Abstract
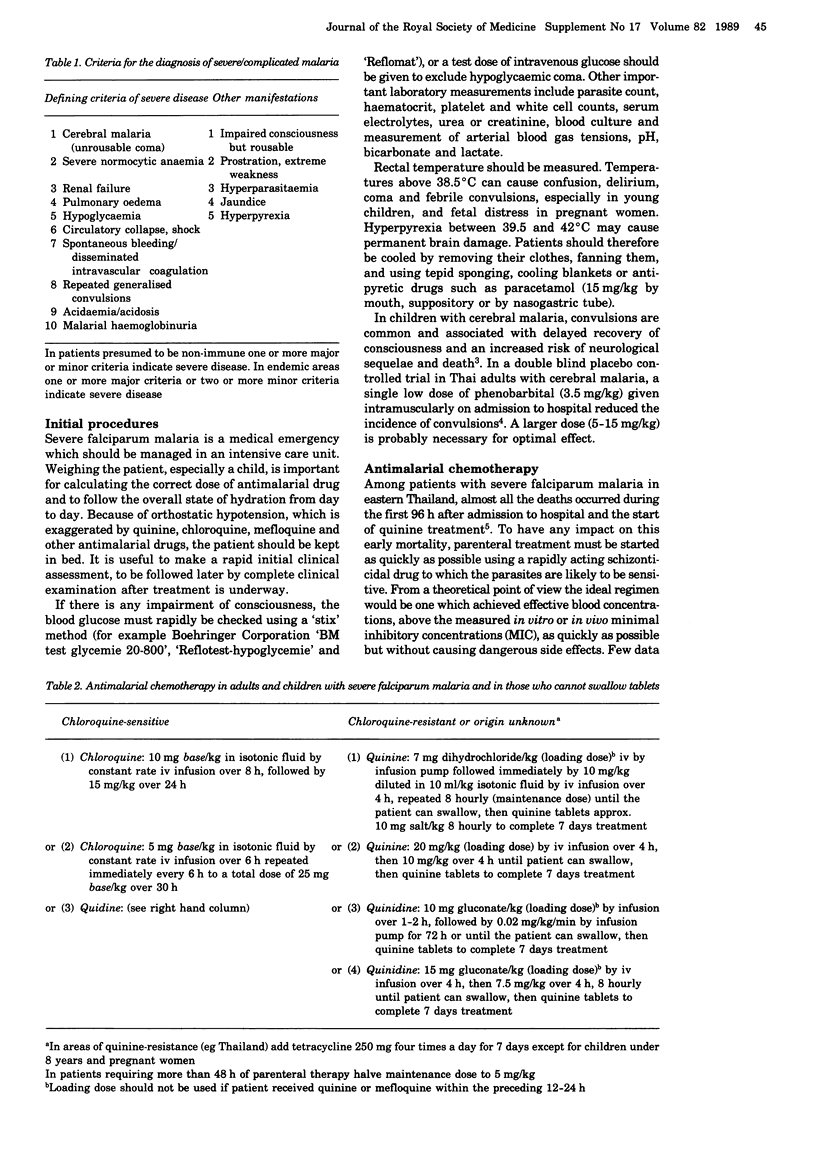
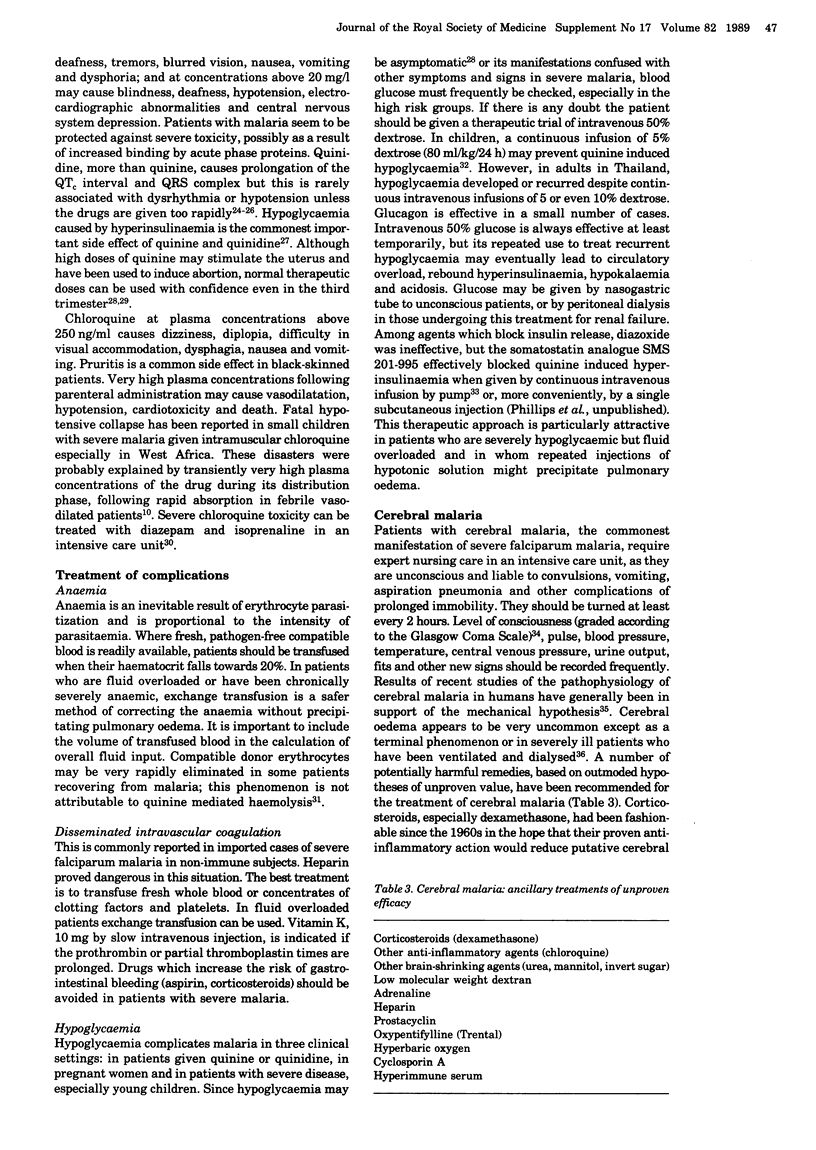
In the treatment of severe Plasmodium falciparum infection antimalarial drugs should, ideally, be given by controlled rate intravenous infusion until the patient is able to swallow tablets. In cases where infection has been acquired in a chloroquine resistant area, and where it has broken through chloroquine prophylaxis or where the geographical origin or species are uncertain, quinine is the treatment of choice. When access to parenteral quinine is likely to be delayed, parenteral quinidine is an effective alternative. A loading dose of quinine is recommended in order to achieve therapeutic plasma concentrations as quickly as possible. In the case of chloroquine sensitive P. falciparum infection, chloroquine, which can be given safely by slow intravenous infusion, may be more rapidly effective and has fewer toxic effects than quinine. There is limited experience with parenteral administration of pyrimethamine sulphonamide combinations such as Fansidar, and resistance to these drugs has developed in South East Asia and elsewhere. Mefloquine and halofantrine cannot be given parenterally. Qinghaosu derivatives are not readily available and have not been adequately tested outside China. Supportive treatment includes the prevention or early detection and treatment of complications, strict attention to fluid balance, provision of adequate nursing for unconscious patients and avoidance of harmful ancillary treatments. Anaemia is inevitable and out of proportion to detectable parasitaemia. Hypotension and shock ('algid malaria') are often attributable to secondary gram-negative septicaemia requiring appropriate antimicrobial therapy and haemodynamic resuscitation. Many patients with severe falciparum malaria are hypovolaemic on admission to hospital and require cautious fluid replacement. Failure to rehydrate these patients may lead to circulatory collapse, lactic acidosis, renal failure and severe hyponatraemia.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bone R. C., Fisher C. J., Jr, Clemmer T. P., Slotman G. J., Metz C. A., Balk R. A. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N Engl J Med. 1987 Sep 10;317(11):653–658. doi: 10.1056/NEJM198709103171101. [DOI] [PubMed] [Google Scholar]
- Brooks M. H., Malloy J. P., Bartelloni P. J., Tigertt W. D., Sheehy T. W., Barry K. G. Pathophysiology of acute falciparum malaria. I. Correlation of clinical and biochemical abnormalities. Am J Med. 1967 Nov;43(5):735–744. doi: 10.1016/0002-9343(67)90115-5. [DOI] [PubMed] [Google Scholar]
- Bruce-Chwatt L. J. Unde venis viator et quo vadis? Ann Trop Med Parasitol. 1987 Oct;81(5):471–486. doi: 10.1080/00034983.1987.11812150. [DOI] [PubMed] [Google Scholar]
- Chanthavanich P., Looareesuwan S., White N. J., Warrell D. A., Warrell M. J., DiGiovanni J. H., von Bredow J. Intragastric mefloquine is absorbed rapidly in patients with cerebral malaria. Am J Trop Med Hyg. 1985 Nov;34(6):1028–1036. doi: 10.4269/ajtmh.1985.34.1028. [DOI] [PubMed] [Google Scholar]
- Chongsuphajaisiddhi T., Dauruag V., Patcharakessakul V., Kittivattanakul V., Dulyasakdi B., Ridthimat W. Treatment of falciparum malaria with intra muscular quinine in a rural area of Thailand. Southeast Asian J Trop Med Public Health. 1983 Jun;14(2):220–222. [PubMed] [Google Scholar]
- Chongsuphajaisiddhi T., Kasemsuth R., Tejavanija S., Harinasuta T. Changes in blood volume in Falciparum malaria. Southeast Asian J Trop Med Public Health. 1971 Sep;2(3):344–350. [PubMed] [Google Scholar]
- Chongsuphajaisiddhi T., Sabcharoen A., Attanath P. In vivo and in vitro sensitivity of Falciparum malaria to quinine in Thai children. Ann Trop Paediatr. 1981 Mar;1(1):21–26. doi: 10.1080/02724936.1981.11748054. [DOI] [PubMed] [Google Scholar]
- Cooper B. High-dose dexamethasone in malaria. J Infect Dis. 1989 Apr;159(4):803–804. doi: 10.1093/infdis/159.4.803. [DOI] [PubMed] [Google Scholar]
- Davis T. M., White N. J., Looareesuwan S., Silamut K., Warrell D. A. Quinine pharmacokinetics in cerebral malaria: predicted plasma concentrations after rapid intravenous loading using a two-compartment model. Trans R Soc Trop Med Hyg. 1988;82(4):542–547. doi: 10.1016/0035-9203(88)90498-1. [DOI] [PubMed] [Google Scholar]
- Edwards G., Davies A. J., Phillips R. E., Looareesuwan S., Karbwang J., White N. J., Warrell D. A. Plasma concentrations and toxicity of chloroquine after slow intravenous infusion in patients with falciparum malaria. Ann Trop Med Parasitol. 1987 Apr;81(2):79–84. doi: 10.1080/00034983.1987.11812098. [DOI] [PubMed] [Google Scholar]
- Edwards G., Looareesuwan S., Davies A. J., Wattanagoon Y., Phillips R. E., Warrell D. A. Pharmacokinetics of chloroquine in Thais: plasma and red-cell concentrations following an intravenous infusion to healthy subjects and patients with Plasmodium vivax malaria. Br J Clin Pharmacol. 1988 Apr;25(4):477–485. doi: 10.1111/j.1365-2125.1988.tb03332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg A. E., Nguyen-Dinh P., Davachi F., Yemvula B., Malanda N., Nzeza M., Williams S. B., de Zwart J. F., Nzeza M. Intravenous quinine therapy of hospitalized children with Plasmodium falciparum malaria in Kinshasa, Zaire. Am J Trop Med Hyg. 1989 Apr;40(4):360–364. doi: 10.4269/ajtmh.1989.40.360. [DOI] [PubMed] [Google Scholar]
- Harinasuta T., Viravan C., Buranasin P. Parenteral Fansidar in falciparum malaria. Trans R Soc Trop Med Hyg. 1988;82(5):694–694. doi: 10.1016/0035-9203(88)90203-9. [DOI] [PubMed] [Google Scholar]
- Hoffman S. L., Rustama D., Punjabi N. H., Surampaet B., Sanjaya B., Dimpudus A. J., McKee K. T., Jr, Paleologo F. P., Campbell J. R., Marwoto H. High-dose dexamethasone in quinine-treated patients with cerebral malaria: a double-blind, placebo-controlled trial. J Infect Dis. 1988 Aug;158(2):325–331. doi: 10.1093/infdis/158.2.325. [DOI] [PubMed] [Google Scholar]
- Horstmann R. D., Ehrich J. H., Beck J., Dietrich M. Letale Komplikationen der Malaria tropica bei Nichtimmunen. Eine retrospektive klinisch-pathologische Analyse von 25 Fällen. Dtsch Med Wochenschr. 1985 Oct 25;110(43):1651–1656. doi: 10.1055/s-2008-1069063. [DOI] [PubMed] [Google Scholar]
- Lataste P., Soubiran G., Nlend A., Le Bras M., Roue R., Wone C., Ragnaud J. C., Buil A., Briand M. C., Ripert C. Intérêt de l'exsanguinotransfusion dans le traitement du paludisme grave (à propos de 5 observations). Bull Soc Pathol Exot Filiales. 1987;80(3 Pt 2):561–568. [PubMed] [Google Scholar]
- Li G. Q., Guo X. B., Jin R., Wang Z. C., Jian H. X., Li Z. Y. Clinical studies on treatment of cerebral malaria with qinghaosu and its derivatives. J Tradit Chin Med. 1982 Jun;2(2):125–130. [PubMed] [Google Scholar]
- Looareesuwan S., Merry A. H., Phillips R. E., Pleehachinda R., Wattanagoon Y., Ho M., Charoenlarp P., Warrell D. A., Weatherall D. J. Reduced erythrocyte survival following clearance of malarial parasitaemia in Thai patients. Br J Haematol. 1987 Dec;67(4):473–478. doi: 10.1111/j.1365-2141.1987.tb06171.x. [DOI] [PubMed] [Google Scholar]
- Looareesuwan S., Phillips R. E., White N. J., Kietinun S., Karbwang J., Rackow C., Turner R. C., Warrell D. A. Quinine and severe falciparum malaria in late pregnancy. Lancet. 1985 Jul 6;2(8445):4–8. doi: 10.1016/s0140-6736(85)90056-x. [DOI] [PubMed] [Google Scholar]
- Malloy J. P., Brooks M. H., Barry K. G. Pathophysiology of acute falciparum malaria. II. Fluid compartmentalization. Am J Med. 1967 Nov;43(5):745–750. doi: 10.1016/0002-9343(67)90116-7. [DOI] [PubMed] [Google Scholar]
- Miller K. D., Greenberg A. E., Campbell C. C. Treatment of severe malaria in the United States with a continuous infusion of quinidine gluconate and exchange transfusion. N Engl J Med. 1989 Jul 13;321(2):65–70. doi: 10.1056/NEJM198907133210201. [DOI] [PubMed] [Google Scholar]
- Molyneux M. E., Taylor T. E., Wirima J. J., Borgstein A. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. Q J Med. 1989 May;71(265):441–459. [PubMed] [Google Scholar]
- Phillips R. E., Looareesuwan S., White N. J., Silamut K., Kietinun S., Warrell D. A. Quinine pharmacokinetics and toxicity in pregnant and lactating women with falciparum malaria. Br J Clin Pharmacol. 1986 Jun;21(6):677–683. doi: 10.1111/j.1365-2125.1986.tb05233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips R. E., Warrell D. A., Edwards G., Galagedera Y., Theakston R. D., Abeysekera D. T., Dissanayaka P. Divided dose intramuscular regimen and single dose subcutaneous regimen for chloroquine: plasma concentrations and toxicity in patients with malaria. Br Med J (Clin Res Ed) 1986 Jul 5;293(6538):13–16. doi: 10.1136/bmj.293.6538.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips R. E., Warrell D. A., Looareesuwan S., Turner R. C., Bloom S. R., Quantrill D., Moore A. R. Effectiveness of SMS 201-995, a synthetic, long-acting somatostatin analogue, in treatment of quinine-induced hyperinsulinaemia. Lancet. 1986 Mar 29;1(8483):713–716. doi: 10.1016/s0140-6736(86)91103-7. [DOI] [PubMed] [Google Scholar]
- Phillips R. E., Warrell D. A., White N. J., Looareesuwan S., Karbwang J. Intravenous quinidine for the treatment of severe falciparum malaria. Clinical and pharmacokinetic studies. N Engl J Med. 1985 May 16;312(20):1273–1278. doi: 10.1056/NEJM198505163122001. [DOI] [PubMed] [Google Scholar]
- Poungvarin N., Bhoopat W., Viriyavejakul A., Rodprasert P., Buranasiri P., Sukondhabhant S., Hensley M. J., Strom B. L. Effects of dexamethasone in primary supratentorial intracerebral hemorrhage. N Engl J Med. 1987 May 14;316(20):1229–1233. doi: 10.1056/NEJM198705143162001. [DOI] [PubMed] [Google Scholar]
- Rees P. Dexamethasone deleterious in cerebral malaria. Br Med J (Clin Res Ed) 1982 Nov 6;285(6351):1357–1357. doi: 10.1136/bmj.285.6351.1357. [DOI] [PubMed] [Google Scholar]
- Riou B., Barriot P., Rimailho A., Baud F. J. Treatment of severe chloroquine poisoning. N Engl J Med. 1988 Jan 7;318(1):1–6. doi: 10.1056/NEJM198801073180101. [DOI] [PubMed] [Google Scholar]
- Shann F., Stace J., Edstein M. Pharmacokinetics of quinine in children. J Pediatr. 1985 Mar;106(3):506–510. doi: 10.1016/s0022-3476(85)80692-2. [DOI] [PubMed] [Google Scholar]
- Sprung C. L., Caralis P. V., Marcial E. H., Pierce M., Gelbard M. A., Long W. M., Duncan R. C., Tendler M. D., Karpf M. The effects of high-dose corticosteroids in patients with septic shock. A prospective, controlled study. N Engl J Med. 1984 Nov 1;311(18):1137–1143. doi: 10.1056/NEJM198411013111801. [DOI] [PubMed] [Google Scholar]
- Stacpoole P. W., Lorenz A. C., Thomas R. G., Harman E. M. Dichloroacetate in the treatment of lactic acidosis. Ann Intern Med. 1988 Jan;108(1):58–63. doi: 10.7326/0003-4819-108-1-58. [DOI] [PubMed] [Google Scholar]
- Taylor T. E., Molyneux M. E., Wirima J. J., Fletcher K. A., Morris K. Blood glucose levels in Malawian children before and during the administration of intravenous quinine for severe falciparum malaria. N Engl J Med. 1988 Oct 20;319(16):1040–1047. doi: 10.1056/NEJM198810203191602. [DOI] [PubMed] [Google Scholar]
- Teasdale G., Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974 Jul 13;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Warrell D. A., Looareesuwan S., Warrell M. J., Kasemsarn P., Intaraprasert R., Bunnag D., Harinasuta T. Dexamethasone proves deleterious in cerebral malaria. A double-blind trial in 100 comatose patients. N Engl J Med. 1982 Feb 11;306(6):313–319. doi: 10.1056/NEJM198202113060601. [DOI] [PubMed] [Google Scholar]
- Warrell D. A. Pathophysiology of severe falciparum malaria in man. Parasitology. 1987;94 (Suppl):S53–S76. doi: 10.1017/s0031182000085826. [DOI] [PubMed] [Google Scholar]
- Wattanagoon Y., Phillips R. E., Warrell D. A., Silamut K., Looareesuwan S., Nagachinta B., Back D. J. Intramuscular loading dose of quinine for falciparum malaria: pharmacokinetics and toxicity. Br Med J (Clin Res Ed) 1986 Jul 5;293(6538):11–13. doi: 10.1136/bmj.293.6538.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston M. J., Jackman N., Rudge C., Bowles J., Brady C., Bielawska C., O'Grady J. Prostacyclin in Falciparum malaria. Lancet. 1982 Sep 11;2(8298):609–609. doi: 10.1016/s0140-6736(82)90684-5. [DOI] [PubMed] [Google Scholar]
- White N. J., Chanthavanich P., Krishna S., Bunch C., Silamut K. Quinine disposition kinetics. Br J Clin Pharmacol. 1983 Oct;16(4):399–403. doi: 10.1111/j.1365-2125.1983.tb02184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White N. J., Looareesuwan S., Phillips R. E., Chanthavanich P., Warrell D. A. Single dose phenobarbitone prevents convulsions in cerebral malaria. Lancet. 1988 Jul 9;2(8602):64–66. doi: 10.1016/s0140-6736(88)90002-5. [DOI] [PubMed] [Google Scholar]
- White N. J., Looareesuwan S., Warrell D. A. Quinine and quinidine: a comparison of EKG effects during the treatment of malaria. J Cardiovasc Pharmacol. 1983 Mar-Apr;5(2):173–175. doi: 10.1097/00005344-198303000-00001. [DOI] [PubMed] [Google Scholar]
- White N. J., Looareesuwan S., Warrell D. A., Warrell M. J., Chanthavanich P., Bunnag D., Harinasuta T. Quinine loading dose in cerebral malaria. Am J Trop Med Hyg. 1983 Jan;32(1):1–5. doi: 10.4269/ajtmh.1983.32.1. [DOI] [PubMed] [Google Scholar]
- White N. J., Miller K. D., Churchill F. C., Berry C., Brown J., Williams S. B., Greenwood B. M. Chloroquine treatment of severe malaria in children. Pharmacokinetics, toxicity, and new dosage recommendations. N Engl J Med. 1988 Dec 8;319(23):1493–1500. doi: 10.1056/NEJM198812083192301. [DOI] [PubMed] [Google Scholar]
- White N. J., Warrell D. A., Chanthavanich P., Looareesuwan S., Warrell M. J., Krishna S., Williamson D. H., Turner R. C. Severe hypoglycemia and hyperinsulinemia in falciparum malaria. N Engl J Med. 1983 Jul 14;309(2):61–66. doi: 10.1056/NEJM198307143090201. [DOI] [PubMed] [Google Scholar]
- White N. J., Watt G., Bergqvist Y., Njelesani E. K. Parenteral chloroquine for treating falciparum malaria. J Infect Dis. 1987 Feb;155(2):192–201. doi: 10.1093/infdis/155.2.192. [DOI] [PubMed] [Google Scholar]


