Abstract
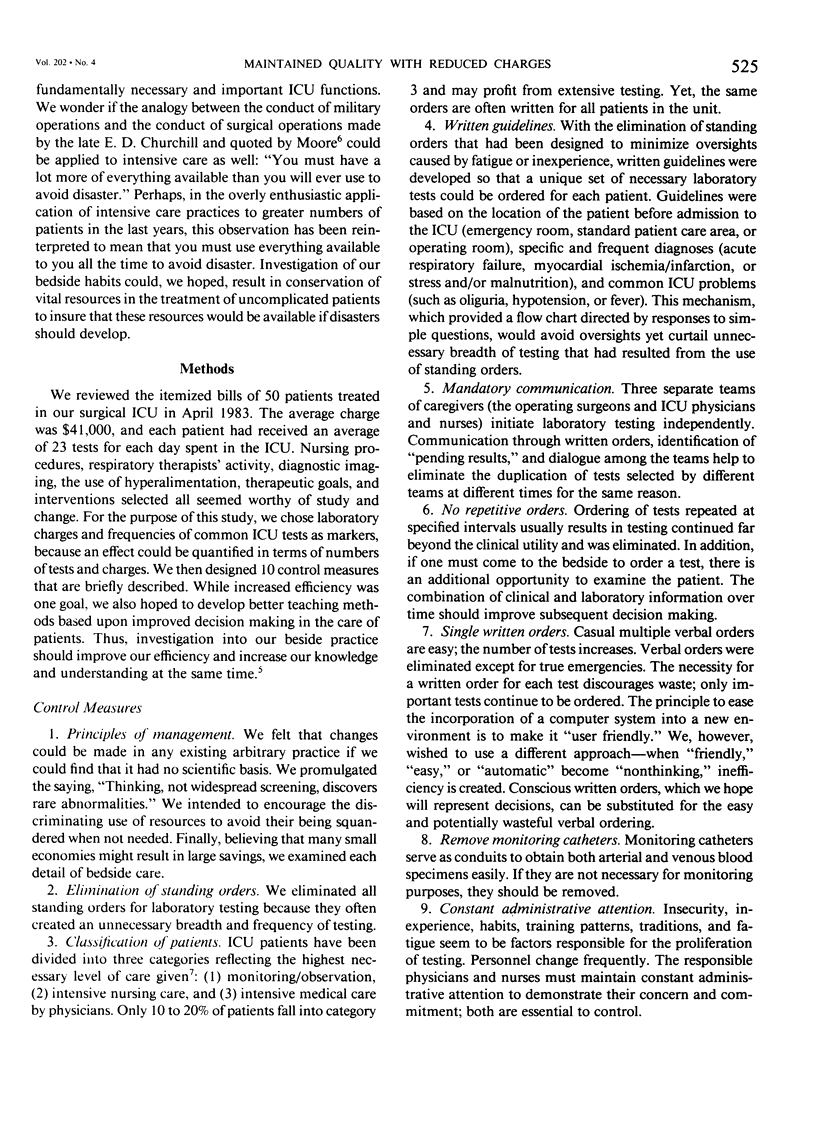
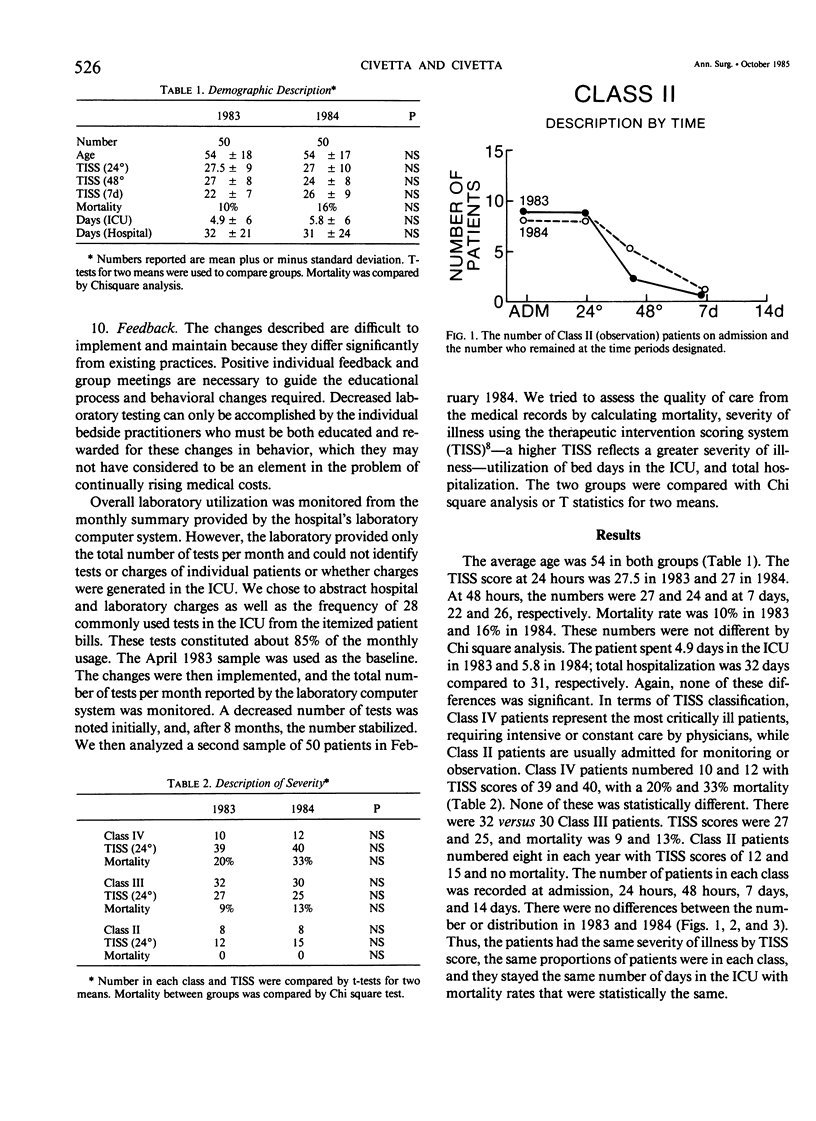
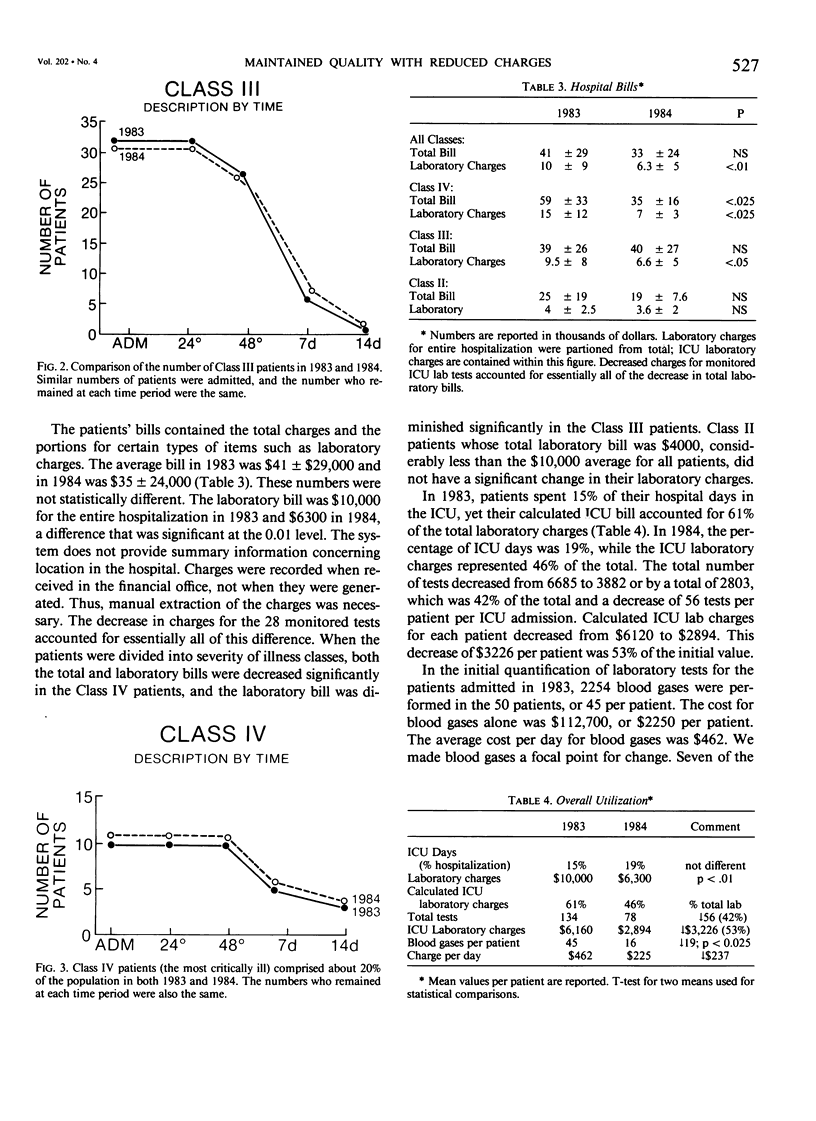
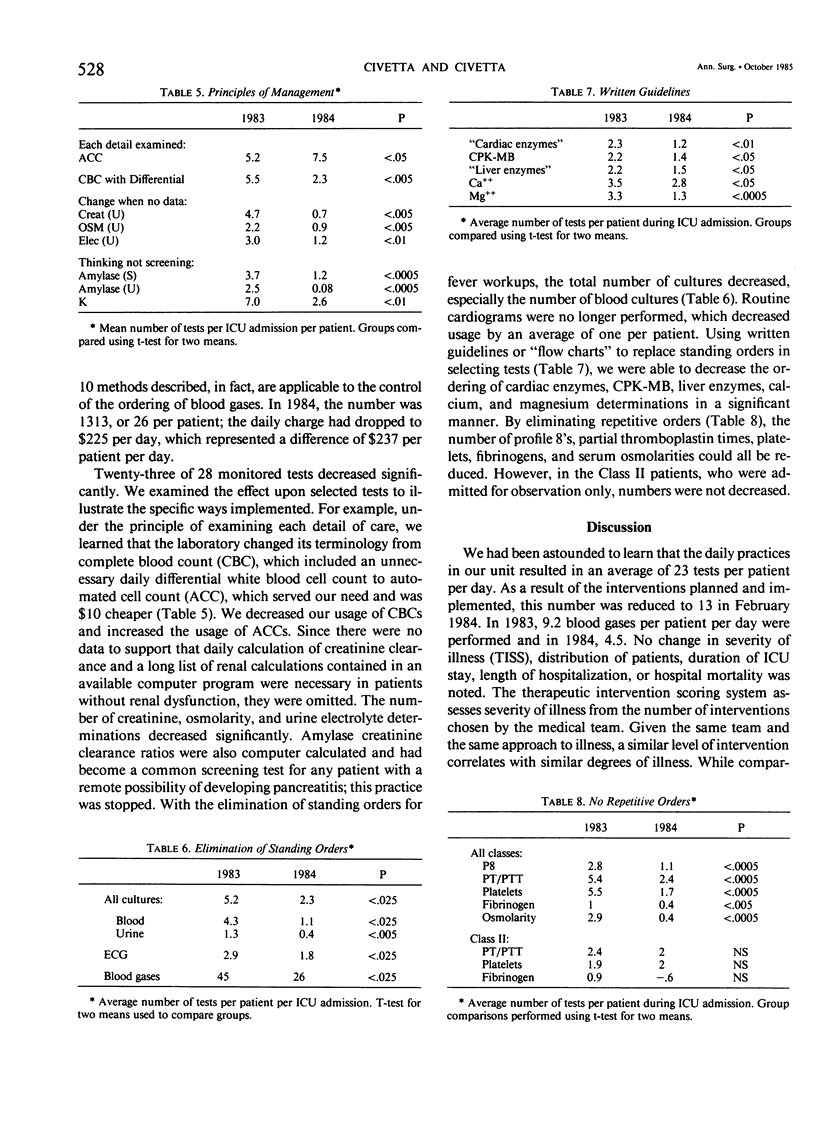
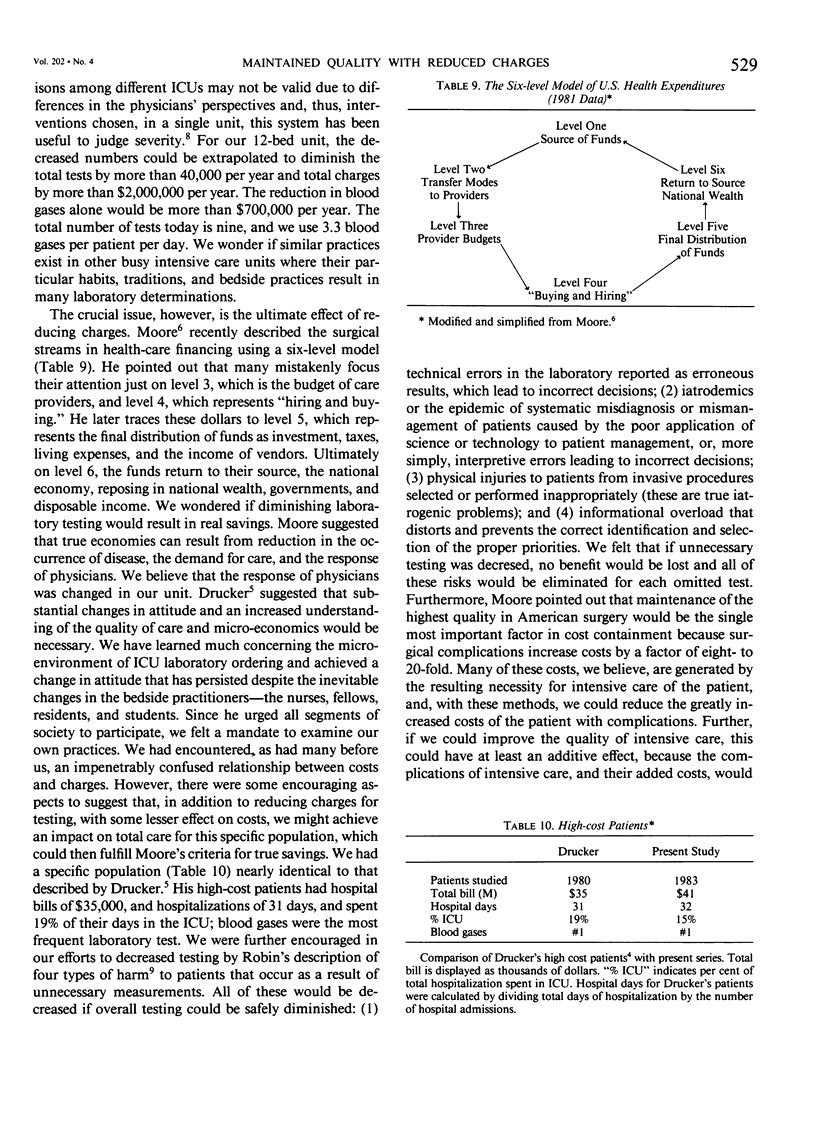
We believed that the dilemma of controlling costs yet maintaining quality of care might be approached in 10 ways designed to improve efficiency of care: principles of management, elimination of standing orders, classification of patients, written guidelines, mandatory communication, no repetitive orders, single order for single test, removal of monitoring catheters, constant administrative attention, and feedback. We monitored quality of care using the therapeutic intervention scoring system (TISS), mortality, utilization of bed days in the ICU, and the total hospitalization of 50 patients treated in April 1983 and, 8 months after the interventions, 50 patients treated in February 1984. There were no differences in the patient population, severity, outcome, or days. The total lab bills were $10,000 in 1983 and $6300 in 1984 (p less than 0.01). The total number of tests decreased by 2803 (42%) from 6685 to 3882, or 56 per patient per admission. Calculated ICU laboratory charges per patient decreased $3226 (53%) from $6210 to $2894. In 1983, while patients spent 15% of their hospital days in the ICU, they accumulated 61% of their total laboratory charges. In 1984, ICU days were 19% and ICU laboratory charges were 46% of the total. If the decrease of $3226 per patient is extrapolated to a year's population, this would decrease charges by over $2,000,000 in one 12-bed surgical ICU.
Full text
PDF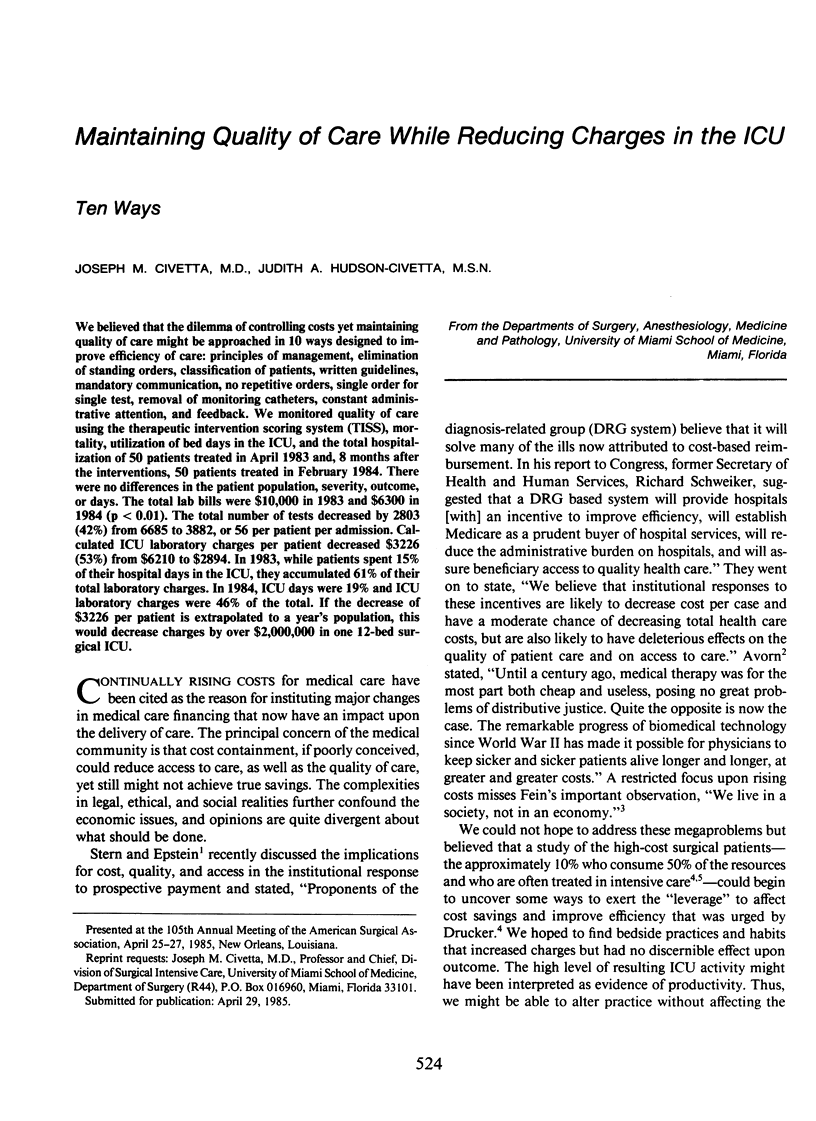
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avorn J. Benefit and cost analysis in geriatric care. Turning age discrimination into health policy. N Engl J Med. 1984 May 17;310(20):1294–1301. doi: 10.1056/NEJM198405173102005. [DOI] [PubMed] [Google Scholar]
- Butler P. W., Bone R. C., Field T. Technology under Medicare diagnosis-related groups prospective payment. Implications for medical intensive care. Chest. 1985 Feb;87(2):229–234. doi: 10.1378/chest.87.2.229. [DOI] [PubMed] [Google Scholar]
- Campion E. W., Mulley A. G., Goldstein R. L., Barnett G. O., Thibault G. E. Medical intensive care for the elderly. A study of current use, costs, and outcomes. JAMA. 1981 Nov 6;246(18):2052–2056. [PubMed] [Google Scholar]
- Civetta J. M. The inverse relationship between cost and survival. J Surg Res. 1973 Mar;14(3):265–269. doi: 10.1016/0022-4804(73)90144-3. [DOI] [PubMed] [Google Scholar]
- Cullen D. J., Civetta J. M., Briggs B. A., Ferrara L. C. Therapeutic intervention scoring system: a method for quantitative comparison of patient care. Crit Care Med. 1974 Mar-Apr;2(2):57–60. [PubMed] [Google Scholar]
- Drucker W. R., Gavett J. W., Kirshner R., Messick W. J., Ingersoll G. Toward strategies for cost containment in surgical patients. Ann Surg. 1983 Sep;198(3):284–300. doi: 10.1097/00000658-198309000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs V. R. A more effective, efficient and equitable system. West J Med. 1976 Jul;125(1):3–5. [PMC free article] [PubMed] [Google Scholar]
- Moore F. D. Surgical streams in the flow of health care financing. The role of surgery in national expenditures: what costs are controllable? Ann Surg. 1985 Feb;201(2):132–141. doi: 10.1097/00000658-198502000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin E. D. A critical look at critical care. Crit Care Med. 1983 Feb;11(2):144–148. doi: 10.1097/00003246-198302000-00019. [DOI] [PubMed] [Google Scholar]
- Singer D. E., Carr P. L., Mulley A. G., Thibault G. E. Rationing intensive care--physician responses to a resource shortage. N Engl J Med. 1983 Nov 10;309(19):1155–1160. doi: 10.1056/NEJM198311103091905. [DOI] [PubMed] [Google Scholar]
- Stern R. S., Epstein A. M. Institutional responses to prospective payment based on diagnosis-related groups. Implications for cost, quality, and access. N Engl J Med. 1985 Mar 7;312(10):621–627. doi: 10.1056/NEJM198503073121005. [DOI] [PubMed] [Google Scholar]
- Zook C. J., Moore F. D. High-cost users of medical care. N Engl J Med. 1980 May 1;302(18):996–1002. doi: 10.1056/NEJM198005013021804. [DOI] [PubMed] [Google Scholar]


