Abstract
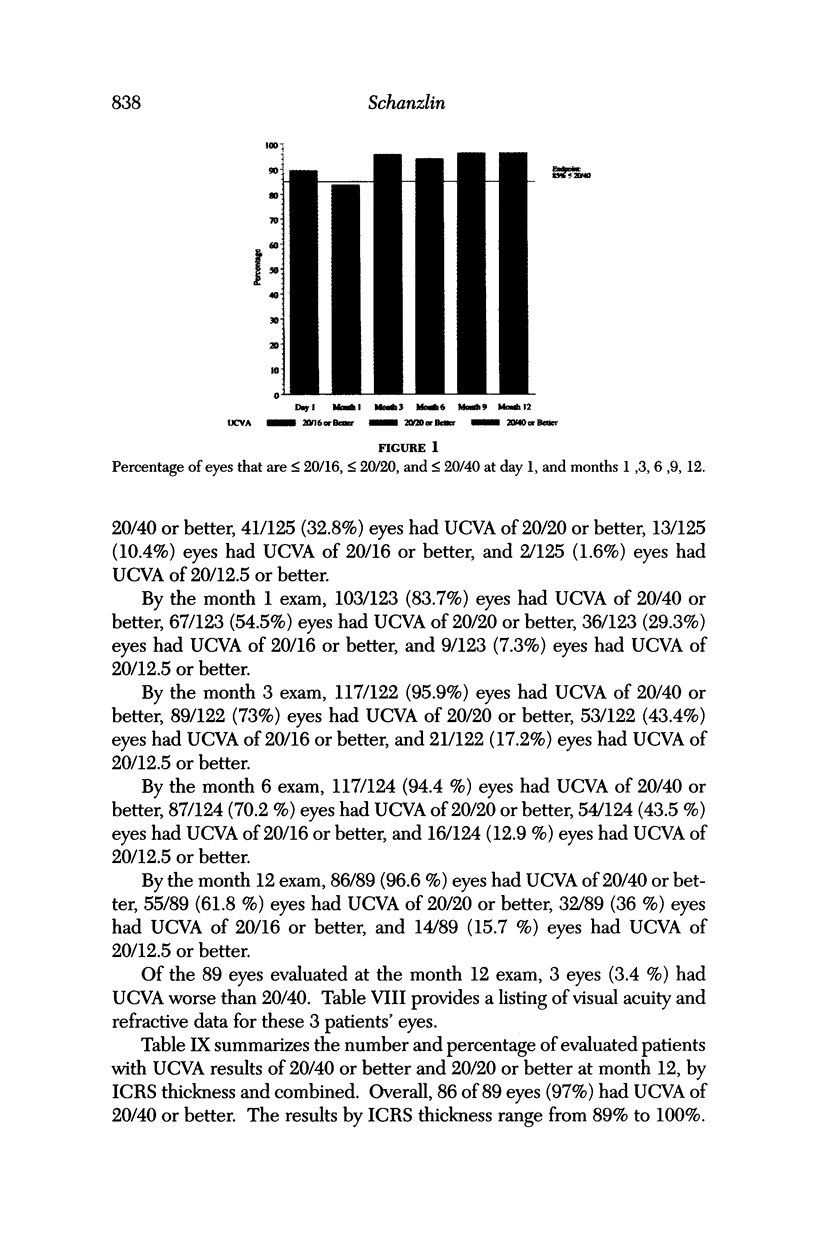
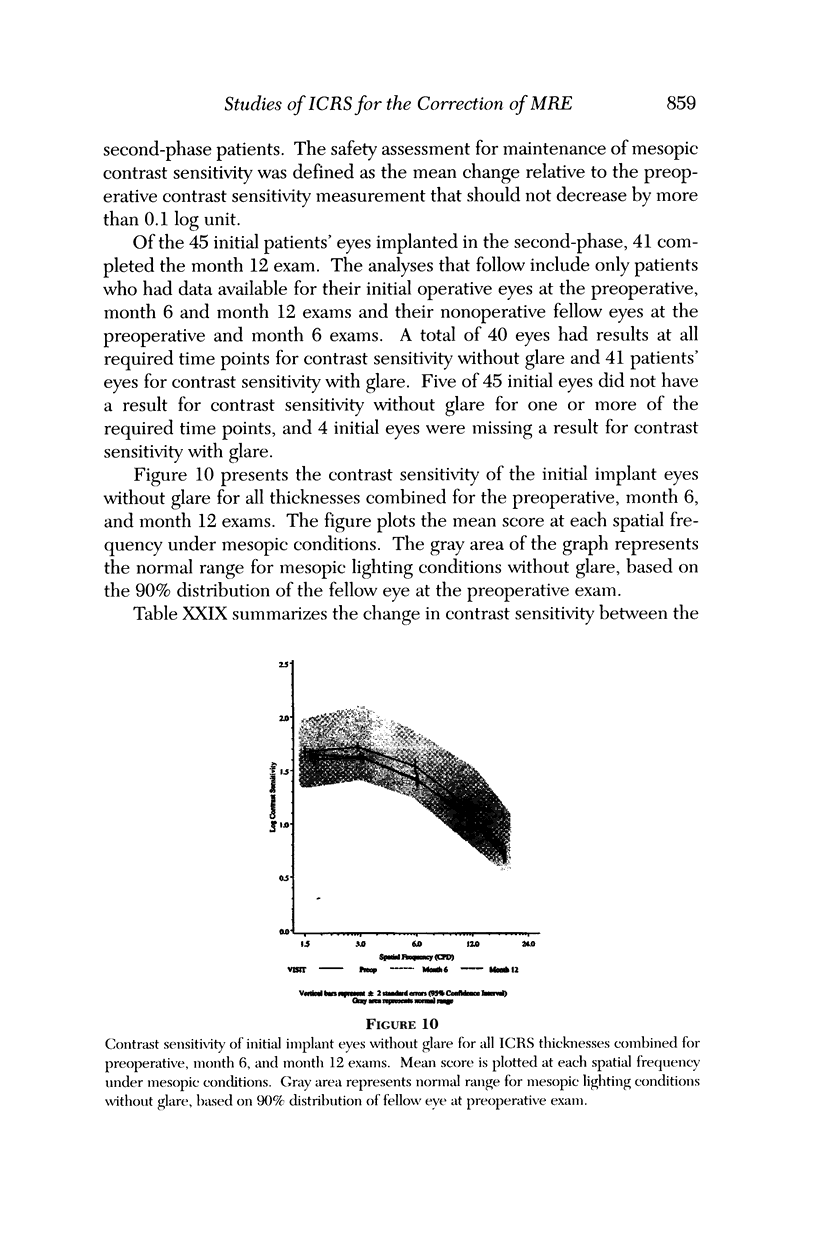
PURPOSE: Intrastromal corneal ring segments (ICRS) were investigated for safety and reliability in the correction of low to moderate myopic refractive errors. METHODS: Initially, 74 patients with spherical equivalent refractive errors between -1.00 and -4.25 diopters (D) received the ICRS in 1 eye. After 6 months, 51 of these patients received the ICRS in the contralateral eye. The total number of eyes investigated was 125. The outcome measures were uncorrected and best-corrected visual acuity, predictability and stability of the refraction, refractive astigmatism, contrast sensitivity, and endothelial cell morphology. RESULTS: The 89 eyes with 12-month follow-up showed significant improvement with uncorrected visual acuities of 20/16 or better in 37%, 20/20 or better in 62%, and 20/40 or better in 97%. Cycloplegic refraction spherical equivalents showed that 68% of the eyes were within +/- 0.50 D and 90% within +/- 1.00 D of the intended correction. Refractive stability was present by 3 months after the surgery. Only 1 patients had a loss greater than 2 lines or 10 letters of best spectacle-corrected visual acuity, but the patient's acuity was 20/20. Refractive cylinder, contrast sensitivity, and endothelial cell morphology were not adversely affected. The ICRS was removed from the eyes of 6 patients. Three removals were prompted by glare and double images occurring at night; 3 were for nonmedical reasons. All patients returned to within +/- 1.00 D of their preoperative refractive spherical equivalent, and no patients lost more than 1 line of best corrected visual acuity by 3 months after ICRS removal. CONCLUSION: The ICRS safely and reliably corrects myopic refractive errors between -1.00 and -4.50 D.
Full text
PDF
















Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Assil K. K., Barrett A. M., Fouraker B. D., Schanzlin D. J. One-year results of the intrastromal corneal ring in nonfunctional human eyes. Intrastromal Corneal Ring Study Group. Arch Ophthalmol. 1995 Feb;113(2):159–167. doi: 10.1001/archopht.1995.01100020041026. [DOI] [PubMed] [Google Scholar]
- Assil K. K., Kassoff J., Schanzlin D. J., Quantock A. J. A combined incision technique of radial keratotomy. A comparison to centripetal and centrifugal incision techniques in human donor eyes. Ophthalmology. 1994 Apr;101(4):746–754. doi: 10.1016/s0161-6420(94)31271-1. [DOI] [PubMed] [Google Scholar]
- Assil K. K., Quantock A. J., Barrett A. M., Schanzlin D. J. Corneal iron lines associated with the intrastromal corneal ring. Am J Ophthalmol. 1993 Sep 15;116(3):350–356. doi: 10.1016/s0002-9394(14)71353-4. [DOI] [PubMed] [Google Scholar]
- Binder P. S., Baumgartner S. D., Fogle J. A. Histopathology of a case of epikeratophakia (aphakic epikeratoplasty). Arch Ophthalmol. 1985 Sep;103(9):1357–1363. doi: 10.1001/archopht.1985.01050090109044. [DOI] [PubMed] [Google Scholar]
- Binder P. S., Zavala E. Y., Baumgartner S. D., Nayak S. K. Combined morphologic effects of cryolathing and lyophilization on epikeratoplasty lenticules. Arch Ophthalmol. 1986 May;104(5):671–679. doi: 10.1001/archopht.1986.01050170061022. [DOI] [PubMed] [Google Scholar]
- Binder P. S., Zavala E. Y. Why do some epikeratoplasties fail? Arch Ophthalmol. 1987 Jan;105(1):63–69. doi: 10.1001/archopht.1987.01060010069033. [DOI] [PubMed] [Google Scholar]
- Bourne W. M., Nelson L. R., Hodge D. O. Central corneal endothelial cell changes over a ten-year period. Invest Ophthalmol Vis Sci. 1997 Mar;38(3):779–782. [PubMed] [Google Scholar]
- Brint S. F., Ostrick D. M., Fisher C., Slade S. G., Maloney R. K., Epstein R., Stulting R. D., Thompson K. P. Six-month results of the multicenter phase I study of excimer laser myopic keratomileusis. J Cataract Refract Surg. 1994 Nov;20(6):610–615. doi: 10.1016/s0886-3350(13)80648-7. [DOI] [PubMed] [Google Scholar]
- Burris T. E., Ayer C. T., Evensen D. A., Davenport J. M. Effects of intrastromal corneal ring size and thickness on corneal flattening in human eyes. Refract Corneal Surg. 1991 Jan-Feb;7(1):46–50. [PubMed] [Google Scholar]
- Burris T. E., Baker P. C., Ayer C. T., Loomas B. E., Mathis M. L., Silvestrini T. A. Flattening of central corneal curvature with intrastromal corneal rings of increasing thickness: an eye-bank eye study. J Cataract Refract Surg. 1993;19 (Suppl):182–187. doi: 10.1016/s0886-3350(13)80404-x. [DOI] [PubMed] [Google Scholar]
- Cennamo G., Rosa N., Del Prete A., Breve M. A., Sebastiani A. The corneal endothelium 12 months after photorefractive keratectomy in high myopia. Acta Ophthalmol Scand. 1997 Apr;75(2):128–130. doi: 10.1111/j.1600-0420.1997.tb00106.x. [DOI] [PubMed] [Google Scholar]
- Chayet A. S., Assil K. K., Montes M., Espinosa-Lagana M., Castellanos A., Tsioulias G. Regression and its mechanisms after laser in situ keratomileusis in moderate and high myopia. Ophthalmology. 1998 Jul;105(7):1194–1199. doi: 10.1016/S0161-6420(98)97020-8. [DOI] [PubMed] [Google Scholar]
- Chayet A. S., Magallanes R., Montes M., Chavez S., Robledo N. Laser in situ keratomileusis for simple myopic, mixed, and simple hyperopic astigmatism. J Refract Surg. 1998 Apr;14(2 Suppl):S175–S176. doi: 10.3928/1081-597X-19980401-05. [DOI] [PubMed] [Google Scholar]
- Choyce D. P. The correction of refractive errors with polysulfone corneal inlays. A new frontier to be explored? Trans Ophthalmol Soc U K. 1985;104(Pt 3):332–342. [PubMed] [Google Scholar]
- D'Hermies F., Hartmann C., von Ey F., Holzkämper C., Renard G., Pouliquen Y. Biocompatibility of a refractive intracorneal PMMA ring. Fortschr Ophthalmol. 1991;88(6):790–793. [PubMed] [Google Scholar]
- Davidorf J. M., Zaldivar R., Oscherow S. Results and complications of laser in situ keratomileusis by experienced surgeons. J Refract Surg. 1998 Mar-Apr;14(2):114–122. doi: 10.3928/1081-597X-19980301-09. [DOI] [PubMed] [Google Scholar]
- Dulaney D. D., Barnet R. W., Perkins S. A., Kezirian G. M. Laser in situ keratomileusis for myopia and astigmatism: 6 month results. J Cataract Refract Surg. 1998 Jun;24(6):758–764. doi: 10.1016/s0886-3350(98)80127-2. [DOI] [PubMed] [Google Scholar]
- Farah S. G., Azar D. T., Gurdal C., Wong J. Laser in situ keratomileusis: literature review of a developing technique. J Cataract Refract Surg. 1998 Jul;24(7):989–1006. doi: 10.1016/s0886-3350(98)80056-4. [DOI] [PubMed] [Google Scholar]
- Fleming J. F., Wan W. L., Schanzlin D. J. The theory of corneal curvature change with the Intrastromal Corneal Ring. CLAO J. 1989 Apr-Jun;15(2):146–150. [PubMed] [Google Scholar]
- Gartry D. S., Kerr Muir M. G., Marshall J. Excimer laser photorefractive keratectomy. 18-month follow-up. Ophthalmology. 1992 Aug;99(8):1209–1219. doi: 10.1016/s0161-6420(92)31821-4. [DOI] [PubMed] [Google Scholar]
- Gartry D. S., Kerr Muir M., Marshall J. The effect of topical corticosteroids on refraction and corneal haze following excimer laser treatment of myopia: an update. A prospective, randomised, double-masked study. Eye (Lond) 1993;7(Pt 4):584–590. doi: 10.1038/eye.1993.127. [DOI] [PubMed] [Google Scholar]
- Gartry D. S., Muir M. G., Lohmann C. P., Marshall J. The effect of topical corticosteroids on refractive outcome and corneal haze after photorefractive keratectomy. A prospective, randomized, double-blind trial. Arch Ophthalmol. 1992 Jul;110(7):944–952. doi: 10.1001/archopht.1992.01080190050028. [DOI] [PubMed] [Google Scholar]
- Ginsburg A. P., Waring G. O., 3rd, Steinberg E. B., Williams P. A., Justin N., Deitz J. R., Roszka-Duggan V. K., Baluvelt K., Bourque L. Contrast sensitivity under photopic conditions in the Prospective Evaluation of Radial Keratotomy (PERK) Study. Refract Corneal Surg. 1990 Mar-Apr;6(2):82–91. [PubMed] [Google Scholar]
- Goosey J. D., Prager T. C., Goosey C. B., Allison M. E., Marvelli T. L. Stability of refraction during two years after myopic epikeratoplasty. Refract Corneal Surg. 1990 Jan-Feb;6(1):4–8. [PubMed] [Google Scholar]
- Hefetz L., Domnitz Y., Haviv D., Krakowsky D., Kibarsky Y., Abrahami S., Nemet P. Influence of patient age on refraction and corneal haze after photorefractive keratectomy. Br J Ophthalmol. 1997 Aug;81(8):637–638. doi: 10.1136/bjo.81.8.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helena M. C., Meisler D., Wilson S. E. Epithelial growth within the lamellar interface after laser in situ keratomileusis (LASIK) Cornea. 1997 May;16(3):300–305. [PubMed] [Google Scholar]
- Hersh P. S., Brint S. F., Maloney R. K., Durrie D. S., Gordon M., Michelson M. A., Thompson V. M., Berkeley R. B., Schein O. D., Steinert R. F. Photorefractive keratectomy versus laser in situ keratomileusis for moderate to high myopia. A randomized prospective study. Ophthalmology. 1998 Aug;105(8):1512-22, discussion 1522-3. doi: 10.1016/S0161-6420(98)98038-1. [DOI] [PubMed] [Google Scholar]
- Hersh P. S., Schein O. D., Steinert R. Characteristics influencing outcomes of excimer laser photorefractive keratectomy. Summit Photorefractive Keratectomy Phase III Study Group. Ophthalmology. 1996 Nov;103(11):1962–1969. doi: 10.1016/s0161-6420(96)30401-6. [DOI] [PubMed] [Google Scholar]
- Hodkin M. J., Lemos M. M., McDonald M. B., Holladay J. T., Shahidi S. H. Near vision contrast sensitivity after photorefractive keratectomy. J Cataract Refract Surg. 1997 Mar;23(2):192–195. doi: 10.1016/s0886-3350(97)80341-0. [DOI] [PubMed] [Google Scholar]
- Jones S. S., Azar R. G., Cristol S. M., Geroski D. H., Waring G. O., 3rd, Stulting R. D., Thompson K. P., Edelhauser H. F. Effects of laser in situ keratomileusis (LASIK) on the corneal endothelium. Am J Ophthalmol. 1998 Apr;125(4):465–471. doi: 10.1016/s0002-9394(99)80186-x. [DOI] [PubMed] [Google Scholar]
- Kaufman H. E., Werblin T. P. Epikeratophakia for the treatment of keratoconus. Am J Ophthalmol. 1982 Mar;93(3):342–347. doi: 10.1016/0002-9394(82)90537-2. [DOI] [PubMed] [Google Scholar]
- Kirkham S. M., Dangel M. E. The keratoprosthesis: improved biocompatibility through design and surface modification. Ophthalmic Surg. 1991 Aug;22(8):455–461. [PubMed] [Google Scholar]
- Koenig S. B., Hamano T., Yamaguchi T., Kimura T., McDonald M. B., Kaufman H. E. Refractive keratoplasty with hydrogel implants in primates. Ophthalmic Surg. 1984 Mar;15(3):225–229. [PubMed] [Google Scholar]
- Kratz-Owens K., Huff J. W., Schanzlin D. J. New cryoprotectant for cryorefractive surgery. J Cataract Refract Surg. 1991 Sep;17(5):608–612. doi: 10.1016/s0886-3350(13)81049-8. [DOI] [PubMed] [Google Scholar]
- Lane S. L., Lindstrom R. L., Cameron J. D., Thomas R. H., Mindrup E. A., Waring G. O., 3rd, McCarey B. E., Binder P. S. Polysulfone corneal lenses. J Cataract Refract Surg. 1986 Jan;12(1):50–60. doi: 10.1016/s0886-3350(86)80057-8. [DOI] [PubMed] [Google Scholar]
- Lee T. J., Wan W. L., Kash R. L., Kratz K. L., Schanzlin D. J. Keratocyte survival following a controlled-rate freeze. Invest Ophthalmol Vis Sci. 1985 Sep;26(9):1210–1215. [PubMed] [Google Scholar]
- Legeais J. M., Renard G., Parel J. M., Serdarevic O., Mei-Mui M., Pouliquen Y. Expanded fluorocarbon for keratoprosthesis cellular ingrowth and transparency. Exp Eye Res. 1994 Jan;58(1):41–51. doi: 10.1006/exer.1994.1193. [DOI] [PubMed] [Google Scholar]
- Lindstrom R. L., Hardten D. R., Chu Y. R. Laser In Situ keratomileusis (LASIK) for the treatment of low moderate, and high myopia. Trans Am Ophthalmol Soc. 1997;95:285–306. [PMC free article] [PubMed] [Google Scholar]
- Lipshitz I., Loewenstein A., Varssano D., Lazar M. Late onset corneal haze after photorefractive keratectomy for moderate and high myopia. Ophthalmology. 1997 Mar;104(3):369–374. doi: 10.1016/s0161-6420(97)30306-6. [DOI] [PubMed] [Google Scholar]
- Loewenstein A., Lipshitz I., Varssano D., Lazar M. Complications of excimer laser photorefractive keratectomy for myopia. J Cataract Refract Surg. 1997 Oct;23(8):1174–1176. doi: 10.1016/s0886-3350(97)80311-2. [DOI] [PubMed] [Google Scholar]
- Lohmann C. P., Güell J. L. Regression after LASIK for the treatment of myopia: the role of the corneal epithelium. Semin Ophthalmol. 1998 Jun;13(2):79–82. doi: 10.3109/08820539809059822. [DOI] [PubMed] [Google Scholar]
- Lynn M. J., Waring G. O., 3rd, Sperduto R. D. Factors affecting outcome and predictability of radial keratotomy in the PERK Study. Arch Ophthalmol. 1987 Jan;105(1):42–51. doi: 10.1001/archopht.1987.01060010048030. [DOI] [PubMed] [Google Scholar]
- MacRae S. M., Rich L. F. Long-term effects of radial keratotomy on the corneal endothelium. J Refract Surg. 1998 Jan-Feb;14(1):49–52. doi: 10.3928/1081-597X-19980101-10. [DOI] [PubMed] [Google Scholar]
- Maldonado-Bas A., Onnis R. Results of laser in situ keratomileusis in different degrees of myopia. Ophthalmology. 1998 Apr;105(4):606–611. doi: 10.1016/S0161-6420(98)94012-X. [DOI] [PubMed] [Google Scholar]
- Martínez C. E., Applegate R. A., Klyce S. D., McDonald M. B., Medina J. P., Howland H. C. Effect of pupillary dilation on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol. 1998 Aug;116(8):1053–1062. doi: 10.1001/archopht.116.8.1053. [DOI] [PubMed] [Google Scholar]
- McCarey B. E., Andrews D. M. Refractive keratoplasty with intrastromal hydrogel lenticular implants. Invest Ophthalmol Vis Sci. 1981 Jul;21(1 Pt 1):107–115. [PubMed] [Google Scholar]
- McDonald M. B., Kaufman H. E., Aquavella J. V., Durrie D. S., Hiles D. A., Hunkeler J. D., Keates R. H., Morgan K. S., Sanders D. R. The nationwide study of epikeratophakia for aphakia in adults. Am J Ophthalmol. 1987 Mar 15;103(3 Pt 2):358–365. doi: 10.1016/s0002-9394(14)77758-x. [DOI] [PubMed] [Google Scholar]
- McDonald M. B., Kaufman H. E., Aquavella J. V., Durrie D. S., Hiles D. A., Hunkeler J. D., Keates R. H., Morgan K. S., Sanders D. R. The nationwide study of epikeratophakia for myopia. Am J Ophthalmol. 1987 Mar 15;103(3 Pt 2):375–383. doi: 10.1016/s0002-9394(14)77760-8. [DOI] [PubMed] [Google Scholar]
- McDonald M. B., Kaufman H. E., Durrie D. S., Keates R. H., Sanders D. R. Epikeratophakia for keratoconus. The nationwide study. Arch Ophthalmol. 1986 Sep;104(9):1294–1300. doi: 10.1001/archopht.1986.01050210048024. [DOI] [PubMed] [Google Scholar]
- McDonald M. B., Koenig S. B., Safir A., Kaufman H. E. On-lay lamellar keratoplasty for the treatment of keratoconus. Br J Ophthalmol. 1983 Sep;67(9):615–618. doi: 10.1136/bjo.67.9.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonnell P. J., Nizam A., Lynn M. J., Waring G. O., 3rd Morning-to-evening change in refraction, corneal curvature, and visual acuity 11 years after radial keratotomy in the prospective evaluation of radial keratotomy study. The PERK Study Group. Ophthalmology. 1996 Feb;103(2):233–239. doi: 10.1016/s0161-6420(96)30711-2. [DOI] [PubMed] [Google Scholar]
- Morgan K. S., Marvelli T. L., Ellis G. S., Jr, Arffa R. C. Epikeratophakia in children with traumatic cataracts. J Pediatr Ophthalmol Strabismus. 1986 May-Jun;23(3):108–114. doi: 10.3928/0191-3913-19860501-03. [DOI] [PubMed] [Google Scholar]
- Morgan K. S., McDonald M. B., Hiles D. A., Aquavella J. V., Durrie D. S., Hunkeler J. D., Kaufman H. E., Keates R. H., Sanders D. R. The nationwide study of epikeratophakia for aphakia in older children. Ophthalmology. 1988 Apr;95(4):526–532. doi: 10.1016/s0161-6420(88)33159-3. [DOI] [PubMed] [Google Scholar]
- Nagy Z., Krasznai G., Módis L., Jr, Sefcsik I., Furka I., Mikó I. Intrastromal corneal ring, a new refractive surgical technique to decrease myopia. Experimental and clinical results. Acta Chir Hung. 1997;36(1-4):248–250. [PubMed] [Google Scholar]
- Nosé W., Neves R. A., Burris T. E., Schanzlin D. J., Belfort Júnior R. Intrastromal corneal ring: 12-month sighted myopic eyes. J Refract Surg. 1996 Jan-Feb;12(1):20–28. doi: 10.3928/1081-597X-19960101-08. [DOI] [PubMed] [Google Scholar]
- Nosé W., Neves R. A., Schanzlin D. J., Belfort Júnior R. Intrastromal corneal ring--one-year results of first implants in humans: a preliminary nonfunctional eye study. Refract Corneal Surg. 1993 Nov-Dec;9(6):452–458. [PubMed] [Google Scholar]
- Pallikaris I. G., Papatzanaki M. E., Siganos D. S., Tsilimbaris M. K. A corneal flap technique for laser in situ keratomileusis. Human studies. Arch Ophthalmol. 1991 Dec;109(12):1699–1702. doi: 10.1001/archopht.1991.01080120083031. [DOI] [PubMed] [Google Scholar]
- Pallikaris I. G., Siganos D. S. Excimer laser in situ keratomileusis and photorefractive keratectomy for correction of high myopia. J Refract Corneal Surg. 1994 Sep-Oct;10(5):498–510. [PubMed] [Google Scholar]
- Pallikaris I. G., Siganos D. S. Excimer laser in situ keratomileusis and photorefractive keratectomy for correction of high myopia. J Refract Corneal Surg. 1994 Sep-Oct;10(5):498–510. [PubMed] [Google Scholar]
- Parks R. A., McCarey B. E., Knight P. M., Storie B. R. Intrastromal crystalline deposits following hydrogel keratophakia in monkeys. Cornea. 1993 Jan;12(1):29–34. doi: 10.1097/00003226-199301000-00006. [DOI] [PubMed] [Google Scholar]
- Pietilä J., Mäkinen P., Pajari S., Uusitalo H. Photorefractive keratectomy for -1.25 to -25.00 diopters of myopia. J Refract Surg. 1998 Nov-Dec;14(6):615–622. doi: 10.3928/1081-597X-19981101-08. [DOI] [PubMed] [Google Scholar]
- Pirzada W. A., Kalaawry H. Laser in situ keratomileusis for myopia of -1 to -3.50 diopters. J Refract Surg. 1997 Aug;13(5 Suppl):S425–S426. doi: 10.3928/1081-597X-19970801-05. [DOI] [PubMed] [Google Scholar]
- Price F. W., Jr, Binder P. S. Scarring of a recipient cornea following epikeratoplasty. Arch Ophthalmol. 1987 Nov;105(11):1556–1560. doi: 10.1001/archopht.1987.01060110102041. [DOI] [PubMed] [Google Scholar]
- Probst L. E., Machat J. J. Mathematics of laser in situ keratomileusis for high myopia. J Cataract Refract Surg. 1998 Feb;24(2):190–195. doi: 10.1016/s0886-3350(98)80199-5. [DOI] [PubMed] [Google Scholar]
- Pérez-Santonja J. J., Sakla H. F., Alió J. L. Contrast sensitivity after laser in situ keratomileusis. J Cataract Refract Surg. 1998 Feb;24(2):183–189. doi: 10.1016/s0886-3350(98)80198-3. [DOI] [PubMed] [Google Scholar]
- Pérez-Santonja J. J., Sakla H. F., Gobbi F., Alió J. L. Corneal endothelial changes after laser in situ keratomileusis. J Cataract Refract Surg. 1997 Mar;23(2):177–183. doi: 10.1016/s0886-3350(97)80339-2. [DOI] [PubMed] [Google Scholar]
- Quantock A. J., Kincaid M. C., Schanzlin D. J. Stromal healing following explantation of an ICR (intrastromal corneal ring) from a nonfunctional human eye. Arch Ophthalmol. 1995 Feb;113(2):208–209. doi: 10.1001/archopht.1995.01100020092036. [DOI] [PubMed] [Google Scholar]
- Rosa N., Cennamo G., Del Prete A., Bianco S., Sebastiani A. Endothelial cells evaluation two years after photorefractive keratectomy. Ophthalmologica. 1997;211(1):32–39. doi: 10.1159/000310871. [DOI] [PubMed] [Google Scholar]
- Rowsey J. J., Balyeat H. D., Rabinovitch B., Burris T. E., Hays J. C. Predicting the results of radial keratotomy. Ophthalmology. 1983 Jun;90(6):642–654. doi: 10.1016/s0161-6420(83)34504-8. [DOI] [PubMed] [Google Scholar]
- Sanders D. R., Deitz M. R., Gallagher D. Factors affecting predictability of radial keratotomy. Ophthalmology. 1985 Sep;92(9):1237–1243. doi: 10.1016/s0161-6420(85)33874-5. [DOI] [PubMed] [Google Scholar]
- Sawelson H., Marks R. G. Five-year results of radial keratotomy. Refract Corneal Surg. 1989 Jan-Feb;5(1):8–20. [PubMed] [Google Scholar]
- Schlote T., Kriegerowski M., Bende T., Derse M., Thiel H. J., Jean B. Mesopic vision in myopia corrected by photorefractive keratectomy, soft contact lenses, and spectacles. J Cataract Refract Surg. 1997 Jun;23(5):718–725. doi: 10.1016/s0886-3350(97)80280-5. [DOI] [PubMed] [Google Scholar]
- Scorolli L., Scorolli L., Scalinci S. Z., Savini G., Meduri R. Hyperopic shift after 4-8 incision radial keratotomy: eight-year follow-up. Eur J Ophthalmol. 1996 Oct-Dec;6(4):351–355. doi: 10.1177/112067219600600401. [DOI] [PubMed] [Google Scholar]
- Seiler T., Koufala K., Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998 May-Jun;14(3):312–317. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- Seiler T., McDonnell P. J. Excimer laser photorefractive keratectomy. Surv Ophthalmol. 1995 Sep-Oct;40(2):89–118. doi: 10.1016/s0039-6257(95)80001-8. [DOI] [PubMed] [Google Scholar]
- Seiler T., Quurke A. W. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998 Jul;24(7):1007–1009. doi: 10.1016/s0886-3350(98)80057-6. [DOI] [PubMed] [Google Scholar]
- Shah S. S., Kapadia M. S., Meisler D. M., Wilson S. E. Photorefractive keratectomy using the summit SVS Apex laser with or without astigmatic keratotomy. Cornea. 1998 Sep;17(5):508–516. doi: 10.1097/00003226-199809000-00008. [DOI] [PubMed] [Google Scholar]
- Slack J. W., Kangas T. A., Edelhauser H. F., Geroski D. H., McDermott M. L. Comparison of corneal preservation media for corneal hydration and stromal proteoglycan loss. Cornea. 1992 May;11(3):204–210. [PubMed] [Google Scholar]
- Stulting R. D., Thompson K. P., Waring G. O., 3rd, Lynn M. The effect of photorefractive keratectomy on the corneal endothelium. Ophthalmology. 1996 Sep;103(9):1357–1365. doi: 10.1016/s0161-6420(96)30496-x. [DOI] [PubMed] [Google Scholar]
- Swinger C. A. Variables in radial keratotomy. Trans New Orleans Acad Ophthalmol. 1987;35:89–110. [PubMed] [Google Scholar]
- Tabin G. C., Alpins N., Aldred G. F., McCarty C. A., Taylor H. R. Astigmatic change 1 year after excimer laser treatment of myopia and myopic astigmatism. Melbourne Excimer Laser Group. J Cataract Refract Surg. 1996 Sep;22(7):924–930. doi: 10.1016/s0886-3350(96)80193-3. [DOI] [PubMed] [Google Scholar]
- Trinkaus-Randall V., Capecchi J., Newton A., Vadasz A., Leibowitz H., Franzblau C. Development of a biopolymeric keratoprosthetic material. Evaluation in vitro and in vivo. Invest Ophthalmol Vis Sci. 1988 Mar;29(3):393–400. [PubMed] [Google Scholar]
- Trokel S. L., Srinivasan R., Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol. 1983 Dec;96(6):710–715. doi: 10.1016/s0002-9394(14)71911-7. [DOI] [PubMed] [Google Scholar]
- Verdon W., Bullimore M., Maloney R. K. Visual performance after photorefractive keratectomy. A prospective study. Arch Ophthalmol. 1996 Dec;114(12):1465–1472. doi: 10.1001/archopht.1996.01100140663003. [DOI] [PubMed] [Google Scholar]
- Verity S. M., Talamo J. H., Chayet A., Wolf T. C., Rapoza P., Schanzlin D. J., Lane S., Kenyon K., Assil K. K. The combined (Genesis) technique of radial keratotomy. A prospective, multicenter study. Refractive Keratoplasty Study Group. Ophthalmology. 1995 Dec;102(12):1908–1917. doi: 10.1016/s0161-6420(95)30776-2. [DOI] [PubMed] [Google Scholar]
- Wang Z., Chen J., Yang B. Comparison of laser in situ keratomileusis and photorefractive keratectomy to correct myopia from -1.25 to -6.00 diopters. J Refract Surg. 1997 Sep-Oct;13(6):528–534. doi: 10.3928/1081-597X-19970901-09. [DOI] [PubMed] [Google Scholar]
- Waring G. O., 3rd, Casebeer J. C., Dru R. M. One-year results of a prospective multicenter study of the Casebeer system of refractive keratotomy. Casebeer Chiron Study Group. Ophthalmology. 1996 Sep;103(9):1337–1347. doi: 10.1016/s0161-6420(96)30498-3. [DOI] [PubMed] [Google Scholar]
- Waring G. O., 3rd, Lynn M. J., Culbertson W., Laibson P. R., Lindstrom R. D., McDonald M. B., Myers W. D., Obstbaum S. A., Rowsey J. J., Schanzlin D. J. Three year results of the Prospective Evaluation of Radial Keratotomy (PERK) study. Indian J Ophthalmol. 1990 Jul-Sep;38(3):107–113. [PubMed] [Google Scholar]
- Waring G. O., 3rd, Lynn M. J., Fielding B., Asbell P. A., Balyeat H. D., Cohen E. A., Culbertson W., Doughman D. J., Fecko P., McDonald M. B. Results of the Prospective Evaluation of Radial Keratotomy (PERK) Study 4 years after surgery for myopia. Perk Study Group. JAMA. 1990 Feb 23;263(8):1083–1091. [PubMed] [Google Scholar]
- Waring G. O., 3rd, Lynn M. J., Gelender H., Laibson P. R., Lindstrom R. L., Myers W. D., Obstbaum S. A., Rowsey J. J., McDonald M. B., Schanzlin D. J. Results of the prospective evaluation of radial keratotomy (PERK) study one year after surgery. Ophthalmology. 1985 Feb;92(2):177-98, 307. doi: 10.1016/s0161-6420(85)34054-x. [DOI] [PubMed] [Google Scholar]
- Waring G. O., 3rd, Lynn M. J., McDonnell P. J. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol. 1994 Oct;112(10):1298–1308. doi: 10.1001/archopht.1994.01090220048022. [DOI] [PubMed] [Google Scholar]
- Waring G. O., 3rd, Moffitt S. D., Gelender H., Laibson P. R., Lindstrom R. L., Myers W. D., Obstbaum S. A., Rowsey J. J., Safir A., Schanzlin D. J. Rationale for and design of the National Eye Institute Prospective Evaluation of Radial Keratotomy (PERK) Study. Ophthalmology. 1983 Jan;90(1):40–58. doi: 10.1016/s0161-6420(83)34603-0. [DOI] [PubMed] [Google Scholar]
- Werblin T. P., Stafford G. M. Hyperopic shift after refractive keratotomy using the Casebeer System. J Cataract Refract Surg. 1996 Oct;22(8):1030–1036. doi: 10.1016/s0886-3350(96)80115-5. [DOI] [PubMed] [Google Scholar]
- Werblin T. P., Stafford G. M. Three year results of refractive keratotomy using the Casebeer System. J Cataract Refract Surg. 1996 Oct;22(8):1023–1029. doi: 10.1016/s0886-3350(96)80114-3. [DOI] [PubMed] [Google Scholar]
- Werblin T. P., Stafford G. M. Three year results of refractive keratotomy using the Casebeer System. J Cataract Refract Surg. 1996 Oct;22(8):1023–1029. doi: 10.1016/s0886-3350(96)80114-3. [DOI] [PubMed] [Google Scholar]
- Yamaguchi T., Koenig S. B., Hamano T., Kimura T., Santana E., McDonald M. B., Kaufman H. E. Electron microscopic study of intrastromal hydrogel implants in primates. Ophthalmology. 1984 Oct;91(10):1170–1175. doi: 10.1016/s0161-6420(84)34153-7. [DOI] [PubMed] [Google Scholar]