Abstract
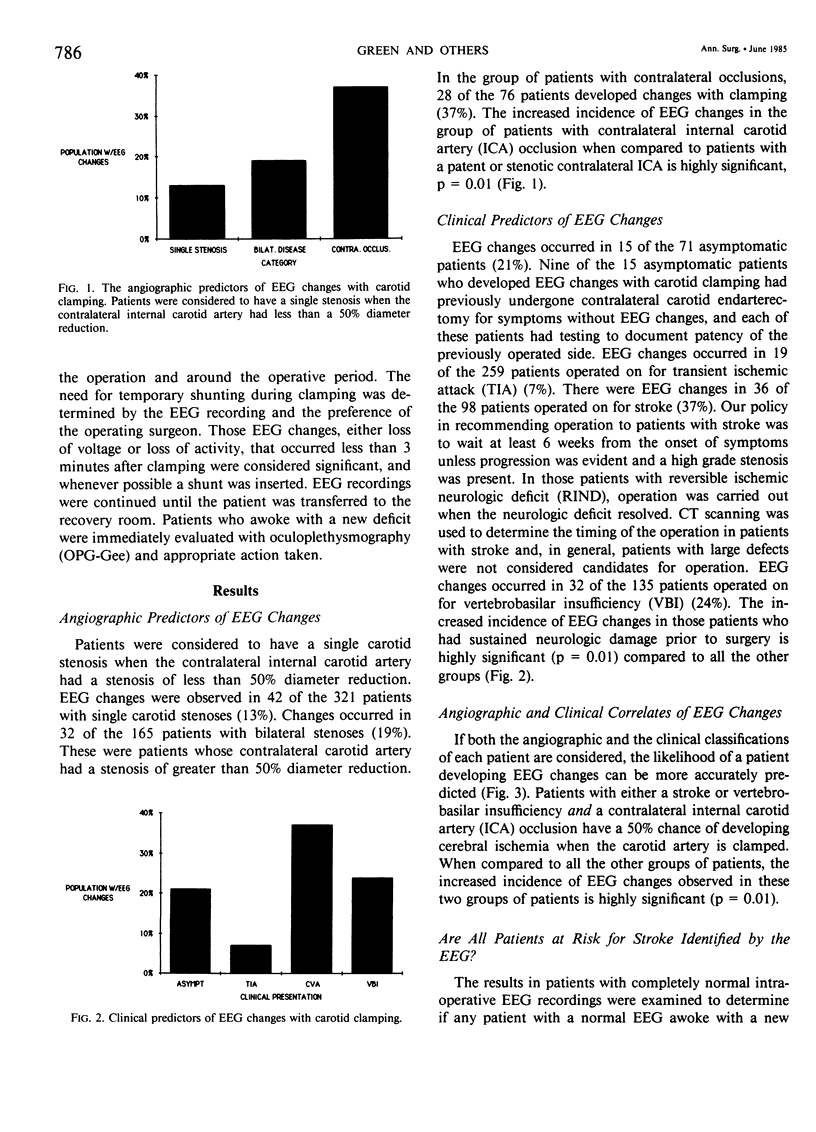
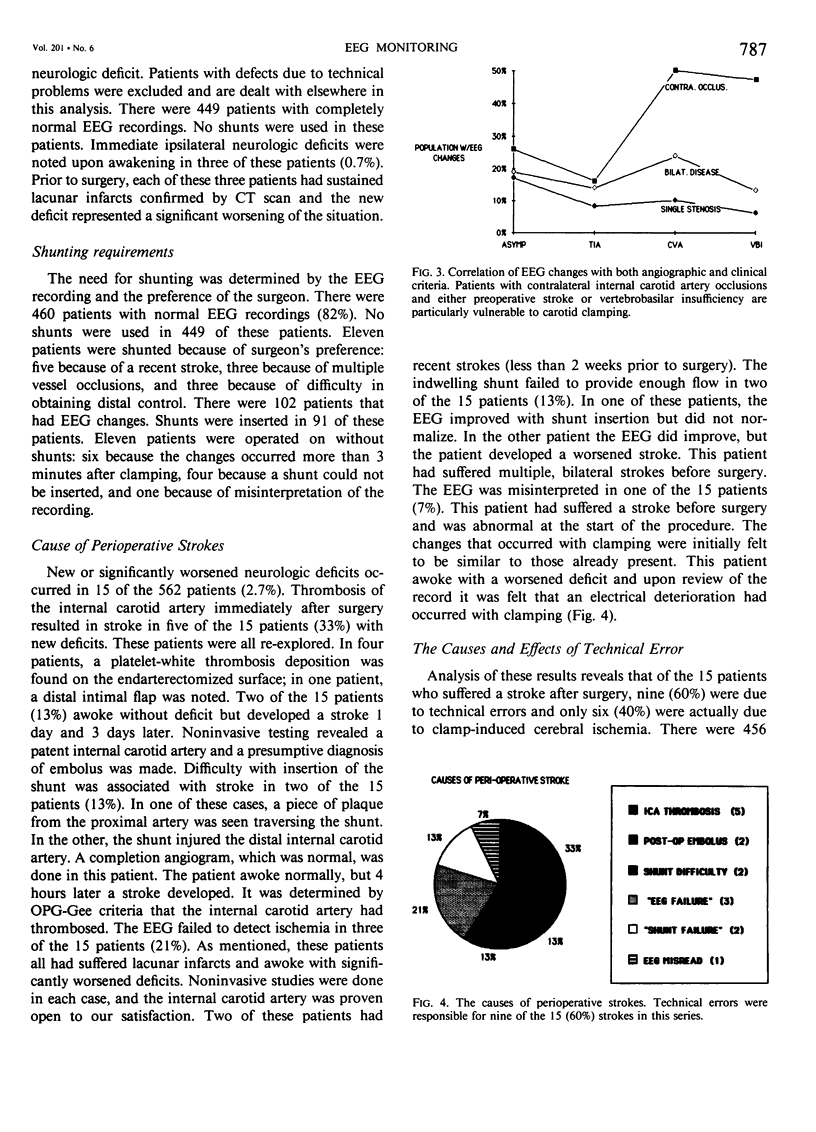
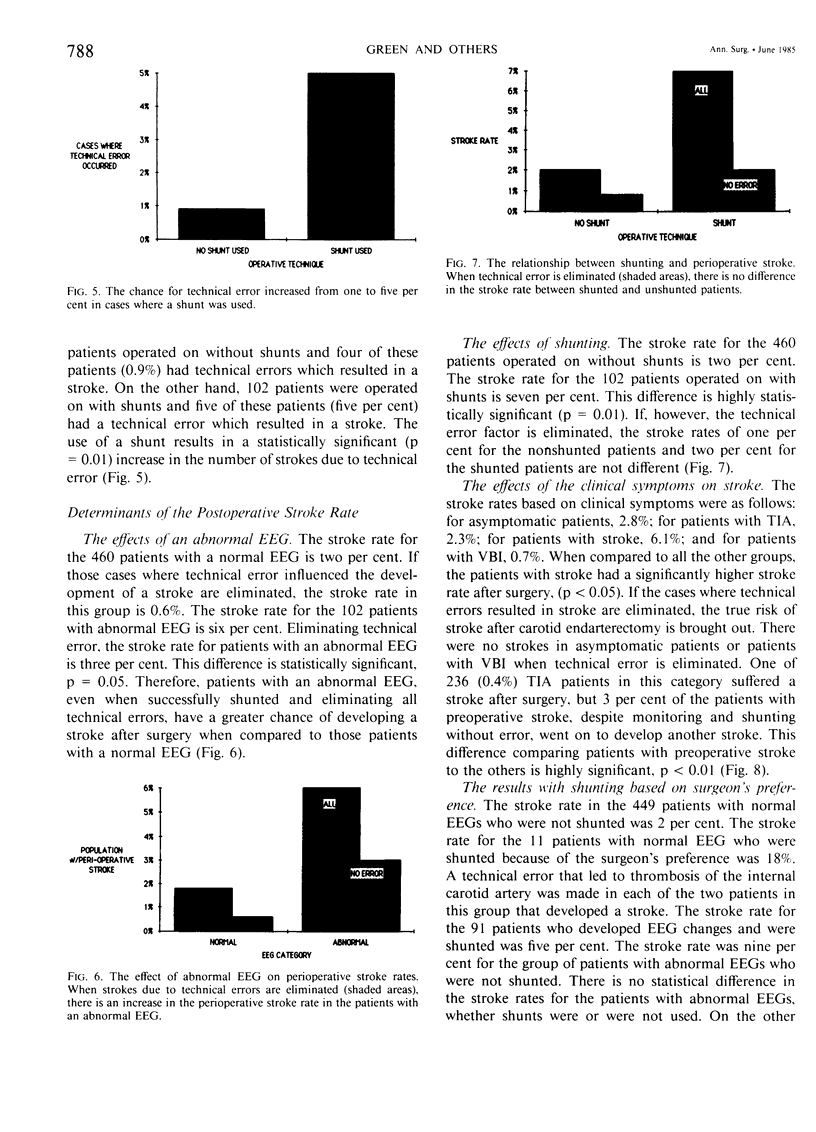
A 5-year experience with 562 carotid endarterectomies, using electroencephalogram (EEG) monitoring and selective shunting, was reviewed. EEG changes occurred in 102 patients (18%). The frequency of EEG changes, as related to cerebral vascular symptoms, was as follows: transient ischemic attacks, seven per cent (19/259); completed strokes, 37% (36/98); vertebral basilar insufficiency, 24% (32/135); asymptomatic, 21% (15/71). Patients with contralateral carotid occlusion exhibited EEG changes in 37% (28/76) of operations. Fifteen patients suffered perioperative strokes (2.6%). Nine of the 15 were associated with a technical problem of either thrombosis of the internal carotid artery (five) or emboli (four). Technical problems were more common when shunts were used (five per cent) than when they were not (0.9%). Patients who suffered strokes prior to surgery were more at risk to develop a perioperative stroke (three per cent) than those not suffering prior strokes (0.3%). The EEG did not change in three patients who had lacunar infarcts prior to surgery and who awoke with a worsened deficit. Our series does not clearly establish the advantages of EEG monitoring, which is expensive (+375/patient) and may not detect ischemia in all areas of the brain. However, the use of shunts may introduce a risk of stroke due to technical error that is equal or greater than the risk of stroke due to hemodynamic ischemia. Since the need for protection is unpredictable by angiographic or clinical criteria, the benefit of EEG monitoring may be in reducing the incidence of shunting in those patients whose tracing remains normal after clamping. The decision to shunt, however, when there is electrical dysfunction after carotid clamping should be based not only on the EEG but also on the clinical signs and computed tomography (CT) scan. Our data does not show a net benefit in selective shunting unless the patient has sustained a stroke prior to surgery.
Full text
PDF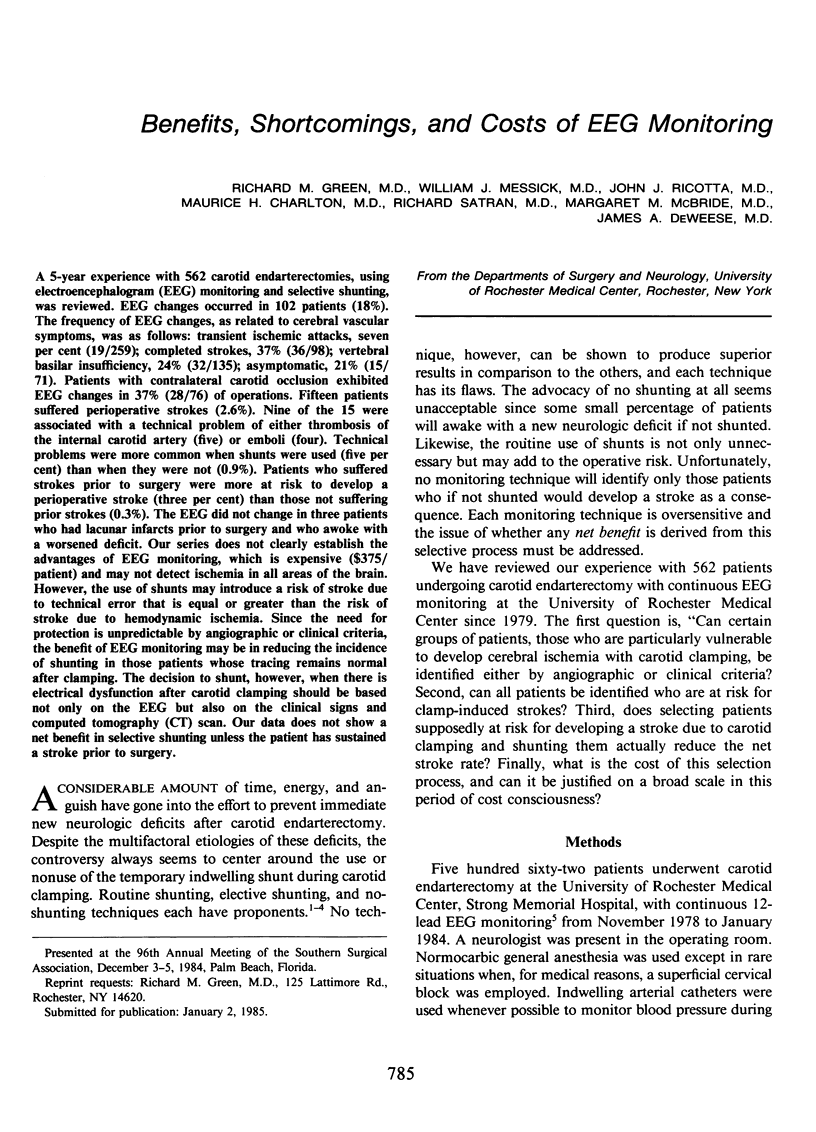
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alberto P., Elisabetta F., Paola R., Uberto R., Alfredo B. The EEG in lacunar strokes. Stroke. 1984 May-Jun;15(3):579–580. [PubMed] [Google Scholar]
- Astrup J. Energy-requiring cell functions in the ischemic brain. Their critical supply and possible inhibition in protective therapy. J Neurosurg. 1982 Apr;56(4):482–497. doi: 10.3171/jns.1982.56.4.0482. [DOI] [PubMed] [Google Scholar]
- Baker J. D., Gluecklich B., Watson C. W., Marcus E., Kamat V., Callow A. D. An evaluation of electroencephalographic monitoring for carotid study. Surgery. 1975 Dec;78(6):787–794. [PubMed] [Google Scholar]
- Baker W. H., Dorner D. B., Barnes R. W. Carotid endarterectomy: is an indwelling shunt necessary? Surgery. 1977 Sep;82(3):321–326. [PubMed] [Google Scholar]
- Baker W. H., Littooy F. N., Hayes A. C., Dorner D. B., Stubbs D. Carotid endarterectomy without a shunt: the control series. J Vasc Surg. 1984 Jan;1(1):50–56. [PubMed] [Google Scholar]
- Callow A. D., Matsumoto G., Baker D., Cossman D., Watson W. Protection of the high risk carotid endarterectomy patient by continuous electroencephalography. J Cardiovasc Surg (Torino) 1978 Jan-Feb;19(1):55–64. [PubMed] [Google Scholar]
- Caplan L. R. Lacunar infarction: a neglected concept. Geriatrics. 1976 Feb;31(2):71–75. [PubMed] [Google Scholar]
- Chiappa K. H., Burke S. R., Young R. R. Results of electroencephalographic monitoring during 367 carotid endarterectomies. Use of a dedicated minicomputer. Stroke. 1979 Jul-Aug;10(4):381–388. doi: 10.1161/01.str.10.4.381. [DOI] [PubMed] [Google Scholar]
- Ferguson G. G. Intra-operative monitoring and internal shunts: are they necessary in carotid endarterectomy? Stroke. 1982 May-Jun;13(3):287–289. doi: 10.1161/01.str.13.3.287. [DOI] [PubMed] [Google Scholar]
- Heiss W. D. Flow thresholds of functional and morphological damage of brain tissue. Stroke. 1983 May-Jun;14(3):329–331. doi: 10.1161/01.str.14.3.329. [DOI] [PubMed] [Google Scholar]
- Imparato A. M., Ramirez A., Riles T., Mintzer R. Cerebral protection in carotid surgery. Arch Surg. 1982 Aug;117(8):1073–1078. doi: 10.1001/archsurg.1982.01380320057015. [DOI] [PubMed] [Google Scholar]
- Kelly J. J., Callow A. D., O'Donnell T. F., McBride K., Ehrenberg B., Korwin S., Welch H., Gembarowicz R. M. Failure of carotid stump pressures. Its incidence as a predictor for a temporary shunt during carotid endarterectomy. Arch Surg. 1979 Dec;114(12):1361–1366. doi: 10.1001/archsurg.1979.01370360015002. [DOI] [PubMed] [Google Scholar]
- Morawetz R. B., Zeiger H. E., McDowell H. A., Jr, McKay R. D., Varner P. D., Gelman S., Halsey J. H. Correlation of cerebral blood flow and EEG during carotid occlusion for endarterectomy (without shunting) and neurologic outcome. Surgery. 1984 Aug;96(2):184–189. [PubMed] [Google Scholar]
- Ott D. A., Cooley D. A., Chapa L., Coelho A. Carotid endarterectomy without temporary intraluminal shunt. Study of 309 consecutive operations. Ann Surg. 1980 Jun;191(6):708–714. doi: 10.1097/00000658-198006000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundt T. M., Jr, Sharbrough F. W., Piepgras D. G., Kearns T. P., Messick J. M., Jr, O'Fallon W. M. Correlation of cerebral blood flow and electroencephalographic changes during carotid endarterectomy: with results of surgery and hemodynamics of cerebral ischemia. Mayo Clin Proc. 1981 Sep;56(9):533–543. [PubMed] [Google Scholar]
- Thompson J. E. Complications of carotid endarterectomy and their prevention. World J Surg. 1979 Jul 16;3(2):155–165. doi: 10.1007/BF01561265. [DOI] [PubMed] [Google Scholar]
- Thompson J. E., Patman R. D., Talkington C. M. Carotid surgery for cerebrovascular insufficiency. Curr Probl Surg. 1978 Dec;15(12):1–68. doi: 10.1016/s0011-3840(78)80010-0. [DOI] [PubMed] [Google Scholar]
- Whitney D. G., Kahn E. M., Estes J. W., Jones C. E. Carotid artery surgery without a temporary indwelling shunt. 1,917 consecutive procedures. Arch Surg. 1980 Nov;115(11):1393–1399. doi: 10.1001/archsurg.1980.01380110125020. [DOI] [PubMed] [Google Scholar]


