Abstract
Abstract
Introduction
Brain and heart conditions are among the leading causes of illness and mortality in Canada. Heart failure is one of the fastest-growing cardiovascular conditions globally, with more than 100 000 Canadians diagnosed each year. Individuals with heart failure are at significantly increased risk of mental health challenges such as depression, anxiety and stress. However, healthcare services often remain siloed, treating physical and mental health separately. This complicates care for individuals with multiple chronic conditions. This multiyear study will adapt, test and accelerate changes to regional care delivery models in Eastern Ontario to optimise brain-heart health and generate knowledge to support the spread and scale of effective interventions that address community needs and priorities. We aim to: (1) identify resource gaps by mapping available services; (2) document strengths and challenges in care delivery; and (3) co-design, pilot test and evaluate an intervention developed based on the priority gap area(s) identified through objectives (1) and (2).
Methods and analysis
This community-based participatory action research study is led by a research coalition of patient and caregiver partners, care providers and leadership staff from two Ontario Health Teams. In Year 1, we will conduct asset mapping and community consultations with individuals living with heart failure, caregivers, care providers and service organisations to identify care gaps, strengths and opportunities for improvement around modifiable behavioural risk factors and brain-heart health. A scoping review will identify evidence-based strategies to address care gaps and inform the co-design of an intervention focused on supporting individuals with brain-heart interconnected conditions. In Year 2, we will co-design an intervention with community partners for implementation with clinical test sites. Year 3 will involve pilot testing the intervention and conducting outcome and process evaluations. This will inform future spread and scale of the intervention to other brain-heart conditions and new jurisdictions.
Ethics and dissemination
The study is approved by the Bruyère Health Research Ethics Board (M16-24-016). Findings will be disseminated through peer-reviewed publications, conference presentations and knowledge mobilisation activities such as social media, community events and local media outreach, as well as through dedicated engagement with Ontario Health partners and the Brain-Heart Interconnectome Network via retreats and collaborative forums.
Keywords: Health Equity, Community-Based Participatory Research, QUALITATIVE RESEARCH, MENTAL HEALTH, PUBLIC HEALTH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study uses a community-based participatory action research approach, engaging researchers, patients, caregivers and care providers to co-lead the project in ways that integrate research evidence with community and clinical perspectives.
The study includes multiple data sources to identify priority gap areas and inform intervention development. This includes asset mapping, community consultations, a rapid scoping review, implementation planning and evaluation.
The study is based in two Ontario Health Teams, which may limit the generalisability of findings to other community health system settings.
The study focuses on brain-heart interconnected conditions, yet participants may have multiple comorbidities that influence their care experiences in ways not fully captured by this focus.
Introduction
The importance of addressing brain-heart interconnected conditions
Our study is part of the Brain-Heart Interconnectome, an interdisciplinary research programme uniting experts from the University of Ottawa, McGill University, the University of Saskatchewan and over 45 academic, industry and government partners across Canada.1 Supported by a $C109 million grant from the Canada First Research Excellence Fund, the Brain-Heart Interconnectome aims to improve health outcomes for Canadians and people worldwide by accelerating the prevention, detection, treatment and care of brain-heart conditions.
Brain and heart conditions both rank among the top causes of illness and mortality in Canada.2 3 Despite their prevalence, there is still limited understanding of how to best support and care for people living with, or at risk of, interconnected chronic conditions. Heart failure is one of the fastest-growing cardiovascular conditions worldwide, with more than 100 000 Canadians diagnosed each year.4 Individuals with heart failure are at higher risk of experiencing mental health issues such as depression, anxiety and stress compared with the general population.5 Among every 10 people with heart failure, 5–7 are likely to experience depression,6 and about 1 in 5 persons living with heart disease can experience significant anxiety symptoms, such as uncontrollable worry, sleep challenges and difficulty breathing.7 Furthermore, heart failure increases the risk of developing atrial fibrillation, which leads to a greater likelihood of developing stroke,8 impacting the normal brain function of patients.
The interconnected nature of heart failure and mental health conditions, along with associated modifiable risk factors such as exercise, nutrition and smoking cessation, presents a unique challenge to healthcare systems where care services are often siloed, designed to treat one disease in isolation. This complicates care delivery for those with multiple, inter-related chronic conditions.9 10 Modifiable risk factors represent an important yet underaddressed aspect of chronic disease treatment, with their management offering opportunities to improve patient health outcomes.11 12
Healthcare service providers and system planners face challenges in applying scientific knowledge to practice, hindered by barriers such as limited awareness, inaccessible scientific jargon and difficulties in contextualising knowledge. According to a study, only 60% of healthcare follows evidence-based guidelines; 30% is wasteful, low-value or potentially redundant; and 10% is harmful, such as unnecessary surgeries or overprescribing medications.13
One avenue to help bridge this knowledge-to-action gap is to involve community members and decision-makers in the research process from the outset to help them better understand scientific data and how it can be used to strengthen healthcare systems and care delivery. This is the aim of a participatory action research approach, where researchers and interest-holders collaborate to co-create knowledge, to help ensure that research findings and outputs are directly relevant to the community and lead to meaningful improvements in policy and clinical care.14 15 Such collaborative efforts can improve existing care models, enabling them to respond more effectively and promptly to brain-heart interconnect conditions such as heart failure and mental health.
Project description
This 3-year participatory action research project will identify, adapt, test and evaluate changes to the care delivery models used in two Ontario Health Teams in Ontario, Canada. Our project aims to optimise care delivery for adults who have heart failure and also have, or are at risk of, depression, anxiety or stress. The overarching goal is to improve patient health outcomes and the care experience of patients, caregivers and care providers. Established in 2019, Ontario Health Teams are regional entities responsible for organising and delivering comprehensive and coordinated services for patients in their communities.16 To do so, Ontario Health Teams collaborate with partner organisations, such as hospitals, primary care practices, home and community services and social services, to plan and deliver services that account for their population’s needs.17 Currently, there are 58 Ontario Health Teams across the province. Our project is undertaken in collaboration with the Archipel and Great River Ontario Health Teams in the Eastern region of Ontario (see figure 1). They serve a bilingual population, with the Archipel Ontario Health Team having 35% and the Great River Ontario Health Team having 18% of residents with French as their mother tongue, compared with the provincial average of 3%.
Figure 1. Map showing the regions of Ontario Health Teams within the Ontario Health East area.33.

Project objectives
This project has five objectives:
To identify and map the existing services and resources within the Archipel and Great River Ontario Health Team communities that support adults living with heart failure who are at risk of, or are experiencing, mental health challenges, along with their caregivers.
To document gaps, strengths and challenges in current care delivery for heart failure and mental healthcare through community consultations with people with lived or living experience of heart failure, as well as with caregivers, care providers and service organisations.
To inform the co-design of a community-informed intervention through a scoping review of existing, evaluated interventions aimed at improving care delivery for individuals with brain-heart interconnected conditions.
To co-design, test and evaluate a novel intervention in partnership with patients, caregivers, care providers and health system leaders.
To strengthen community partnerships with hospitals, primary care providers, Indigenous communities and policymakers to support knowledge dissemination and intervention uptake.
The timeline below (see figure 2) outlines the sequence and duration of activities required to achieve the study aims.
Figure 2. Project timeline outlining the sequencing and duration of study activities to achieve the stated aims.

Methods
Study design and framework
This community-based participatory action research study aims to empower individuals and communities in our partnered regions by involving them in the transformative process of social change.15 Levesque’s Access to Healthcare Framework will guide our exploration and identification of barriers and facilitators to care access with a focus on approachability, acceptability, availability, affordability and appropriateness of services.18 The framework will inform the co-design of our intervention as it addresses both regional health priorities and the unique challenges identified by our two communities.
Patient and public involvement
The research team is comprised of a research coalition of interest holders, including patient/caregiver partners, primary care physicians and specialists in our chosen brain-heart interconnected condition, and leadership members from the two participating Ontario Health Teams. All partners contribute to the team based on their lived/living experience and/or clinical expertise to ensure their priorities are addressed as we move through the research process. An early example of their engagement was in selecting mental health and heart as the brain-heart dyad of focus in this project. Additionally, our research team consults with an Advisory Board quarterly, which includes key decision-makers at the provincial level from Ontario Health, CorHealth and the Ontario Health Primary Care Division. Ongoing input from the research coalition and Advisory Board provides a mechanism to identify when adjustments are needed. Engagement with these diverse partners will help ensure that study methods and outputs remain responsive to patient and caregiver needs, while also being feasible for care providers and Ontario Health Teams. Decisions will be made collaboratively, with consensus pursued through ongoing discussions to balance the needs of interest holders and feasibility within the care context.
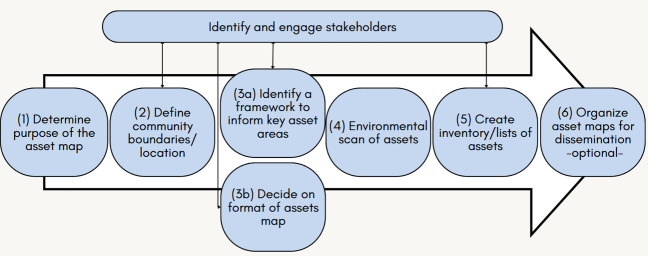
Asset mapping
Asset mapping is a method for identifying and cataloguing the resources and services within a community.19 In Year 1, we will undertake asset mapping in the catchment areas of the Great River and Archipel Ontario Health Teams to identify gaps and suggest areas where care delivery may need to be improved. Figure 3 outlines the steps we will use in our asset mapping process.19
Figure 3. Approach to asset mapping adapted from Turin et al.19.
We will use the 10 Quality Statements for Heart Failure developed by Health Quality Ontario20 to guide the categorisation and analysis of key asset areas, helping us determine which areas of care have sufficient assets and where assets are missing. To analyse our asset maps, we will provide descriptive statistical analysis of the types and number of services available and their distribution across different locations, analyse counts for language offerings of services, accessibility, format of the service (eg, virtual, in-person, group) and consider service costs. Services are anticipated to include those that support heart failure and mental health management as well as broader socioeconomic risk factors, for example, exercise programmes, mental health supports, cessation programmes and nutritional services.
Community consultations
The asset maps will be discussed in community consultations to help researchers gain a deeper understanding of participants’ awareness, utilisation and experiences with the services available in their region. We will consult with three target groups: (1) adults (18+) living with heart failure and their caregivers, (2) care providers delivering clinical care to our brain-heart interconnected condition population and (3) members of service organisations offering health or social services relevant to brain-heart interconnected conditions. This could include cardiac rehabilitation programmes, support groups, smoking cessation programmes and other related services.
Table 1 provides a high-level summary of participant recruitment for each target group.
Table 1. High-level summary of the methods and recruitment strategy for each target group.
| Adults (18+) with heart failure and their caregivers | Care providers | Members of service organisations | |
|---|---|---|---|
| Eligibility | Speak English or French. Ability to provide informed consent. Reside in our Ontario Health Team regions. |
||
| Adults with heart failure and their caregivers living in our two Ontario Health Team regions. | Primary care physicians, cardiologists, psychologists and psychiatrists in our two Ontario Health Team regions. | Leaders and service delivery personnel within organisations serving the target population. | |
| Approach | Focus groups (60–90 min) or semi-structured interviews (30–45 mins). | Semi-structured Interviews (30–45 min). | Semi-structured Interviews (30–45 min). |
| Target sample size | 12–15 participants | 10–15 semi-structured interviews. | 6–10 semi-structured interviews. |
| Diversity sought | Role: (patient/caregiver), gender, age, ethnicity (white/non-white), language (French/English) and geography (urban/rural residence) | Role: (clinical/support staff within the clinic), profession (primary care physician, cardiologist, psychologist/psychiatrist), setting (community/hospital) | Role: type of services provided |
| Recruitment strategy | Purposive snowball sampling34 to achieve diversity in gender, age, ethnicity, education, income and rurality. Multipronged recruitment approach:
|
||
Consultations will take the form of either focus groups (four to six participants, duration: 60–90 min) or individual/dyadic semi-structured interviews (one to two participants, duration: 30–45 min). The proposed sample size for each target group is designed to achieve data saturation, which is defined as the point where no new themes or insights emerge from the data, and additional data collection no longer contributes to the overall analysis.21 We will ensure diversity in our sample across key demographic and contextual factors (table 1). Participants will choose whether to participate in a semi-structured interview or a focus group, either in person or virtual, using Microsoft Teams. The focus groups/interviews will contain open-ended questions using a guide co-developed with the Research Coalition. Each participant will also complete a demographic questionnaire.
Data from our interviews will be transcribed by a third-party agency and managed using the qualitative software package MAXQDA 2022.22 Our inductive data analysis will be guided by Braun and Clarke’s23 approach to reflexive thematic analysis to facilitate the identification and analysis of patterns or themes in a given data set using a six-phase process. We will interpret the thematic findings using the 10 Quality Statements for Heart Failure20 and Levesque’s Access to Healthcare Framework18 to assist in pinpointing critical areas for improvement linked to modifiable behavioural risk factors. To support trustworthiness and rigour in qualitative data collection, the research team includes members from multidisciplinary backgrounds, and we will continue to engage our Research Coalition throughout the project. We will meet all aspects of COREQ (Consolidated criteria for Reporting Qualitative research), a well-established reporting checklist for qualitative research.
Scoping review
Consultation findings will be used to identify a priority care gap in collaboration with our Research Coalition. A rapid scoping review using JBI methods24 will be used to identify pre-existing strategies that could be used to address this gap. Scoping reviews are a tool to synthesise existing knowledge on interventions, outcomes, contexts and populations studied in the field.24 25 Eligibility criteria for the review will include evaluated interventions aimed at improving care delivery for cardiac and mental health conditions in high-income countries. We will include systematic reviews, primary studies with comparison groups and pre–post-evaluation studies. Findings will be synthesised in tables and charts indicating each strategy, study type, outcomes and evidence strength.
Intervention co-design
Using results from the scoping review as a starting point, we will employ the Double Diamond framework26 to guide our Research Coalition in the co-design of a novel intervention to address our priority gap in heart failure-mental healthcare. The Double Diamond framework has four stages: (1) discover, (2) define, (3) develop and (4) deliver.26 Co-design sessions will take place primarily during monthly coalition meetings, with additional one-on-one meetings held as needed to support deeper engagement and accommodate availability. The research team will consult with leadership and operational staff in each Ontario Health Team to ensure the intervention is appropriately adapted for implementation within their respective service and organisational contexts. To ensure that the intervention is responsive to the needs of diverse communities, we will conduct targeted consultations to gain the perspectives of five to eight community organisations serving equity-deserving populations that may not be fully captured in coalition discussions and adapt the intervention for relevance, accessibility and cultural safety.
Intervention planning, testing and evaluation
Using the Consolidated Framework for Implementation Research27 to guide our understanding of the contextual factors influencing intervention planning and delivery within the Archipel and Great River Ontario Health Teams, we will partner with the executive support teams at each Ontario Health Team to engage in system mapping28 to visualise the structures, partnerships, workflows and service ecosystems that make up the current regional care delivery model for adults with heart failure and mental health conditions. System mapping will be used to document key elements, such as partner organisations, referral pathways and resource flows, as well as identify gaps, opportunities and potential leverage points for implementation. These insights will inform the development of a tailored implementation strategy for each test site in our feasibility trial.
We will pilot test the intervention in 6–10 care sites in the Archipel and Great River Ontario Health Team regions. We will use a hybrid 1 design to measure effectiveness for patients through an outcome evaluation while also conducting process evaluations at each test site to understand the feasibility of intervention implementation in real-world clinical settings.29 In keeping with our participatory action research approach, all decisions regarding evaluation frameworks and measurement strategies will be made collaboratively with our Research Coalition. The research team will provide implementation recommendations, such as applying the RE-AIM (Reach, Effectiveness, Adoption, Implementation and Maintenance) framework30 31, and developing a fidelity checklist32 to monitor delivery across sites. However, primary and secondary outcome metrics will be co-developed with and validated by the Research Coalition to ensure alignment with community priorities and context.
Discussion
This study is the first to use a system-wide lens to assess and address multiple communities’ care needs related to interconnected heart failure and mental health conditions. By applying a participatory action research approach, the research team will find ways to better support adults with our targeted conditions, along with their caregivers and care providers, to improve care access and health outcomes. We have co-produced this protocol with community partners, ensuring that they play an integral role in shaping this research project and its priorities. Together, we will support our Ontario Health Team partners in developing and implementing a novel intervention to address a priority care in the chronic disease management of brain-heart conditions. We will use a pragmatic and community-tailored approach to optimise the project’s outcomes. We aim to understand and address potential issues to improve adaptability, allowing us to develop processes and tools that can be disseminated and scaled for use by similar communities across the province and by the Brain-Heart Interconnectome Hub in future collaborations.
Anticipated limitations and mitigation strategies
Recruiting participants with heart failure, particularly those experiencing mental health issues, presents significant challenges due to the hard-to-reach nature of this population. To address this, we will work closely with cardiac clinics, primary care networks and mental health programmes, leveraging their established relationships with patients. Additionally, mental health conditions like anxiety and depression can carry stigma, potentially deterring participants from discussing their experiences openly, especially in group settings. We will offer one-on-one interviews or interviews with caregivers or loved ones present as an alternative to group discussions, creating a more supportive and comfortable environment.
The project’s primary collaboration with two Ontario Health Teams may limit the generalisability of the results to other Ontario Health Teams across the province. To mitigate this, we will continue to engage and share our findings with Ontario Health to solicit guidance on how to increase the transferability of our work.
Ethics and dissemination
Ethics approval
This study has received approval from the Bruyère Health Research Ethics Board (M16-24-016) and will be conducted in accordance with the Declaration of Helsinki. Written and verbal informed consent will be obtained from all participants, including consent to be audio-recorded. De-identified interview data will be stored on secure servers at Bruyère Health and will not be made publicly available due to privacy considerations.
Dissemination
Findings from this study will be disseminated through peer-reviewed publications and conference presentations, as well as targeted knowledge mobilisation activities. These will include community engagement strategies such as social media, local community events and media outreach, along with tailored policy and research briefings for our Ontario Health partners. Results will also be shared with the Brain–Heart Interconnectome Research Network through retreats and collaborative forums to inform future cross-community initiatives. Evaluation findings from intervention testing will inform refinements and highlight opportunities for scale-up and integration into broader care models across Ontario and beyond. This study will position the research team to conduct a large-scale cohort randomised trial should the results demonstrate intervention effectiveness.
Acknowledgements
We appreciate the support of Brain-Heart Interconnectome and our research coalition members, including the Ontario Health Team’s directors and staff, lead physicians, patient/caregiver partners and other interest-holders, for their time, input and engagement with the project.
Footnotes
Funding: This study is part of the University of Ottawa Brain Heart Interconnectome Research Initiative, which is funded by the Canada First Research Excellence Fund (BHI 24–126; GR005166 – BHI Foundations/Theme; BHI 24–126T). The principal researcher, Krystal Kehoe MacLeod, is supported by a Canadian Institutes of Health Research Postdoctoral Fellowship Award (Grant No. 187961) and a Brain Heart Interconnectome Postdoctoral Award (BHI 24 - 126-2T/1).
Prepub: Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2025-109113).
Patient consent for publication: Consent obtained directly from patient(s).
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Author note: KKML is a Postdoctoral Fellow at Bruyere Health Research Institute and the Director of the Centre for Care Access and Equity Research (CCAER). At CCAER, our aim is to improve access to culturally informed health and social care with a focus on challenging the social, structural and systemic inequities faced by underserved communities. We use intersectionality, health equity, organisational management and feminist political economy theoretical frameworks and specialise in mixed methods studies that combine qualitative methods with population-level health administrative data. We prioritise community-based research approaches and integrated knowledge mobilization to involve our community partners across the entire research process. Our work is funded through grants from Health Canada, the Canadian Institutes of Health Research (CIHR), the Social Sciences and Humanities Research Council of Canada (SSHRC), the Centre for Aging + Brain Health Innovation at Baycrest, the New Brunswick Research Foundation, l’Association Médicale Universitaire Montfort and the University of Ottawa.
References
- 1.University of Ottawa; 2024. Brain-heart interconnectome | research and innovation.https://www.uottawa.ca/research-innovation/bhi Available. [Google Scholar]
- 2.Heart and Stroke; 2023. What we don’t know can hurt us when it comes to heart and brain health.https://www.heartandstroke.ca/what-we-do/media-centre/news-releases/what-you-dont-know-about-heart-disease-and-stroke-could-hurt-you Available. [Google Scholar]
- 3.Public Health Agency of Canada Report from the canadian chronic disease surveillance system: heart disease in canada, 2018. 2018 https://www.canada.ca/en/public-health/services/publications/diseases-conditions/asthma-chronic-obstructive-pulmonary-disease-canada-2018.html Available.
- 4.Heart and Stroke Foundation Falling short how canada is failing people with heart failure-and how we can change that 2022 spotlight on heart failure. 2022
- 5.Rashid S, Qureshi AG, Noor TA, et al. Anxiety and Depression in Heart Failure: An Updated Review. Curr Probl Cardiol. 2023;48 doi: 10.1016/j.cpcardiol.2023.101987. [DOI] [PubMed] [Google Scholar]
- 6.Heart and Stroke Foundation Living with heart failure: resources to help you manage your heart failure
- 7.University of Ottawa Heart Institute Heart failure: a guide for patients and caregivers. 2024
- 8.Bilato C, Bordignon S, Chiara Corti M. Atrial fibrillation associated with heart failure, stroke and mortality. www.jafib.com n.d. Available. [DOI] [PMC free article] [PubMed]
- 9.Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition--multimorbidity. JAMA. 2012;307:2493–4. doi: 10.1001/jama.2012.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ploeg J, Matthew-Maich N, Fraser K, et al. Managing multiple chronic conditions in the community: a Canadian qualitative study of the experiences of older adults, family caregivers and healthcare providers. BMC Geriatr. 2017;17 doi: 10.1186/s12877-017-0431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meeker D, Goldberg J, Kim KK, et al. Patient Commitment to Health (PACT-Health) in the Heart Failure Population: A Focus Group Study of an Active Communication Framework for Patient-Centered Health Behavior Change. J Med Internet Res. 2019;21:e12483. doi: 10.2196/12483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng R, Sutradhar R, Yao Z, et al. Smoking, drinking, diet and physical activity—modifiable lifestyle risk factors and their associations with age to first chronic disease. Int J. 2020;49:113–30. doi: 10.1093/ije/dyz078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: the 60-30-10 Challenge. BMC Med. 2020;18:102. doi: 10.1186/s12916-020-01563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health. 2006;60:854–7. doi: 10.1136/jech.2004.028662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cornish F, Breton N, Moreno-Tabarez U, et al. Participatory action research. Nat Rev Methods Primers. 2023;3 doi: 10.1038/s43586-023-00214-1. [DOI] [Google Scholar]
- 16.Government of Ontario Ontario health teams. 2024. https://www.ontario.ca/page/ontario-health-teams Available.
- 17.Ontario Health Ontario health teams: guidance for health care providers and organizations. 2023. https://www.ontario.ca/files/2024-01/moh-oht-hcp-guidance-doc-en-2024-01-22.pdf Available.
- 18.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turin TC, Shahid M, Vaska M. Asset Mapping as a Tool for Identifying Resources in Community Health: A Methodological Overview. J biomed anal. 2019;2:13–25. doi: 10.30577/jba.2019.v2n1.22. [DOI] [Google Scholar]
- 20.Health Quality Ontario Heart failure care in the community for adults. 2019
- 21.Faulkner SL, Trotter SP. The International Encyclopedia of Communication Research Methods; 2017. Data saturation.https://onlinelibrary.wiley.com/doi/book/10.1002/9781118901731 Available. [Google Scholar]
- 22.VERBI Software . Berlin: VERBI Software; 2022. MAXQDA 2022. [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 24.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis. 2020;18:2119–26. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 25.Tricco AC, Lillie E, Zarin W, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16 doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Design Council The double diamond. 2024. https://www.designcouncil.org.uk/our-resources/the-double-diamond/ Available.
- 27.Safaeinili N, Brown‐Johnson C, Shaw JG, et al. CFIR simplified: Pragmatic application of and adaptations to the Consolidated Framework for Implementation Research (CFIR) for evaluation of a patient‐centered care transformation within a learning health system. Learning Health Systems. 2020;4 doi: 10.1002/lrh2.10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbrook-Johnson P, Penn AS. Oxford; 2022. Systems mapping: how to build and use causal models of systems.https://gum.co/systemdiagrams Available. [Google Scholar]
- 29.Curran GM, Bauer M, Mittman B, et al. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217–26. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwan BM, McGinnes HL, Ory MG, et al. RE-AIM in the Real World: Use of the RE-AIM Framework for Program Planning and Evaluation in Clinical and Community Settings. Front Public Health. 2019;7:345. doi: 10.3389/fpubh.2019.00345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health. 2013;103:e38–46. doi: 10.2105/AJPH.2013.301299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carroll C, Patterson M, Wood S, et al. A conceptual framework for implementation fidelity. Implement Sci. 2007;2:40. doi: 10.1186/1748-5908-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Great River Ontario Health Team Who we are. 2023
- 34.Parker C, Scott S, Geddes A. SAGE research methods foundations. SAGE Publications Ltd; 2020. Snowball sampling. [Google Scholar]