Abstract
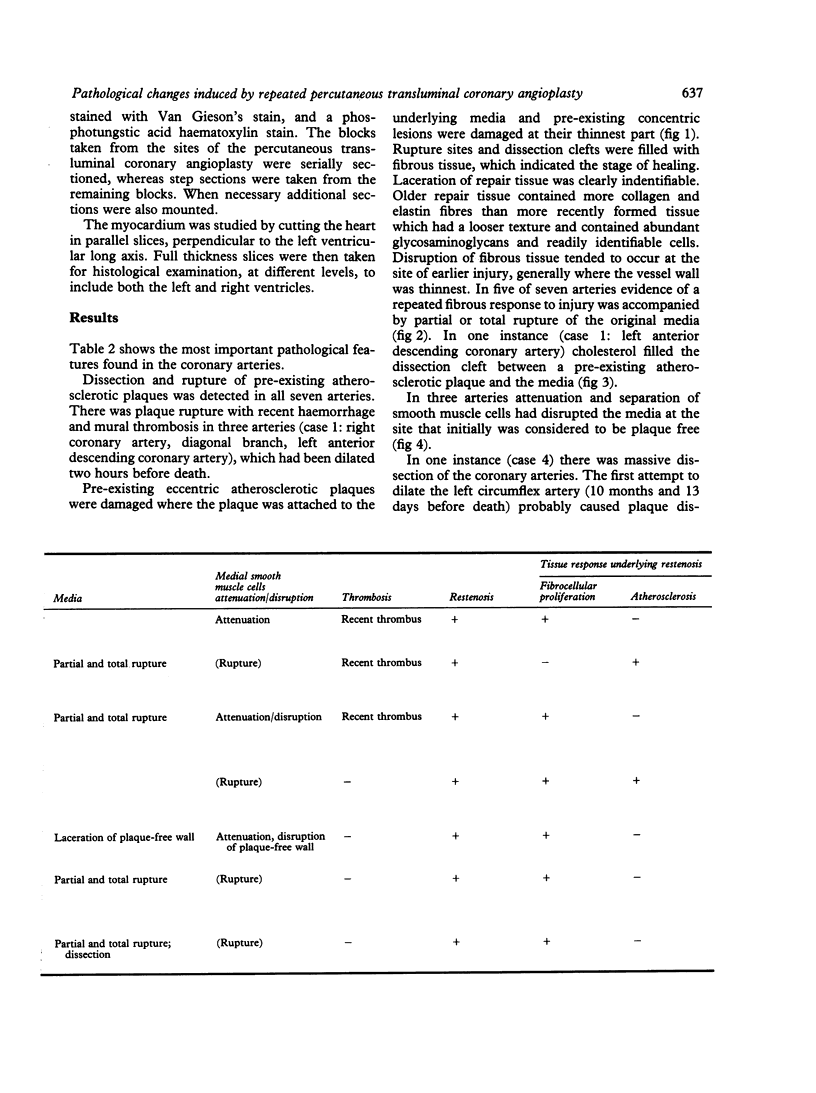
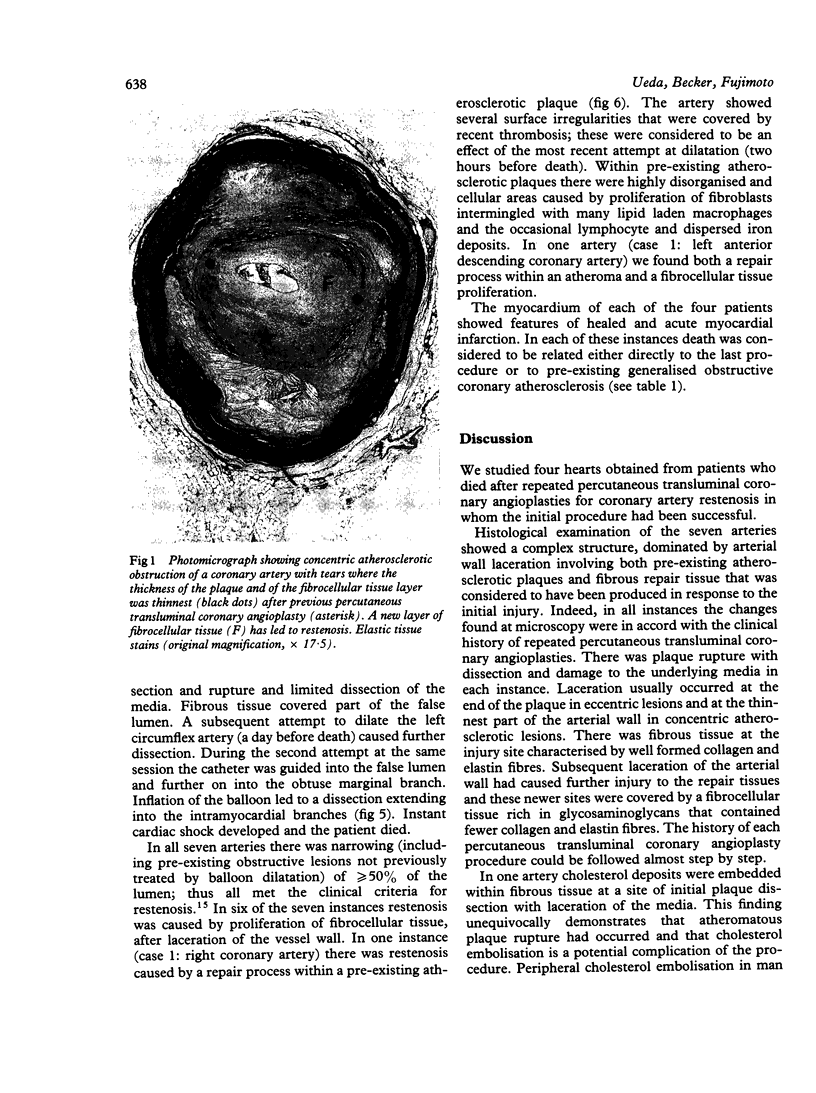
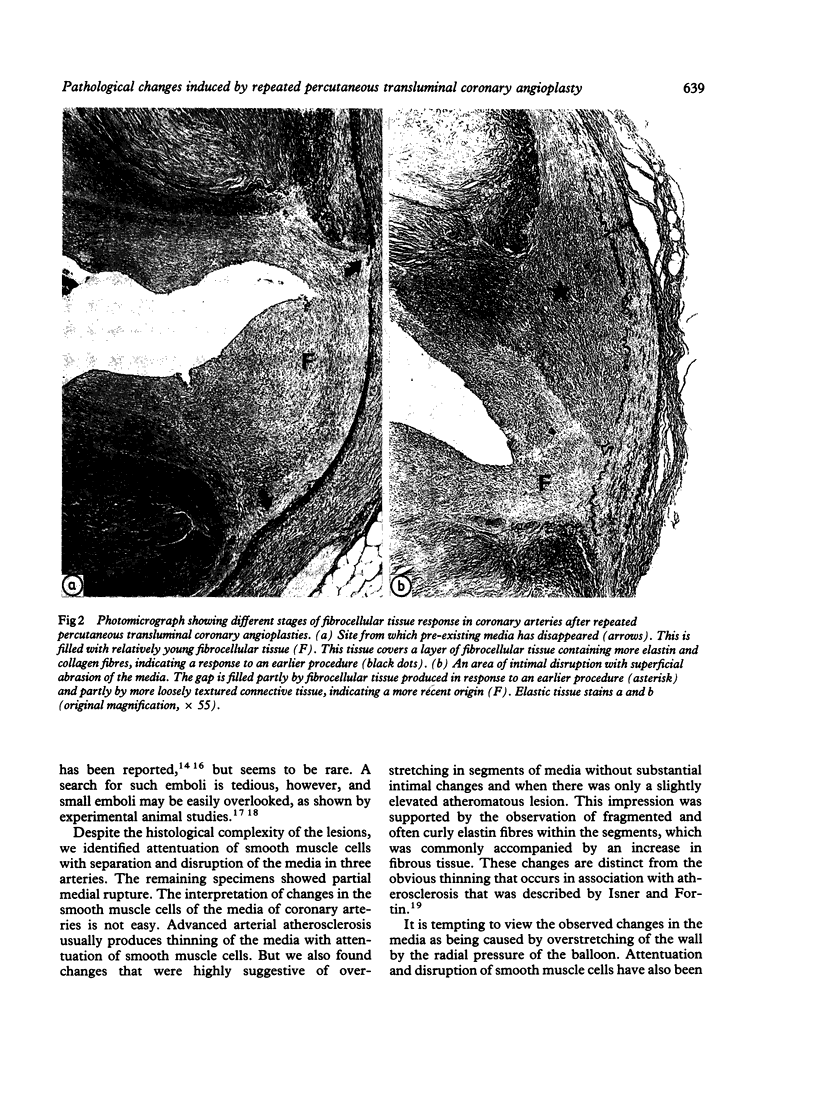
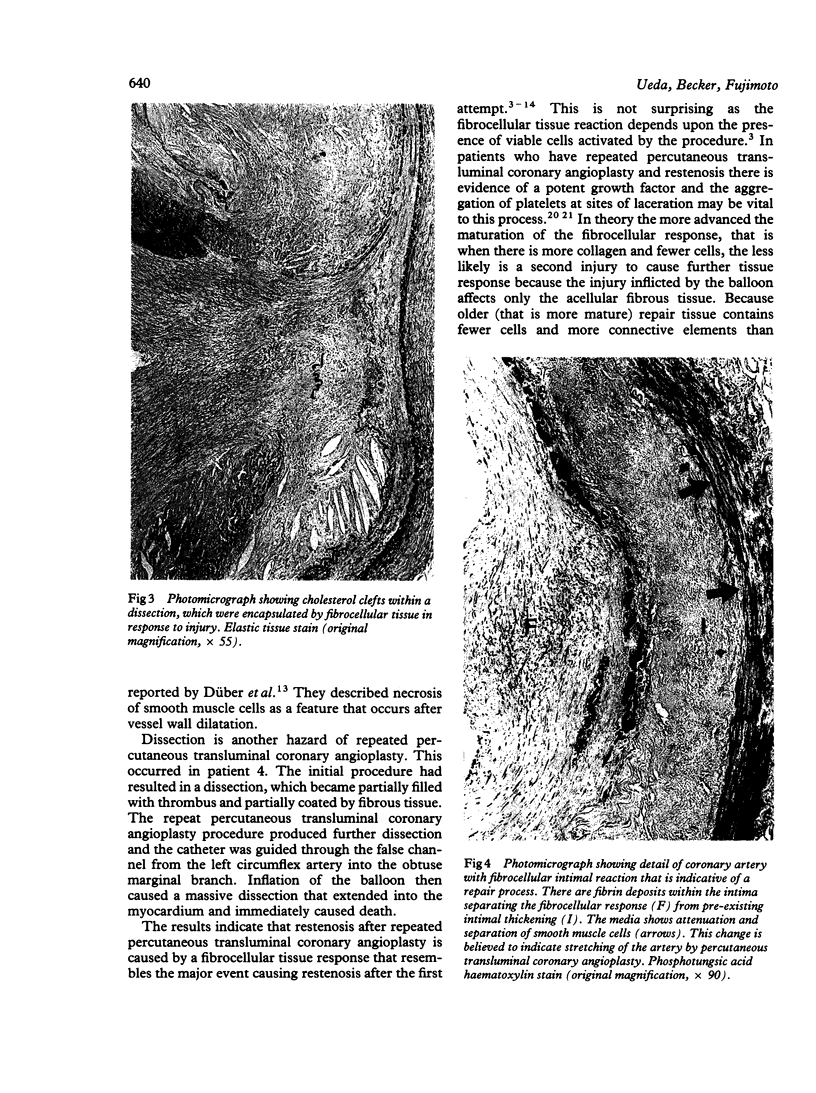
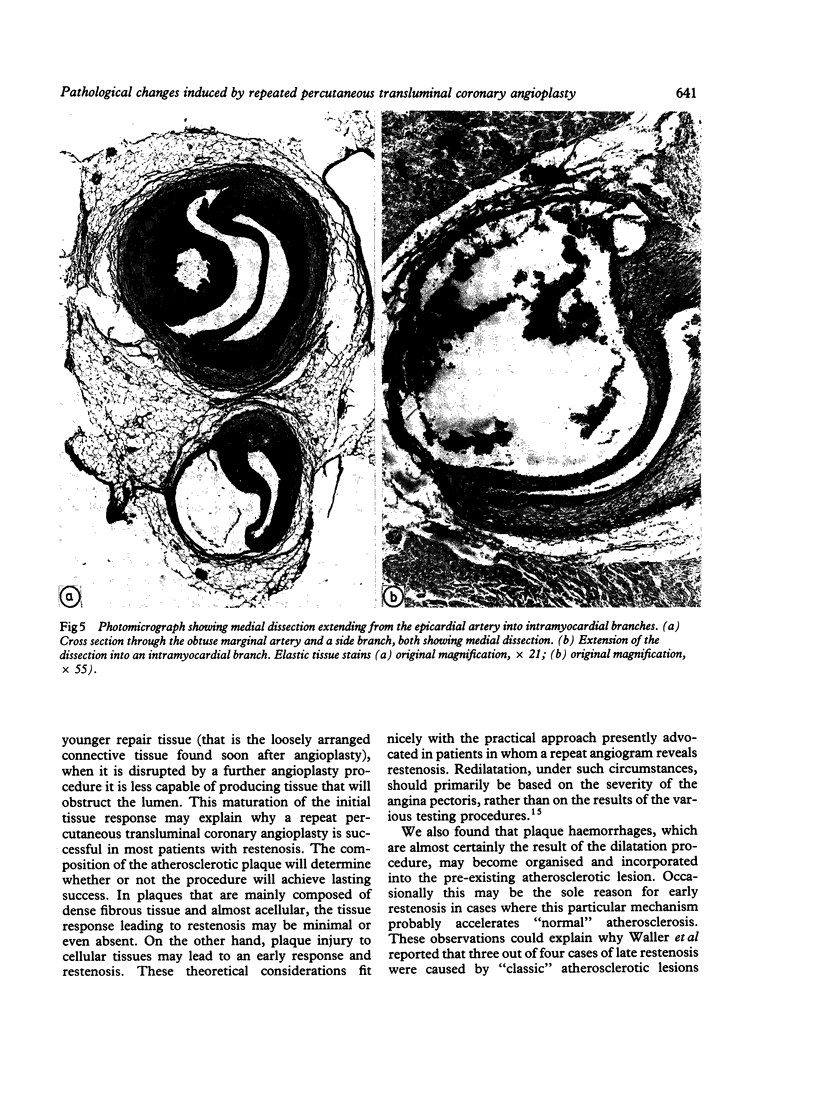
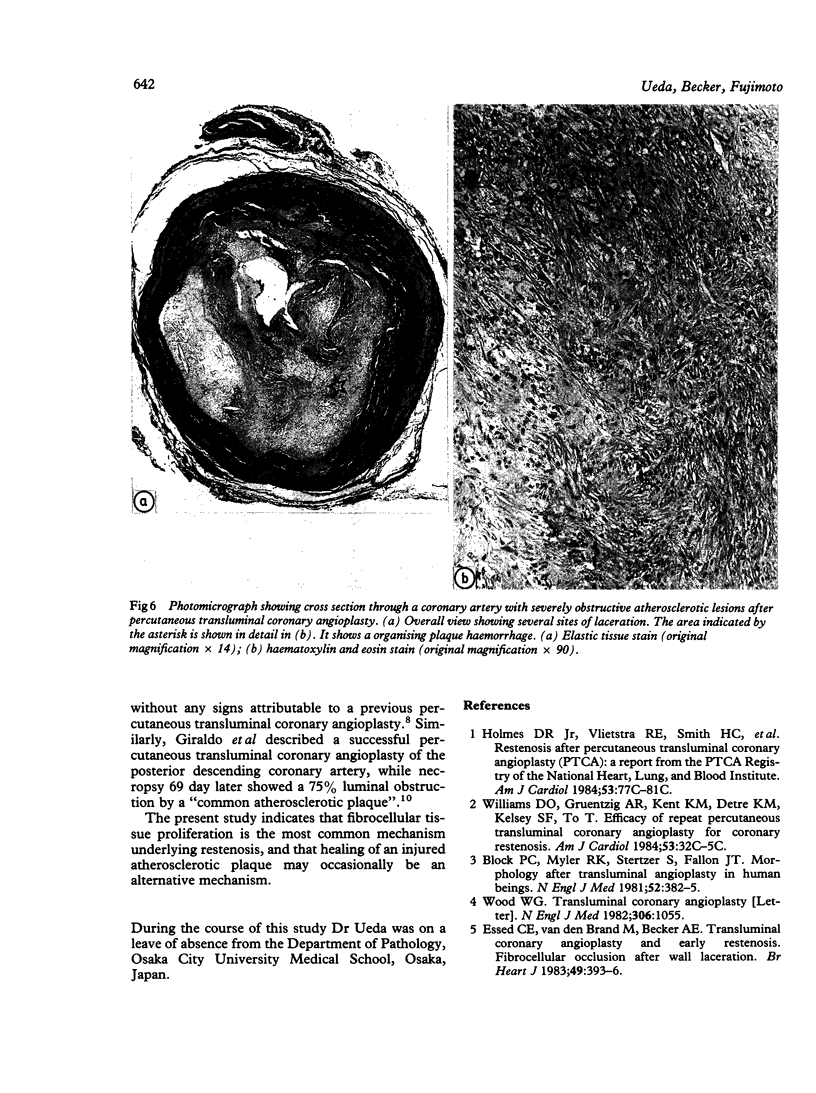
The histopathological appearances of seven coronary arteries obtained from four patients after repeated percutaneous transluminal coronary angioplasty were analysed. A complex picture was found; typically there were ruptured atherosclerotic plaques, plaque dissection, and a fibrous tissue response. The histopathological appearance of older and more recent fibrous lesions was different. Older lesions contained more collagen and elastin fibres, whereas recent ones had more loosely arranged connective tissue containing abundant glycosaminoglycan and readily identifiable cells. The fibrous tissues tended to be damaged at the sites of previous injury and where the vessel wall was thinnest. In five of the seven arteries there was evidence of a repeated fibrous response to injury with partial or total rupture of the original media. In one instance a repair response within a pre-existing atherosclerotic plaque had caused restenosis. The results indicate that restenosis after repeated percutaneous transluminal coronary angioplasty, like restenosis after a first procedure, is mainly the result of fibrocellular tissue response to injury of the wall tissues. Because older (that is more mature) repair tissue contains fewer cells and more connective elements than younger repair tissue (that is the loosely arranged connective tissue found soon after angioplasty), when it is disrupted by a further angioplasty procedure it is less capable of producing tissue that will obstruct the lumen. This may explain why in the majority of patients with restenosis repeated percutaneous transluminal coronary angioplasty is successful. The present study also showed that occasionally plaque haemorrhages may become organised and incorporated into the pre-existing atherosclerotic lesion.
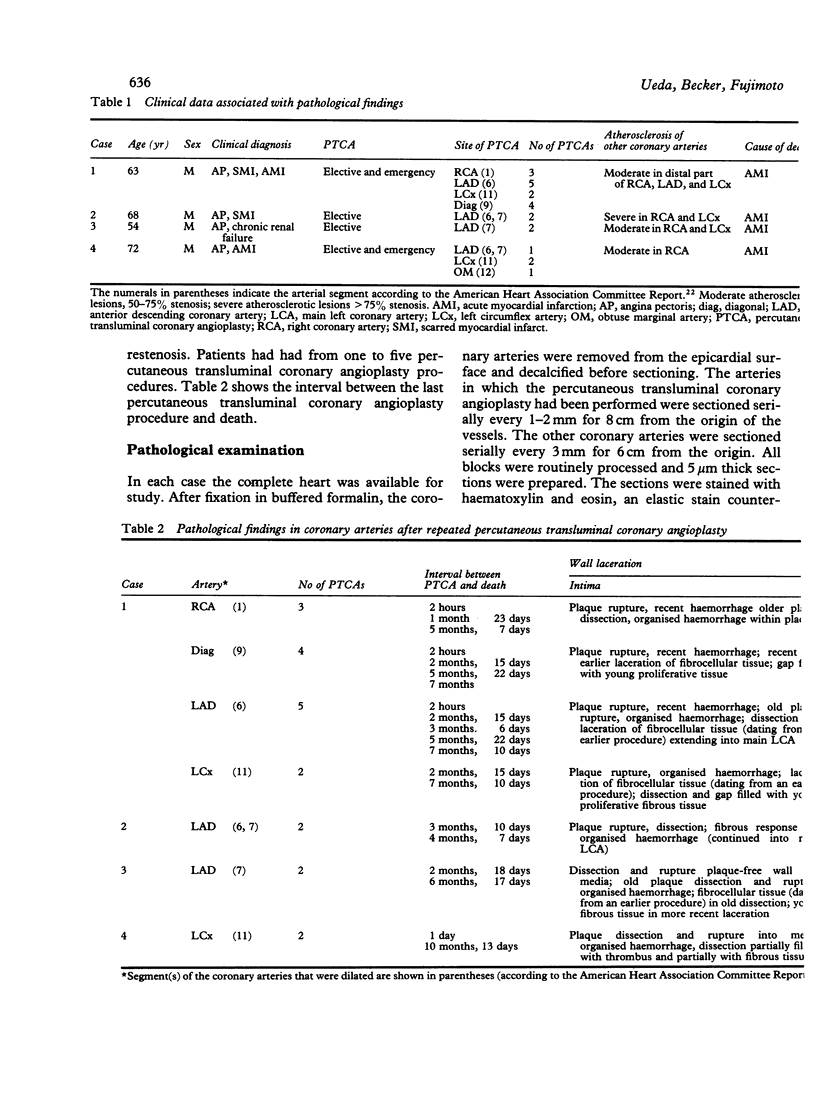
Full text
PDF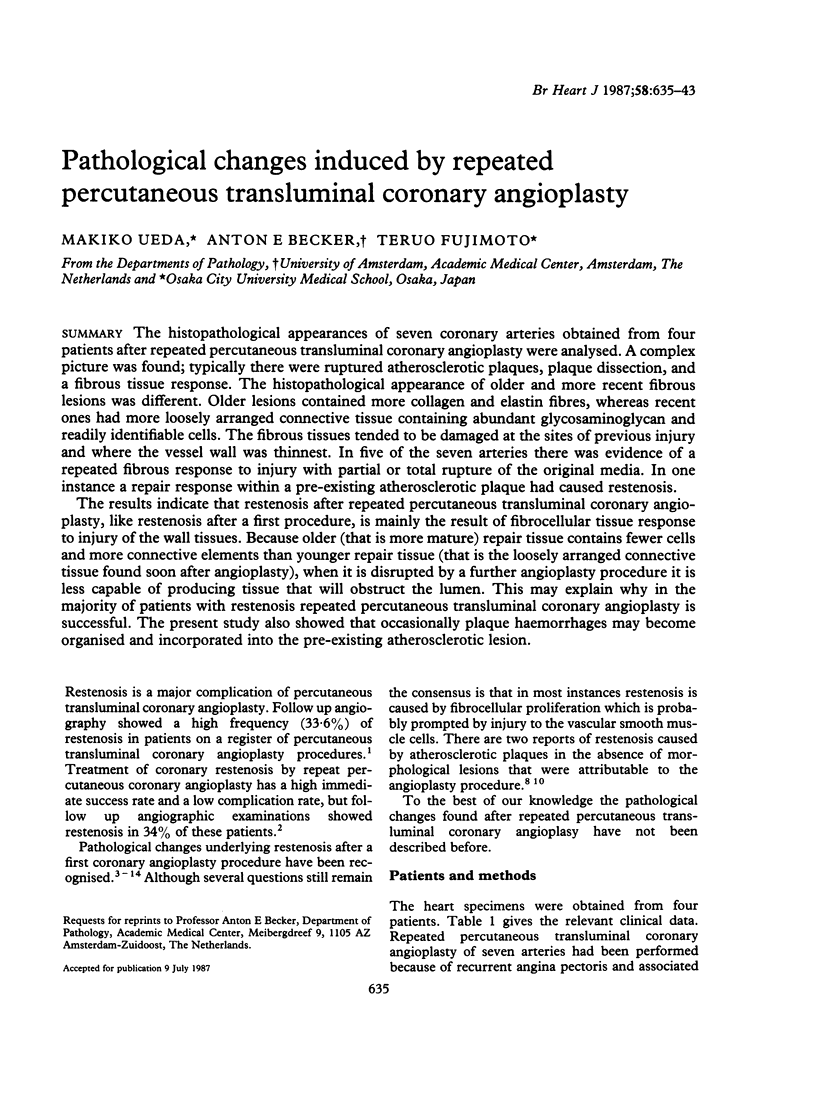
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Austen W. G., Edwards J. E., Frye R. L., Gensini G. G., Gott V. L., Griffith L. S., McGoon D. C., Murphy M. L., Roe B. B. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975 Apr;51(4 Suppl):5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- Austin G. E., Ratliff N. B., Hollman J., Tabei S., Phillips D. F. Intimal proliferation of smooth muscle cells as an explanation for recurrent coronary artery stenosis after percutaneous transluminal coronary angioplasty. J Am Coll Cardiol. 1985 Aug;6(2):369–375. doi: 10.1016/s0735-1097(85)80174-1. [DOI] [PubMed] [Google Scholar]
- Block P. C., Elmer D., Fallon J. T. Release of atherosclerotic debris after transluminal angioplasty. Circulation. 1982 May;65(5):950–952. doi: 10.1161/01.cir.65.5.950. [DOI] [PubMed] [Google Scholar]
- Block P. C., Myler R. K., Stertzer S., Fallon J. T. Morphology after transluminal angioplasty in human beings. N Engl J Med. 1981 Aug 13;305(7):382–385. doi: 10.1056/NEJM198108133050706. [DOI] [PubMed] [Google Scholar]
- Colavita P. G., Ideker R. E., Reimer K. A., Hackel D. B., Stack R. S. The spectrum of pathology associated with percutaneous transluminal coronary angioplasty during acute myocardial infarction. J Am Coll Cardiol. 1986 Oct;8(4):855–860. doi: 10.1016/s0735-1097(86)80427-2. [DOI] [PubMed] [Google Scholar]
- Crawford M. H., Petru M. A., Amon K. W., Sorensen S. G., Vance W. S. Comparative value of 2-dimensional echocardiography and radionuclide angiography for quantitating changes in left ventricular performance during exercise limited by angina pectoris. Am J Cardiol. 1984 Jan 1;53(1):42–46. doi: 10.1016/0002-9149(84)90681-7. [DOI] [PubMed] [Google Scholar]
- Düber C., Jungbluth A., Rumpelt H. J., Erbel R., Meyer J., Thoenes W. Morphology of the coronary arteries after combined thrombolysis and percutaneous transluminal coronary angioplasty for acute myocardial infarction. Am J Cardiol. 1986 Oct 1;58(9):698–703. doi: 10.1016/0002-9149(86)90340-1. [DOI] [PubMed] [Google Scholar]
- Essed C. E., Van den Brand M., Becker A. E. Transluminal coronary angioplasty and early restenosis. Fibrocellular occlusion after wall laceration. Br Heart J. 1983 Apr;49(4):393–396. doi: 10.1136/hrt.49.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraldo A. A., Esposo O. M., Meis J. M. Intimal hyperplasia as a cause of restenosis after percutaneous transluminal coronary angioplasty. Arch Pathol Lab Med. 1985 Feb;109(2):173–175. [PubMed] [Google Scholar]
- Isner J. M., Fortin R. V. Frequency in nonangioplasty patients of morphologic findings reported in coronary arteries treated with transluminal angioplasty. Am J Cardiol. 1983 Mar 1;51(5):689–693. doi: 10.1016/s0002-9149(83)80116-7. [DOI] [PubMed] [Google Scholar]
- MacDonald R. G., Feldman R. L., Conti C. R., Pepine C. J. Thromboembolic complications of coronary angioplasty. Am J Cardiol. 1984 Oct 1;54(7):916–917. doi: 10.1016/s0002-9149(84)80234-9. [DOI] [PubMed] [Google Scholar]
- Mizuno K., Kurita A., Imazeki N. Pathological findings after percutaneous transluminal coronary angioplasty. Br Heart J. 1984 Nov;52(5):588–590. doi: 10.1136/hrt.52.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffitz J. E., Rose T. E., Oaks J. B., Roberts W. C. Coronary arterial rupture during coronary angioplasty. Am J Cardiol. 1983 Mar 1;51(5):902–904. doi: 10.1016/s0002-9149(83)80154-4. [DOI] [PubMed] [Google Scholar]
- Salerno D. M., Granrud G., Sharkey P., Asinger R., Hodges M. A controlled trial of propafenone for treatment of frequent and repetitive ventricular premature complexes. Am J Cardiol. 1984 Jan 1;53(1):77–83. doi: 10.1016/0002-9149(84)90687-8. [DOI] [PubMed] [Google Scholar]
- Sanborn T. A., Faxon D. P., Waugh D., Small D. M., Haudenschild C., Gottsman S. B., Ryan T. J. Transluminal angioplasty in experimental atherosclerosis. Analysis for embolization using an in vivo perfusion system. Circulation. 1982 Nov;66(5):917–922. [PubMed] [Google Scholar]
- Schneider J., Grüntzig A. Percutaneous transluminal coronary angioplasty: morphological findings in 3 patients. Pathol Res Pract. 1985 Oct;180(4):348–352. doi: 10.1016/S0344-0338(85)80104-7. [DOI] [PubMed] [Google Scholar]
- Soward A. L., Essed C. E., Serruys P. W. Coronary arterial findings after accidental death immediately after successful percutaneous transluminal coronary angioplasty. Am J Cardiol. 1985 Nov 1;56(12):794–795. doi: 10.1016/0002-9149(85)91141-5. [DOI] [PubMed] [Google Scholar]
- Steele P. M., Chesebro J. H., Stanson A. W., Holmes D. R., Jr, Dewanjee M. K., Badimon L., Fuster V. Balloon angioplasty. Natural history of the pathophysiological response to injury in a pig model. Circ Res. 1985 Jul;57(1):105–112. doi: 10.1161/01.res.57.1.105. [DOI] [PubMed] [Google Scholar]
- Wijns W., Serruys P. W., Reiber J. H., de Feyter P. J., van den Brand M., Simoons M. L., Hugenholtz P. G. Early detection of restenosis after successful percutaneous transluminal coronary angioplasty by exercise-redistribution thallium scintigraphy. Am J Cardiol. 1985 Feb 1;55(4):357–361. doi: 10.1016/0002-9149(85)90375-3. [DOI] [PubMed] [Google Scholar]
- Wood W. G. Transluminal coronary angioplasty. N Engl J Med. 1982 Apr 29;306(17):1055–1055. doi: 10.1056/NEJM198204293061717. [DOI] [PubMed] [Google Scholar]