths to serve as cartridges for the Accell gene transfer device. The helium pulse Accell device has been described in detail (21). In typical vaccination experiments, each cartridge contained 0.5 mg of gold particles coated with 1.25 μg of plasmid DNA.
Immunofluorescence microscopy.
Chinese hamster ovary (CHO) cells were transfected with pWRG1638 or a control plasmid by using the electric Accell gene transfer device (5). The CHO cells were grown as monolayers on 22- by 22-mm glass coverslips. For transfection, the medium was aspirated and the cells were treated. After treatment, fresh medium was added to the cells, and the mixtures were incubated at 37°C overnight. The cells were fixed with methanol-acetone (50:50) at −20°C and air dried. The fixed cells were incubated with a panel of monoclonal antibodies specific for the HA protein of Sw/IN—3F2c, 1-6b2, 2-15f1, and 7B1b (36)—at room temperature for 60 min, washed, and then incubated with biotinylated goat anti-mouse immunoglobulin (Oncogene Sciences Inc.), washed, and incubated with fluorescein-conjugated streptavidin (Oncogene Sciences Inc.). Fluorescently labeled cells were visualized on a Zeiss Photomicroscope III equipped for fluorescence microscopy.
In vivo gene transfer to skin.
Pigs were immunized by Accell transfer of pWRG1638 into the epidermis in different anatomical regions including the dorsal surface of the ear, the inguinal region, and the lateral thoracic region. Treatment typically included six target sites. Hair was removed with clippers prior to treatment of the lateral thoracic region, but other regions were treated without prior preparation. In addition to epidermal treatments, four pigs were each immunized six times on the inferior surface of the tongue. Accell treatments were conducted at 500 or 600 lb/in2. The gene gun vaccination regimen included a primary immunization followed by booster immunization 4 weeks later.
Parenteral vaccination.
Pigs were vaccinated by intramuscular administration (2 ml) of a commercial swine influenza A vaccine (MaxiVac-FLU; Syntro Vet, Lenexa, Kans.) as directed by the manufacturer. The MaxiVac-FLU vaccine is an oil-in-water vaccine containing influenza A virus (H1N1). Vaccination consisted of a priming administration followed by a booster injection 4 weeks after priming.
Blood collection.
Blood samples from the pigs were collected from the superior vena cava.
ELISAs.
ELISA serology was done with 200 hemagglutination units/well of Sarkosyl-disrupted purified Sw/IN virus diluted in phosphate-buffered saline as described elsewhere (36), with the swine antibodies being measured directly by using a goat anti-swine immunoglobulin G alkaline phosphatase conjugate (Kirkegaard and Perry).
HI assays.
HI assays were performed as described elsewhere (28).
Virus Challenge.
All pigs were challenged by intranasal instillation of 2 × 104 or 2 × 106 50% egg infective doses (EID50s) of Sw/IN virus. Challenged swine were monitored daily for clinical signs. Nasal swabs were collected from each pig on days 1, 3, 5, and 7, and virus titers were determined by limiting-dilution assays in embryonated hens’ eggs (41). Ten days after completion of the challenge, convalescent-phase sera were taken and the animals were euthanized in accordance with guidelines set by the American Veterinary Medical Association (38).
Statistical analysis.
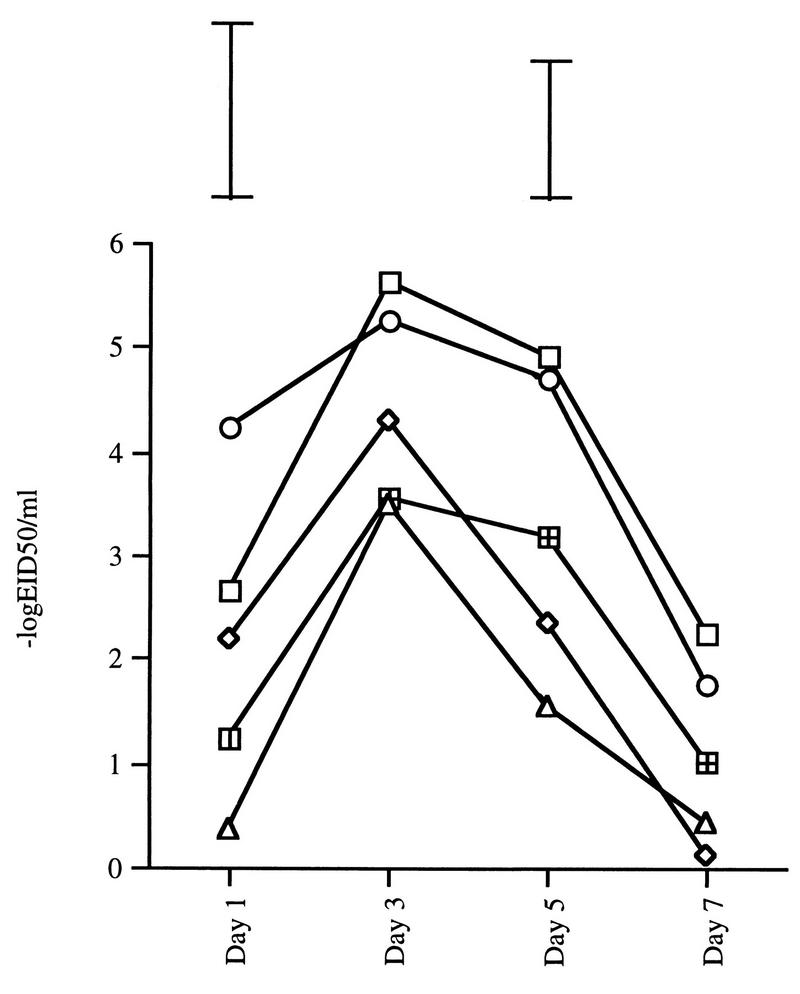
One-way analyses of variance were performed on the data for virus shedding at each sampling point. Least significant difference (LSD) values were calculated for pairwise comparison of treatment groups using α = 0.05. LSD values for comparison of treatment groups where n = 4 are indicated in Fig. 3. These LSD values are conservative for comparisons between the treated groups and the negative-control group (n = 12) because the LSD values for the latter comparisons are smaller than the indicated values. Logarithmic transformations of the antibody titers for different treatment groups were compared by Student’s t test.
FIG. 3.
Geometric mean titers of nasal viral shedding profiles after challenge with Sw/IN. The pigs were immunized by priming and booster administrations of a control plasmid DNA (open squares) (n = 12), an expression plasmid encoding the HA of Sw/IN into the epidermis (diamond) (n = 4) or into the tongue (triangles) (n = 4), or DNA encoding NP of A/PR/8/34 into the epidermis (circles) (n = 3) or by intramuscular injection of a commercial vaccine (crosshatched squares) (n = 4). The pigs were challenged 2 weeks after the booster immunization. None of the convalescent animals exhibited detectable nasal virus following rechallenge. The bars above day 1 and 5 titers represent the LSDs for comparisons between treated pig cohorts (n = 4) at α = 0.05. LSD values for comparison of immunized cohorts to the negative-control group are smaller; thus, the bars shown are conservative for these comparisons.
RESULTS
Expression of the chimeric HA gene in CHO cells.
Preliminary experiments had shown that particle-mediated transfection of swine epidermis with an influenza virus NP expression plasmid induced the production of NP-specific serum antibodies (38a). These results suggested that a particle-mediated DNA vaccine was feasible with swine. The influenza virus HA protein appeared to be a preferable candidate for a vaccine because HI antibody titers correlate with protection against flu (24).
The HA expression plasmid, pWRG1638, used in this study was constructed to express Sw/IN HA in eukaryotic cells (Fig. 1). pWRG1638 contains the CMVie promoter, enhancer, and intron A for transcription initiation, the full-length HA cDNA, and a segment of the 3′ untranslated sequence and polyadenylation signal from the bovine growth hormone gene.
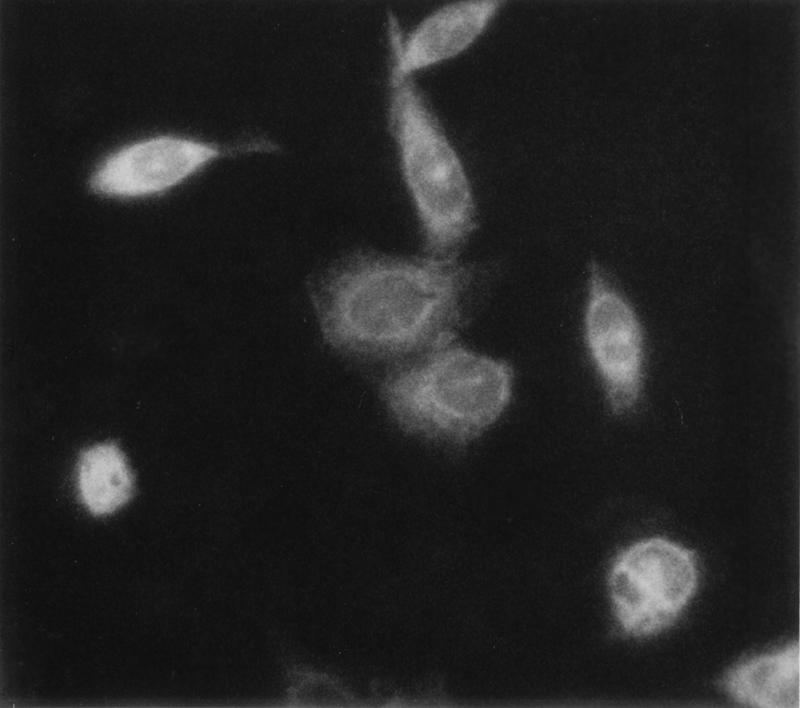
CHO cells were transfected with pWRG1638 to test if the construct would efficiently cause the expression of HA. It was predicted that the expressed HA would be a membrane protein. Therefore, the transfected CHO cells were stained by a panel of monoclonal antibodies to the HA followed by a fluorescein-conjugated secondary antibody. Positive cells were visualized by fluorescence microscopy. The intense staining of the CHO cells (Fig. 2) indicates that the transfected cells are expressing influenza virus HA. CHO cells transfected with pWRG1630, a control plasmid coding for the mature form of epidermal growth factor (1), were not immunoreactive (data not shown).
FIG. 2.
Expression of influenza A virus HA (H1N1) in transiently transfected CHO cells. CHO cells were transfected with pWRG1638, and immunofluorescence microscopy analysis with monoclonal antibodies specific for swine influenza virus HA was performed. Positive cells were visualized on a Zeiss Photomicroscope III equipped for fluorescence microscopy.
Immune responses in vaccinated pigs.
Based on the results from the transfection of CHO cells, a vaccination trial using particle-mediated gene transfer was initiated. The DNA-vaccinated pigs included a group of three pigs vaccinated with the NP expression vector, four pigs vaccinated in the epidermis with the HA expression vector pWRG1638, four pigs vaccinated on the inferior surface of the tongue with pWRG1638, and four pigs vaccinated with a control plasmid, pWRG3510, a plant expression vector (encoding β-glucuronidase from E. coli) which is inactive in mammalian cells. In subsequent experiments, four pigs were vaccinated with a commercial swine influenza A vaccine and four pigs were infected with swine influenza virus to determine protection by conventional vaccines and natural infection, respectively. Serum samples were collected prior to vaccination, prior to booster administration, and 1 week after the booster administration. Two weeks after the booster immunization the animals were challenged with virus, the course of infection was monitored for 7 days, and sera were collected 2 weeks after completion of the challenge.
Table 1 illustrates the ELISA antibody and HI titer changes in six cohorts of pigs during vaccination and after viral challenge. Antibody or HI titers could not be detected in any of the DNA-vaccinated cohorts 4 weeks postpriming. ELISA antibody titers, ranging from 1:200 to 1:1,600, were seen in pigs vaccinated in the epidermis with the NP and HA expression vectors 2 weeks after the boost, and HI antibody titers ranging from 1:10 to 1:160 were seen in the groups vaccinated with pWRG1638. The NP-vaccinated animals did not have HI antibody titers, despite high ELISA antibody titers, because the HI assay detects HA-specific antibodies. The group of pigs vaccinated on the inferior surface of the tongue with pWRG1638 had significantly higher ELISA antibody titers (P = 0.031), ranging from 1:1,600 to 1:12,800, than the pigs vaccinated in the epidermis and lower HI antibody titers, ranging from 1:20 to 1:80. The cohort of pigs vaccinated with inactivated whole virus showed the highest ELISA and HI antibody titers compared to the other groups, while the antibody titers in the natural-infection group were similar to those in the two HA DNA vaccine groups. The control pigs vaccinated with the plant expression vector, pWRG3510, showed no evidence of an anti-influenza virus immune response.
TABLE 1.
ELISA and HI titers for vaccinated pigs
| Vaccination and animal | Reciprocal titera
|
||||
|---|---|---|---|---|---|
| 4 wk postprime
|
2 wk postboost
|
Post- challenge HI | |||
| ELISA | HI | ELISA | HI | ||
| DNA | |||||
| Epidermal NP | |||||
| 1 | <100 | <10 | 1,600 | <10 | 20 |
| 2 | <100 | <10 | 800 | <10 | 80 |
| 3 | <100 | <10 | 1,600 | <10 | 80 |
| Epidermal HA | |||||
| 1 | <100 | <10 | 1,600 | 10 | 160 |
| 2 | <100 | <10 | 800 | 20 | 5,120 |
| 3 | <100 | <10 | 800 | 160 | 5,120 |
| 4 | <100 | <10 | 200 | 40 | 1,280 |
| Tongue HA | |||||
| 1 | <100 | <10 | 3,200 | 80 | 2,560 |
| 2 | <100 | <10 | 3,200 | 40 | 5,120 |
| 3 | <100 | <10 | 1,600 | 20 | 5,120 |
| 4 | <100 | <10 | 12,800 | 80 | 5,120 |
| Inactivated whole virus | |||||
| 1 | 6,400 | 160 | 32,000 | 5,120 | ND |
| 2 | 1,600 | 40 | 4,000 | 80 | ND |
| 3 | 6,400 | 80 | 8,000 | 160 | ND |
| 4 | 800 | 40 | 32,000 | 80 | ND |
| Natural infectionb | |||||
| 1 | 3,200 | 160 | 1,600 | NA | 80 |
| 2 | 800 | 40 | 1,600 | NA | 40 |
| 3 | 1,600 | 160 | 1,600 | NA | 160 |
| 4 | 800 | 20 | 6,400 | NA | 40 |
| Negative control | |||||
| 1 | <100 | <10 | <10 | <10 | 40 |
| 2 | <100 | <10 | <10 | <10 | 80 |
| 3 | <100 | <10 | <10 | <10 | 80 |
| 4 | <100 | <10 | <10 | <10 | 80 |
ND, not determined; NA, not applicable.
The natural-infection cohort was bled 3 weeks after the first infection and 2 weeks after the second infection.
Also of note in Table 1 is the immunological response of the HA-vaccinated animals to viral challenge. The NP-vaccinated cohort and the control cohort show similar postchallenge HI antibody titers, ranging from 1:80 to 1:160. In contrast, the HA DNA-vaccinated cohorts showed HI antibody titers up to 1:5,120 after virus challenge. Even the epidermally vaccinated animal which responded poorly to the prechallenge vaccination in terms of HI antibody titer showed evidence of a hyperimmune response following challenge.
Protection against influenza in pigs immunized with DNA or parenteral vaccine or by natural infection.
A strength of the swine influenza system as a vaccine model is that protective immunity can be measured by challenge with live virus. Each animal was inoculated intranasally with 2 × 106 EID50s of virus. Clinical signs of disease such as lethargy, coryza, and elevated body temperature were monitored and observed during infection but did not provide a reliable measure of disease progression. Nasal virus titers, on the other hand, provided a quantitative indicator of the progress of infection.
Pigs vaccinated with the NP expression vector developed high antibody titers to NP but showed no evidence of protection from viral infection in terms of nasal virus titer (Fig. 3). The pigs vaccinated in the epidermis with the HA expression plasmid became infected but shed lower levels of virus and resolved the infection approximately 2 days earlier than the controls (Fig. 3). Ranking of the individual pigs in the cohort epidermally vaccinated with HA DNA in terms of HI antibody titer correlates directly with the decrease in virus titers in these animals (data not shown).
The pig cohort immunized on the inferior surface of the tongue developed weak HI antibody titers but showed reduced viral shedding over the 7 days. Gene gun administration to the tongue induced erythema with an occasional small necrosis at the center of the treatment site, but there was no evidence of discomfort or a reluctance to eat after immunization. These pigs showed an 18-fold decrease in the mean level of viral shedding relative to the epidermally administered HA DNA vaccine on day 1 (P < 0.05) (Fig. 3).
To provide a perspective for the above results, we investigated the course of infection in two additional cohorts: convalescent animals that gain immunity through prior infection and animals vaccinated with a commercial inactivated whole-virus vaccine. Convalescent cohorts were generated by infecting animals with two different inoculum doses (2 × 104 and 2 × 106 EID50s of virus). Our experiments show that either of these doses is sufficient to infect 100% of unimmunized animals and leads to essentially equivalent progression of infection in terms of nasal virus titer. The animals were then rechallenged 2 weeks after resolution of the initial infection. The parenterally vaccinated cohort was generated by vaccinating animals with a commercially available vaccine, according to the manufacturer’s recommended procedures (3). The vaccination schedule involved a priming immunization and one booster immunization comparable to that used with the DNA immunizations.
Table 1 shows that the commercial vaccine gives rise to high serum antibody titers, detectable by ELISA and HI, in all animals after the priming immunization. Following the second immunization, these animals developed end point ELISA titers ranging from 1:4,000 to 1:32,000 and HI antibody titers between 1:80 and 1:5,120. The Maxi-Vac-FLU-vaccinated animals show roughly one- to twofold-higher HI antibody titers following the full prime-and-boost regimen compared to the gene gun-vaccinated animals, but higher HI antibody titer does not translate into a higher level of protection upon challenge in the case of the conventional vaccine (Fig. 3). In fact, the animal from the conventional-vaccine group with the highest HI antibody titer showed the least protection when challenged with virus.
We were not able to detect virus in the nasal swabs from the pigs that had been previously infected with Sw/IN at any time following a second challenge. This is true even when the animals did not show high HI antibody titers; for example, vaccinated animals showing HI antibody titers in the 1:20-to-1:40 range following vaccination show intermediate protection, whereas the convalescent animals with HI antibody titers in this range were completely protected upon rechallenge.
DISCUSSION
We report the first study of a particle-mediated HA DNA vaccine administered by two routes, parenteral vaccination with inactivated whole virus and natural infection to elicit protective immune responses in pigs. The results show that these vaccination methods induce the production of high levels of influenza virus-specific antibodies and confer various degrees of protection against challenge by homologous virus. In the pig cohort vaccinated in the epidermis with the HA expression plasmid, protection was evidenced by a reduction in the extent and duration of viral shedding. Pigs vaccinated on the inferior surface of the tongue showed more dramatic reduction of virus shed early in infection. Pigs vaccinated with inactivated influenza virus showed a general reduction in viral shedding, and the naturally infected pigs were completely protected against a second challenge.
Ideally, an influenza A vaccine should completely prevent infection. The pigs vaccinated with pWRG1638 by either route or with the conventional vaccine all became infected upon challenge but showed a greater than 1-log-unit reduction in the peak level of shedding and accelerated clearance of the virus relative to the controls. Similar results have been reported by Donnelly et al. (7) for ferrets and nonhuman primates. The exact mechanisms involved in this type of immunity have not been determined, but several important aspects have been described. First, virus-neutralizing anti-HA antibodies can protect against infection with influenza virus if they are present in sufficient quantities at the site of infection (34). Secondly, influenza virus-specific antibody-forming cells (AFCs) are found in the spleen and bone morrow after immunization of mice with DNA encoding influenza virus HA; however, the AFCs are localized at the site of infection only after challenge with influenza virus (15). During the early infection of the epidermally vaccinated pigs, there may be inadequate influenza virus-specific AFCs or antibodies at the site of challenge to neutralize the initial infection. After initiation of the infection, however, the influenza virus-specific AFCs preexisting as a result of vaccination migrate to the upper respiratory tract, where their activities function to neutralize viral progeny and cure the disease (27). This pattern of viral clearance kinetics has been described for other models and was shown for the influenza virus strains used in the challenge reported here (6, 7, 37).
Mucosal immunization with pWRG1638 induced higher ELISA but lower HI influenza virus-specific antibody titers than epidermal immunization with pWRG1638. Although we were able to detect systemic immune responses to the tongue vaccination, the mucosal response to the immunization (influenza virus-specific secretory immunoglobulin A) was below the level of detection. The reduction of nasal virus on day 1, however, is consistent with a mucosal response and is significantly different than the early protection elicited by epidermal administration. These results suggest that mucosal and epidermal immunizations induce different immunological compartments.
We chose the swine influenza model to test particle-mediated DNA vaccine technology in large animals and to try to predict its effectiveness for the human population. Swine are similar to humans in several ways. First, swine epidermis is morphologically similar to human epidermis and is widely used as a model for human skin (1, 11, 12, 26). Second, swine and humans are comparable in size. Third, the swine used in this study are outbred, in contrast to laboratory mouse strains, which are typically isogenic; therefore, the swine model better represents the genetic heterogeneity encountered in natural populations. Finally, the course of infection with influenza A virus in swine is similar to that in humans. In fact, the same influenza A virus strains can infect both swine and humans, and swine have been implicated as a mixing reservoir for the generation of new pandemic strains (42). In contrast, influenza virus challenge in rodents typically leads to lethal pulmonary infection, and protection is scored by survival rather than progression of infection (10, 31, 40).
Particle-mediated DNA influenza vaccines induce strong gene-specific humoral responses in outbred pigs and accelerate the clearance of virus upon subsequent challenge with homologous virus. Accelerated clearance of influenza virus could reduce the potential of transmission as well as the complications associated with prolonged infection. Although the protection elicited by the DNA vaccine was not complete, this methodology has a large potential for improvements. These include the optimization of plasmid vectors (9, 23), the addition of adjuvants or the addition of cytokine genes to modify or boost the host’s immune responses (14, 19), and optimization of the immunization schedule (9). In addition, concomitant immunizations of the epidermis and mucosa, which seem to induce different immune compartments, may provide the immunization regimen necessary for the induction of complete protection from viral challenge.
ACKNOWLEDGMENTS
We are grateful to James Fuller, David Wentworth, and Kari Irvine for providing plasmids used in this study and to Erik Nordheim for help with the statistical analysis.
REFERENCES
- 1.Andree C, Swain W F, Page C P, Macklin M D, Slama J, Hatzis D, Eriksson E. In vivo transfer and expression of a human epidermal growth factor gene accelerates wound repair. Proc Natl Acad Sci USA. 1994;91:12188–12192. doi: 10.1073/pnas.91.25.12188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barry M A, Lai W C, Johnston S A. Protection against mycoplasma infection using expression-library immunization. Nature. 1995;377:632–635. doi: 10.1038/377632a0. [DOI] [PubMed] [Google Scholar]
- 3.Brown G B, McMillen J K. MaxiVacTM-FLU: evaluation of the safety and efficacy of a swine influenza vaccine. Proc Am Assoc Swine Prac. 1994;25:37–39. [Google Scholar]
- 4.Chapman B S, Thayer R M, Vincent K A, Haigwood N L. Effect of intron A from human cytomegalovirus (Towne) immediate-early gene on heterologous expression in mammalian cells. Nucleic Acids Res. 1991;19:3979–3986. doi: 10.1093/nar/19.14.3979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christou P, McCabe D, Martinell B J, Swain W F. Soybean genetic engineering—commercial production of transgenic plants. Trends Biotechnol. 1990;8:145–151. [Google Scholar]
- 6.Cox G J, Lamb T J, Babiuk L A. Bovine herpesvirus 1: immune responses in mice and cattle injected with plasmid DNA. J Virol. 1993;67:5664–5667. doi: 10.1128/jvi.67.9.5664-5667.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donnelly J J, Friedman A, Martinez D, Montgomery D L, Shiver J W, Motzel S L, Ulmer J B, Liu M A. Preclinical efficacy of a prototype DNA vaccine: enhanced protection against antigenic drift in influenza virus. Nat Med. 1995;1:583–587. doi: 10.1038/nm0695-583. [DOI] [PubMed] [Google Scholar]
- 8.Eisenbraum M D, Fuller D H, Haynes J R. Examination of parameters affecting the elicitation of humoral immune responses by particle bombardment-mediated genetic immunization. DNA Cell Biol. 1993;12:791–797. doi: 10.1089/dna.1993.12.791. [DOI] [PubMed] [Google Scholar]
- 9.Fuller D H, Murphy-Corb M, Clements J, Barnett S, Haynes J R. Induction of immunodeficiency virus-specific immune responses in rhesus monkeys following gene gun-mediated DNA vaccination. J Med Primatol. 1996;25:236–241. doi: 10.1111/j.1600-0684.1996.tb00021.x. [DOI] [PubMed] [Google Scholar]
- 10.Fynan E F, Webster R G, Fuller D H, Haynes J R, Santoro J C, Robinson H L. DNA vaccines: protective immunizations by parenteral, mucosal, and gene-gun inoculations. Proc Natl Acad Sci USA. 1993;90:11478–11482. doi: 10.1073/pnas.90.24.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hengge U R, Chan E F, Foster R A, Walker P S, Vogel J C. Cytokine gene expression in epidermis with biological effects following injection of naked DNA. Nat Genet. 1995;10:161–166. doi: 10.1038/ng0695-161. [DOI] [PubMed] [Google Scholar]
- 12.Hengge U R, Walker P S, Vogel J C. Expression of naked DNA in human, pig, and mouse skin. J Clin Invest. 1996;97:2911–2916. doi: 10.1172/JCI118750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huygen K, Content J, Denis O, Montgomery D L, Yawman A M, Deck R R, DeWitt C M, Orme I M, Baldwin S, D’Souza C, Drowart A, Lozes E, Vandenbussche P, Van Vooren J-P, Liu M A, Ulmer J B. Immunogenicity and protective efficacy of a tuberculosis DNA vaccine. Nat Med. 1996;2:893–898. doi: 10.1038/nm0896-893. [DOI] [PubMed] [Google Scholar]
- 14.Irvine K R, Rao J B, Rosenberg S A, Restifo N P. Cytokine enhancement of DNA immunization leads to effective treatment of established pulmonary metastases. J Immunol. 1996;156:238–245. [PMC free article] [PubMed] [Google Scholar]
- 15.Justewicz D M, Morin M J, Robinson H L, Webster R G. Antibody-forming cell response to virus challenge in mice immunized with DNA encoding the influenza virus hemagglutinin. J Virol. 1995;69:7712–7717. doi: 10.1128/jvi.69.12.7712-7717.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz J, Webster R G. Efficacy of inactivated influenza A virus (H3N2) vaccines grown in mammalian cells or embryonated eggs. J Infect Dis. 1989;160:191–198. doi: 10.1093/infdis/160.2.191. [DOI] [PubMed] [Google Scholar]
- 17.Kodihalli S, Sivanandan V, Nagaraja K V, Shaw D, Halvorson D A. A type-specific avian influenza virus subunit vaccine for turkeys: induction of protective immunity to challenge infection. Vaccine. 1994;12:1467–1472. doi: 10.1016/0264-410x(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 18.Kodihalli S, Justewicz D M, Gubareva L V, Webster R G. Selection of a single amino acid substitution in the hemagglutinin molecule by chicken eggs can render influenza A virus (H3) candidate vaccine ineffective. J Virol. 1995;69:4888–4897. doi: 10.1128/jvi.69.8.4888-4897.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kriesel J D, Spruance S L, Daynes R A, Araneo B A. Nucleic acid vaccine encoding gD2 protects mice from herpes simplex virus type 2 disease. J Infect Dis. 1996;173:536–541. doi: 10.1093/infdis/173.3.536. [DOI] [PubMed] [Google Scholar]
- 20.Martins L P, Lau L L, Asano M S, Ahmed R. DNA vaccination against persistent viral infection. J Virol. 1995;69:2574–2582. doi: 10.1128/jvi.69.4.2574-2582.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCabe, D. July 1995. Patent Cooperation Treaty WO 95/19799.
- 22.Michel M L, Davis H L, Schleef M, Mancini M, Tiollais P, Whalen R G. DNA-mediated immunization to the hepatitis B surface antigen in mice: aspects of the humoral response mimic hepatitis B viral infection in humans. Proc Natl Acad Sci USA. 1995;92:5307–5311. doi: 10.1073/pnas.92.12.5307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montgomery D L, Shiver J W, Leander K R, Perry H C, Friedman A, Martinez D, Ulmer J B, Donnelly J J, Liu M A. Heterologous and homologous protection against influenza A by DNA vaccination: optimization of DNA vectors. DNA Cell Biol. 1993;12:777–783. doi: 10.1089/dna.1993.12.777. [DOI] [PubMed] [Google Scholar]
- 24.Murphy B R, Clements M L. The systemic and mucosal response of humans to influenza A virus. Curr Top Microbiol Immunol. 1989;146:107–116. doi: 10.1007/978-3-642-74529-4_12. [DOI] [PubMed] [Google Scholar]
- 25.Murphy B R, Webster R G. Orthomyxoviruses. In: Fields N B, Knipe D M, Howley P M, editors. Field’s Virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1397–1445. [Google Scholar]
- 26.Orgill D P, Butler C E, Regan J F. Behavior of collagen-GAG matrices as dermal replacement in rodent and porcine models. Wounds. 1996;8:151–157. [Google Scholar]
- 27.Palladino G, Mozdzanowska K, Washko G, Gerhard W. Virus-neutralizing antibodies of immunoglobulin G (IgG) but not of IgM or IgA isotypes can cure influenza virus pneumonia in SCID mice. J Virol. 1995;69:2075–2081. doi: 10.1128/jvi.69.4.2075-2081.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palmer D F, Dowdle W R, Coleman M T, Child G C. Advanced laboratory techniques for influenza diagnosis. U. S. Department of Health, Education, and Welfare Immunology Series. Washington, D.C: U.S. Department of Health, Education, and Welfare; 1975. [Google Scholar]
- 29.Pertmer T M, Roberts T R, Haynes J R. Influenza virus nucleoprotein-specific immunoglobulin G subclass and cytokine responses elicited by DNA vaccination are dependent on the route of vector DNA delivery. J Virol. 1996;70:6119–6125. doi: 10.1128/jvi.70.9.6119-6125.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Powers D C, Smith G E, Anderson E L, Kennedy D J, Hackett C S, Wilkinson B E, Volvovitz F, Belshe R B, Treanor J J. Influenza A virus vaccines containing purified recombinant H3 hemagglutinin are well tolerated and induce protective immune responses in healthy adults. J Infect Dis. 1995;171:1595–1599. doi: 10.1093/infdis/171.6.1595. [DOI] [PubMed] [Google Scholar]
- 31.Raz E, Carson D A, Parker S E, Parr T B, Abai A M, Aichinger G, Gromkowski S H, Singh M, Lew D, Yankauckus M A, Baird S M, Rhodes G H. Intradermal gene immunization: the possible role of DNA uptake in the induction of cellular immunity to viruses. Proc Natl Acad Sci USA. 1994;91:9519–9523. doi: 10.1073/pnas.91.20.9519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robertson J S, Bootman J S, Newman R, Oxford J S, Daniels R S, Webster R G, Child G C. Structural changes in the hemagglutinin which accompany egg adaptation of an influenza A (H1N1) virus. Virology. 1987;160:31–37. doi: 10.1016/0042-6822(87)90040-7. [DOI] [PubMed] [Google Scholar]
- 33.Sanford, J. C., E. D. Wolf, and N. K. Allen. 1991. Method for transporting substances into living cells and tissues and apparatus therefore. U.S. Patent 5,036,006.
- 34.Scherle P A, Palladino G, Gerhard W. Mice can recover from pulmonary influenza virus infection in the absence of class I-restricted cytotoxic T cells. J Immunol. 1992;148:212–217. [PubMed] [Google Scholar]
- 35.Sedegah M, Hedstrom R, Hobart P, Hoffman S L. Protection against malaria by immunization with plasmid DNA encoding circumsporozoite protein. Proc Natl Acad Sci USA. 1994;91:9866–9870. doi: 10.1073/pnas.91.21.9866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sheerar M G, Easterday B C, Hinshaw V S. Antigenic conservation of H1N1 swine influenza viruses. J Gen Virol. 1989;70:3297–3303. doi: 10.1099/0022-1317-70-12-3297. [DOI] [PubMed] [Google Scholar]
- 37.Slepushkin V A, Katz J M, Black R A, Gamble W C, Rota P A, Cox N J. Protection of mice against influenza A virus challenge by vaccination with baculovirus-expressed M2 protein. Vaccine. 1995;13:1399–1402. doi: 10.1016/0264-410x(95)92777-y. [DOI] [PubMed] [Google Scholar]
- 38.Smith A W, Houpt K A, Kitchell R L, Kohn D F, McDonald L E, Passaglia M, Thurmon J C, Ames E R. Report of the AVMA panel on euthanasia. J Am Vet Med Assoc. 1986;188:252–268. [PubMed] [Google Scholar]
- 38a.Swain, W. F. Unpublished data.
- 39.Tascon R E, Colston M J, Ragno S, Stavropoulos E, Gregory D, Lowrie D B. Vaccination against tuberculosis by DNA injection. Nat Med. 1996;2:888–892. doi: 10.1038/nm0896-888. [DOI] [PubMed] [Google Scholar]
- 40.Ulmer J B, Donnelly J J, Parker S E, Rhodes G H, Felgner P L, Dwarki V J, Gromkowski S H, Deck R R, DeWitt C M, Friedman A, Hawe L A, Leander K R, Martinez D, Perry H C, Shiver J W, Montgomery D L, Liu M A. Heterologous protection against influenza by injection of DNA encoding a viral protein. Science. 1993;259:1745–1749. doi: 10.1126/science.8456302. [DOI] [PubMed] [Google Scholar]
- 41.Wentworth D E, Thompson B L, Xu X, Regnery H L, Cooley A J, McGregor M W, Cox N J, Hinshaw V S. An influenza A (H1N1) virus, closely related to swine influenza virus, responsible for a fatal case of human influenza. J Virol. 1994;68:2051–2058. doi: 10.1128/jvi.68.4.2051-2058.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wentworth D E, McGregor M W, Macklin M D, Neumann V, Hinshaw V S. Transmission of swine influenza virus to humans after exposure to experimentally infected pigs. J Infect Dis. 1997;175:7–15. doi: 10.1093/infdis/175.1.7. [DOI] [PubMed] [Google Scholar]
- 43.Zarozinski C C, Fynan E F, Selin L K, Robinson H L, Welsh R M. Protective CTL-dependent immunity and enhanced immunopathology in mice immunized by particle bombardment with DNA encoding an internal virion protein. J Immunol. 1995;154:4010–4017. [PubMed] [Google Scholar]
- 44.Zinkernagel R M. Immunology taught by viruses. Science. 1996;271:173–178. doi: 10.1126/science.271.5246.173. [DOI] [PubMed] [Google Scholar]