Abstract
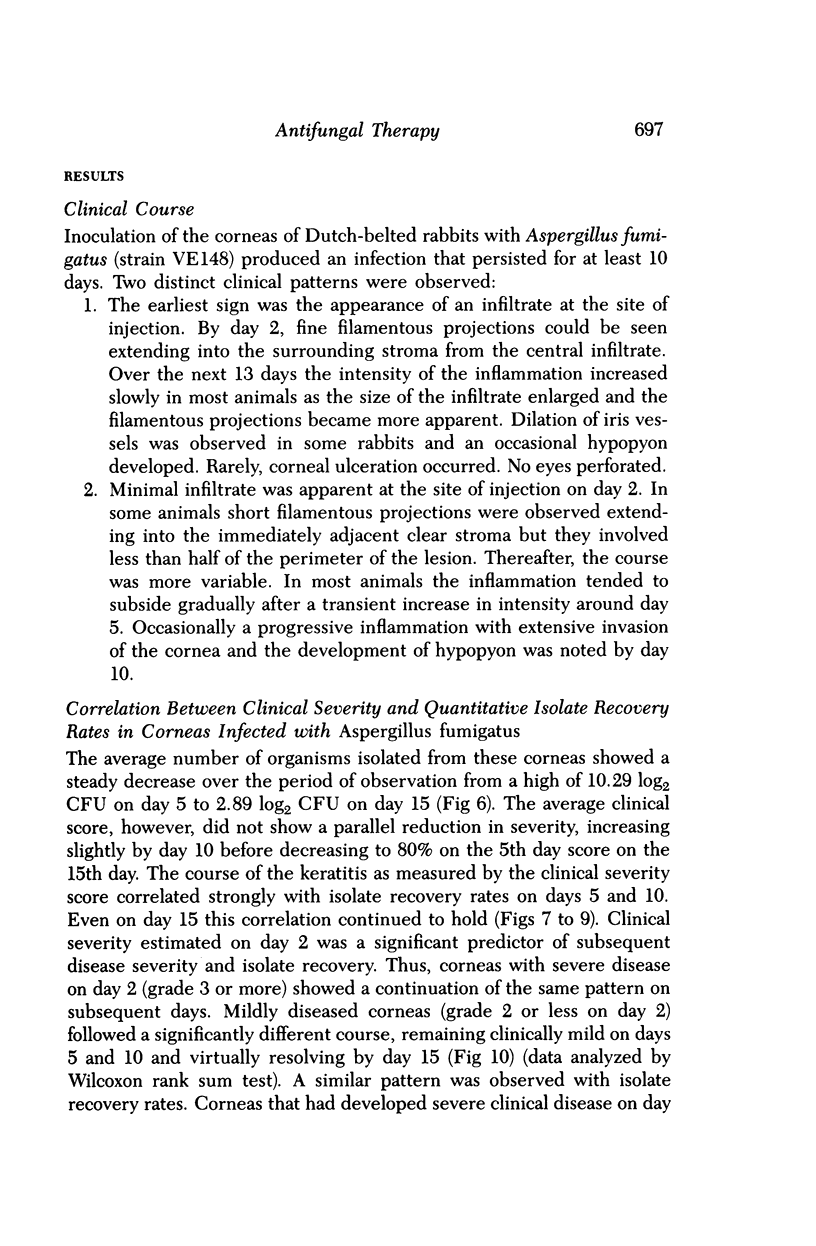
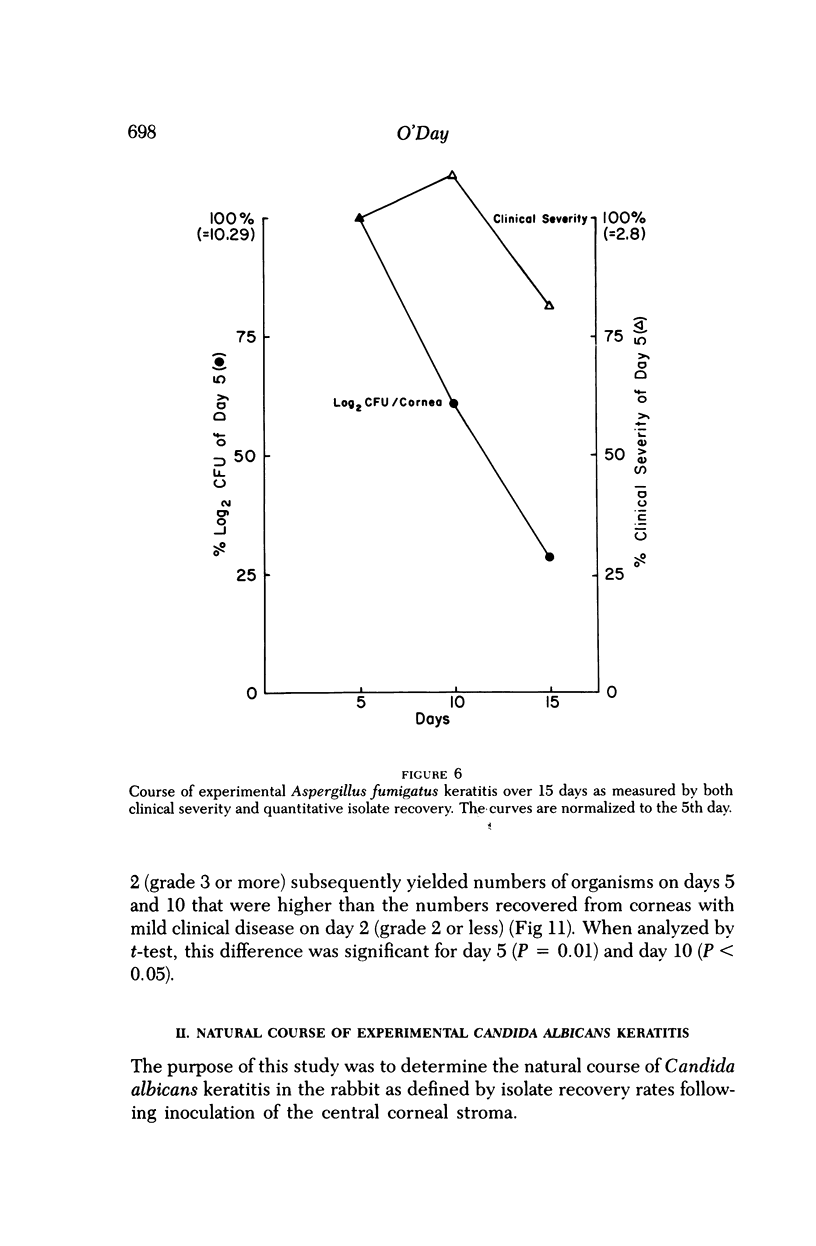
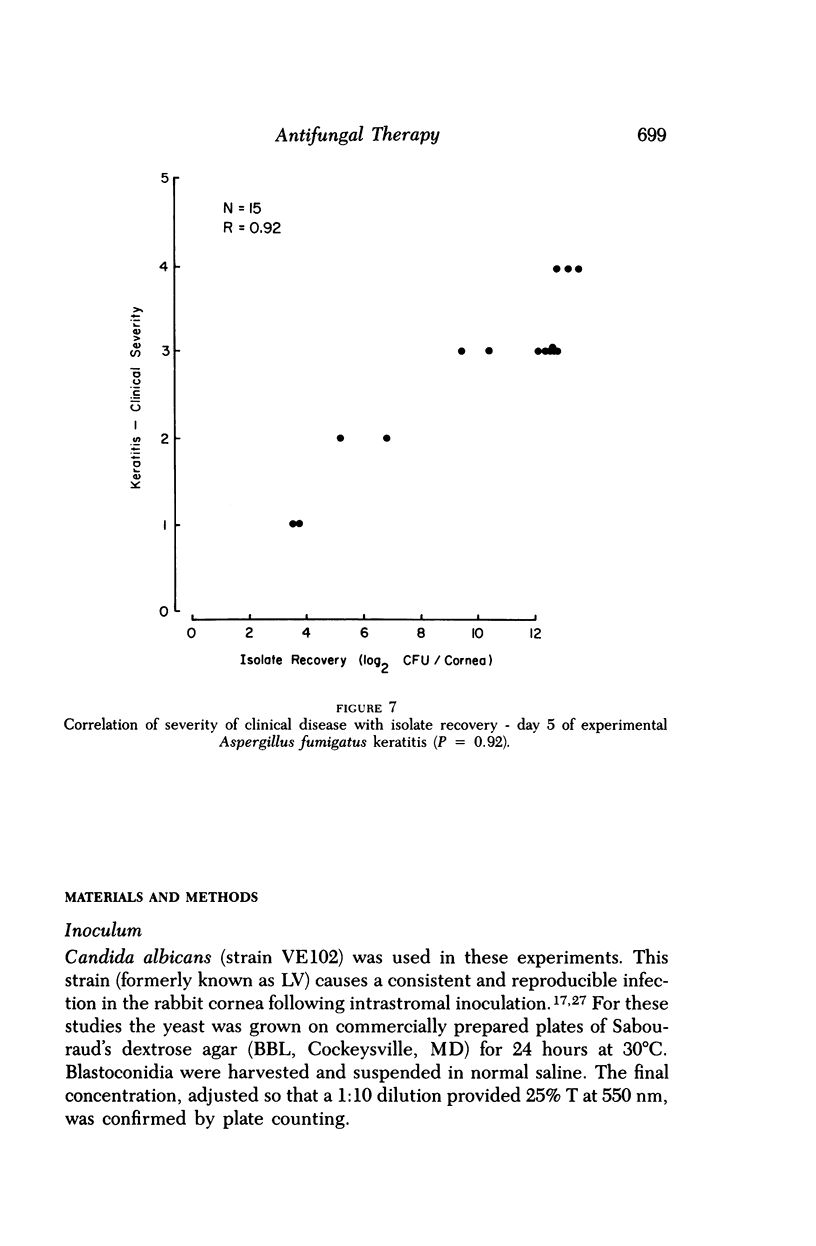
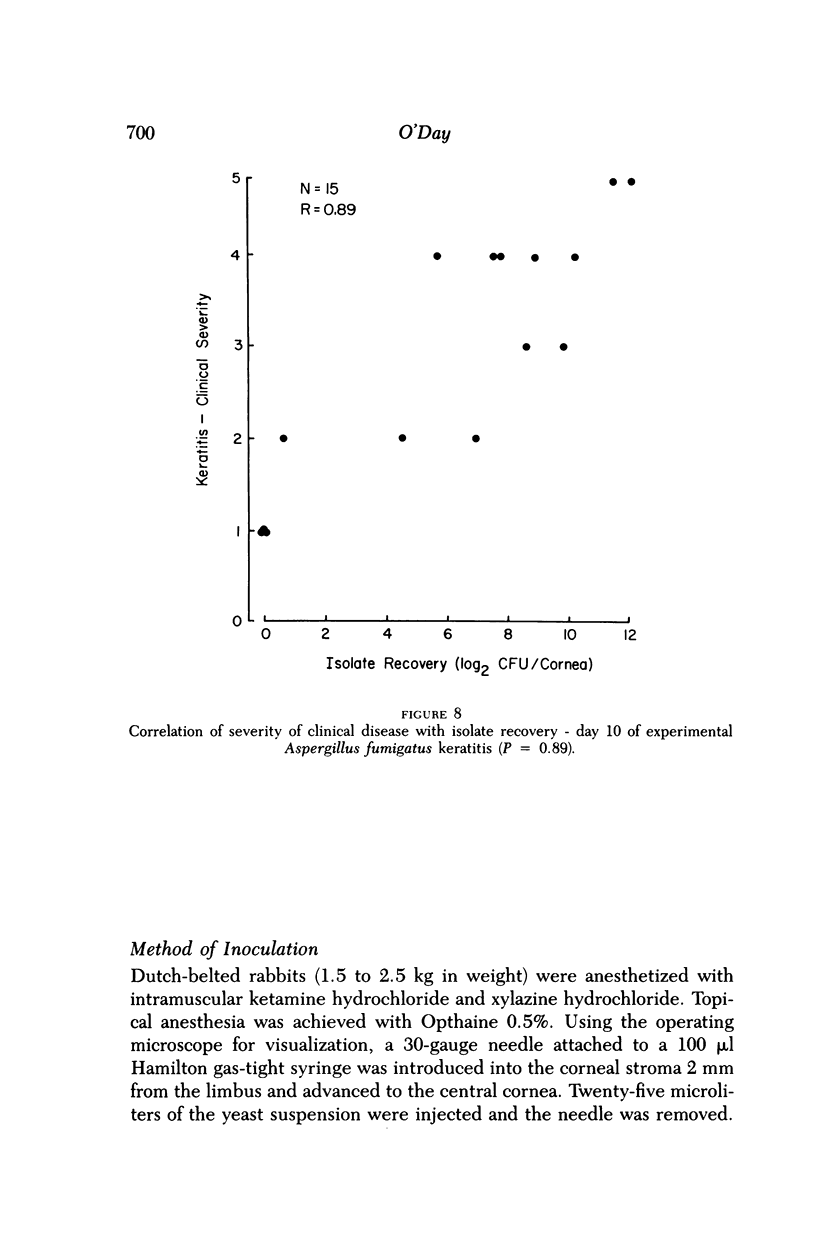
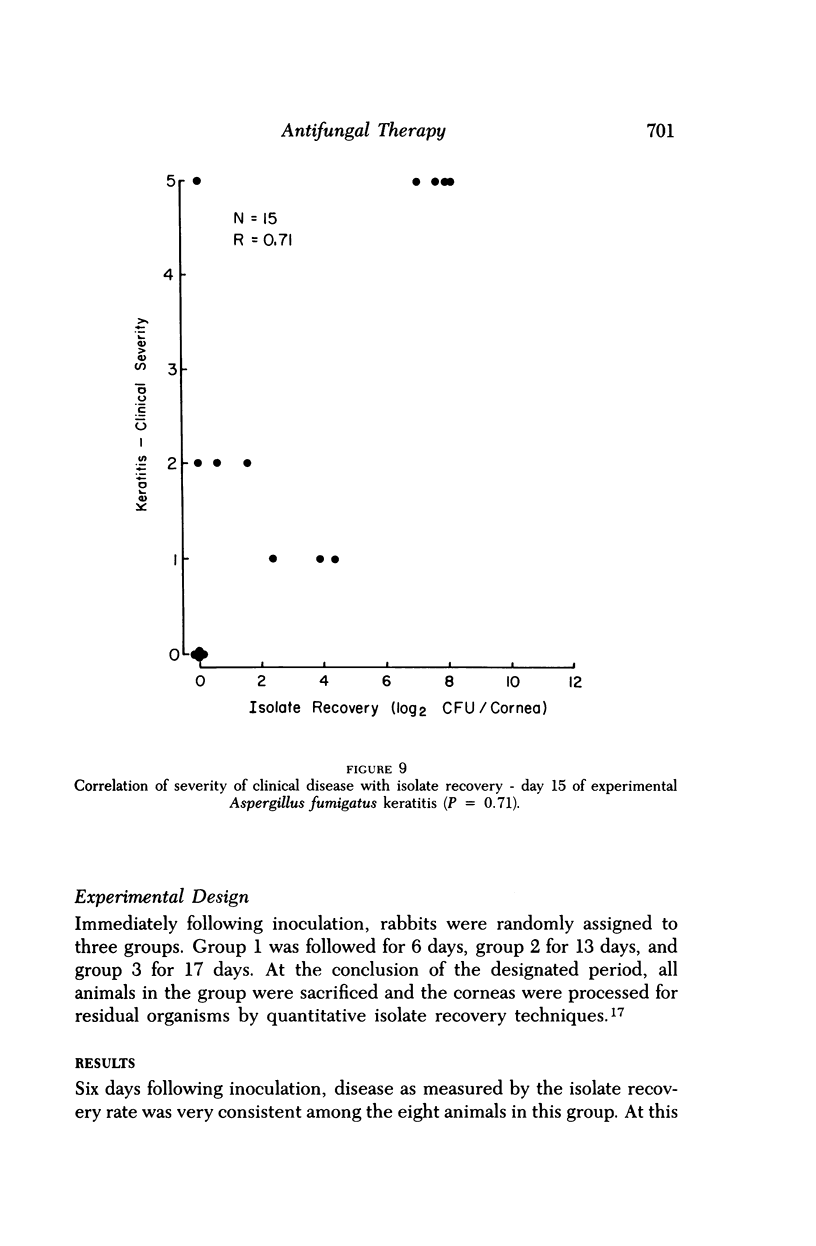
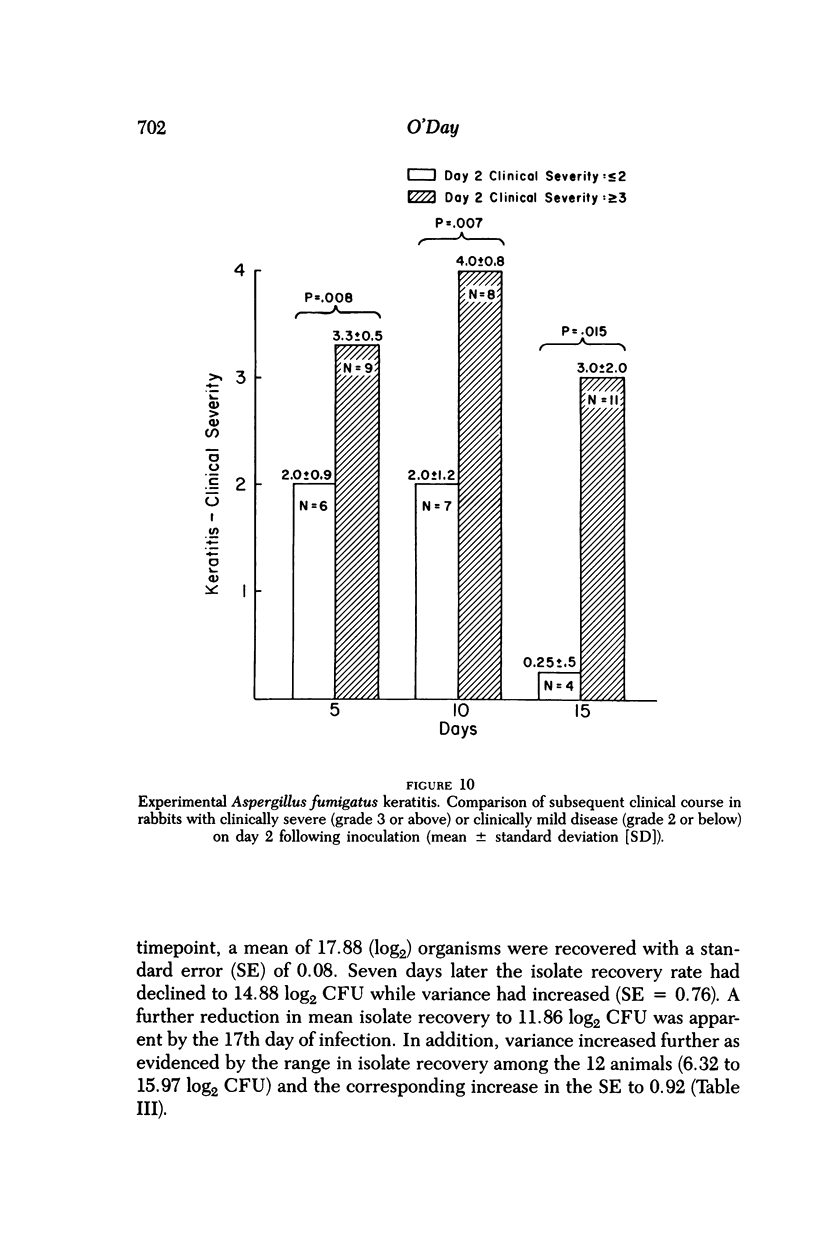
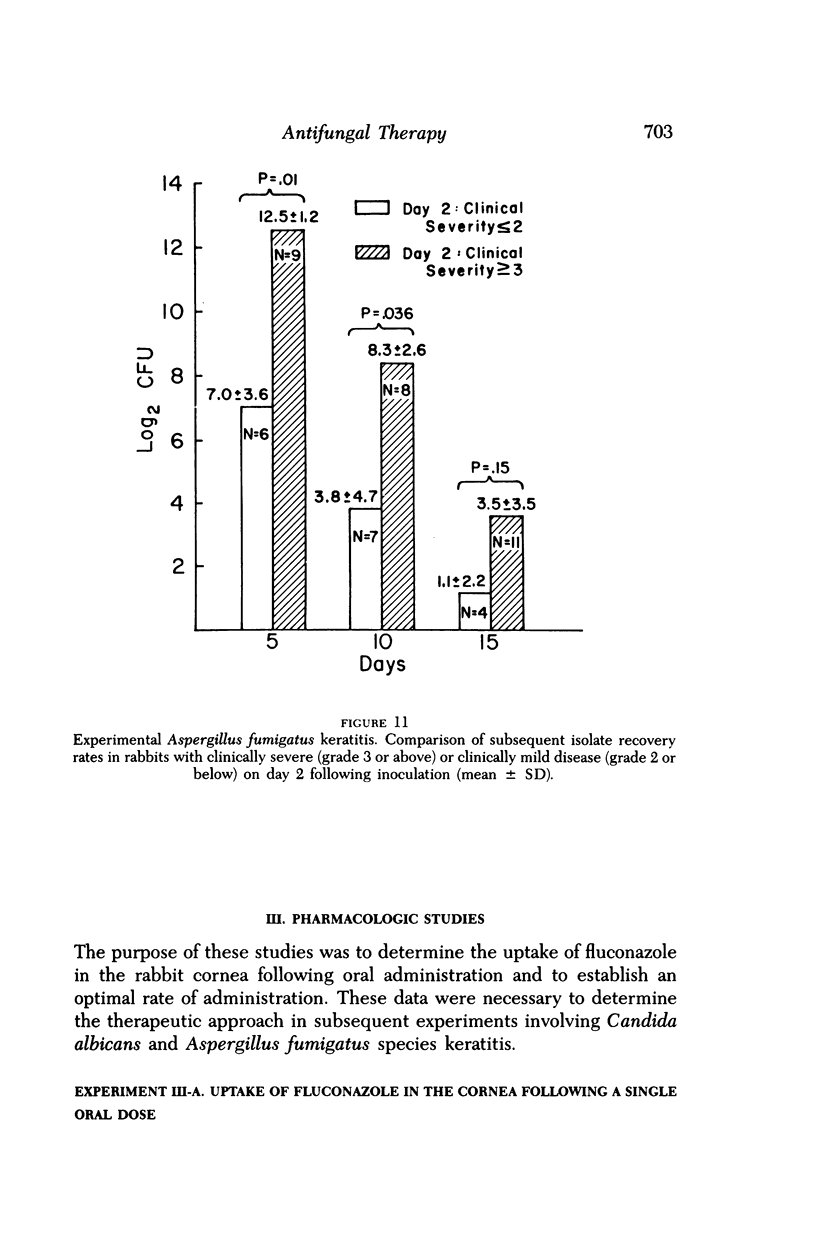
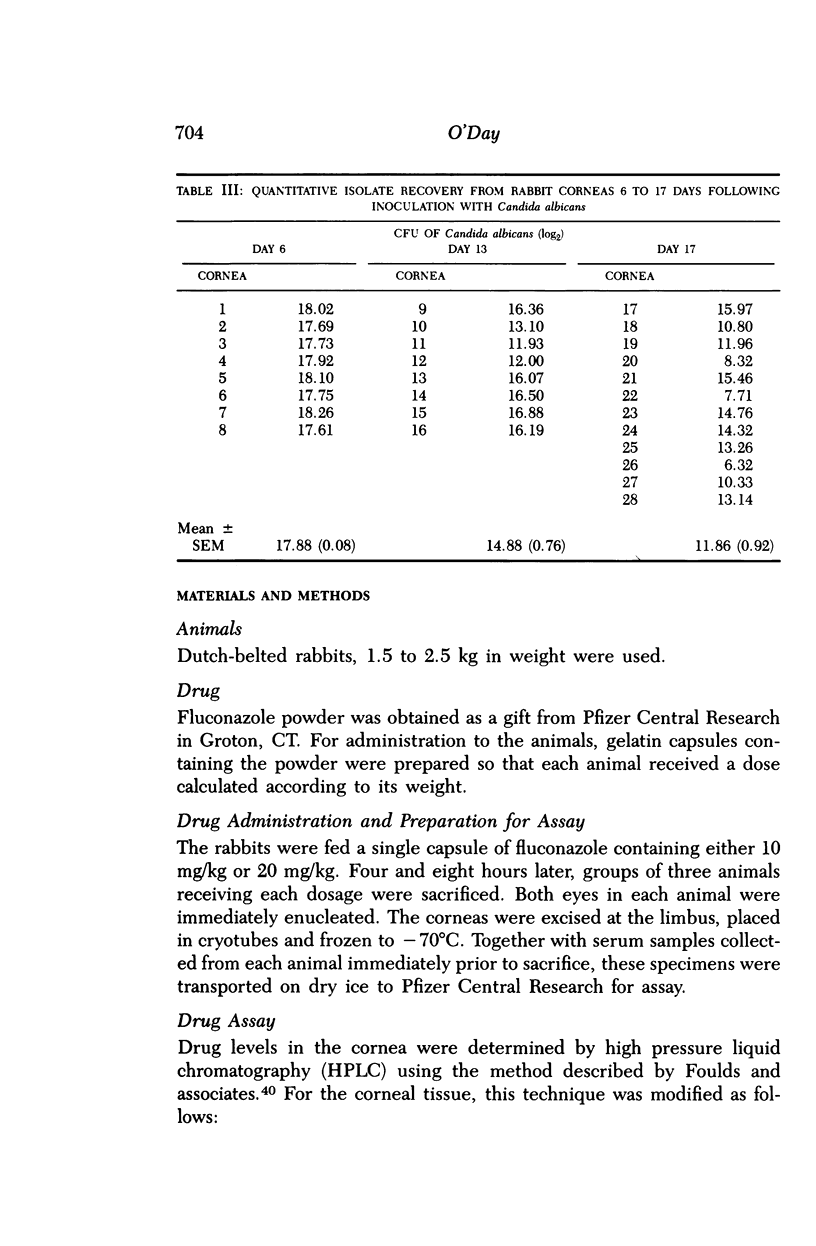
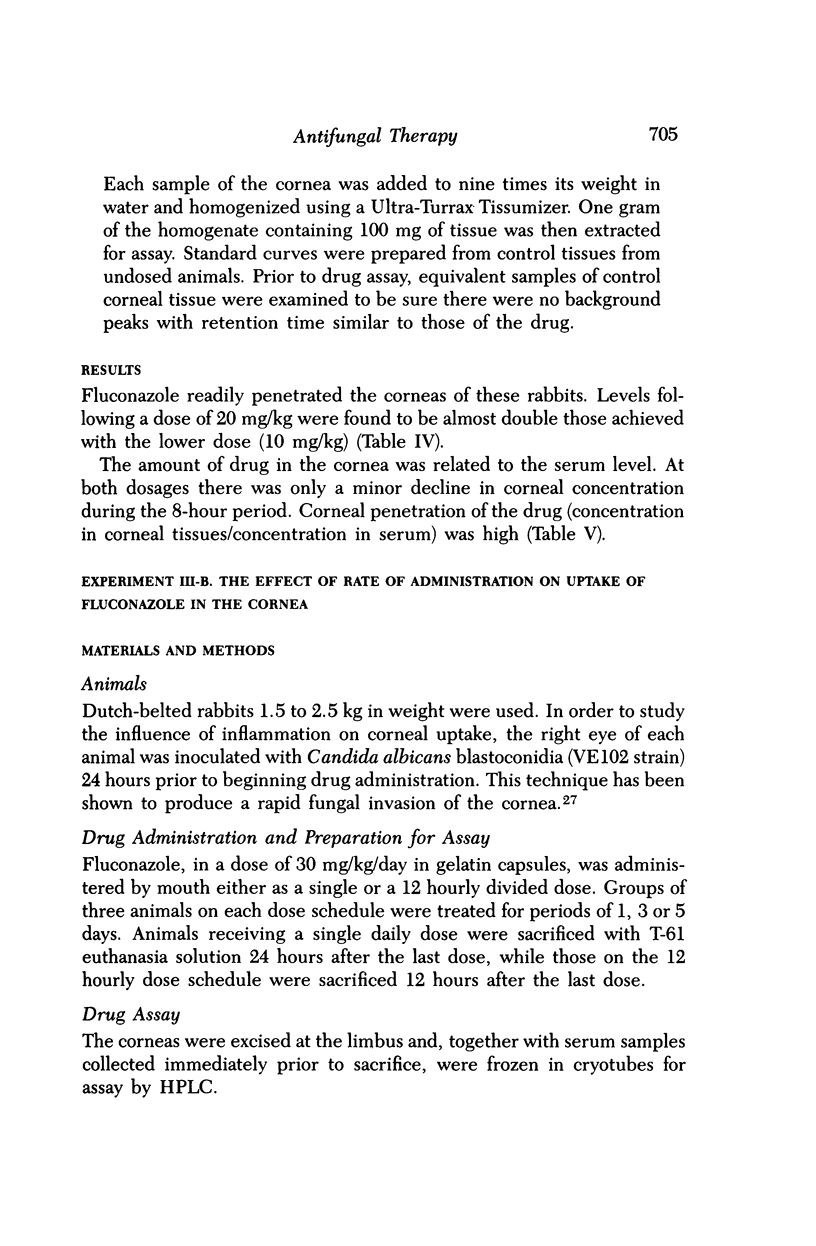
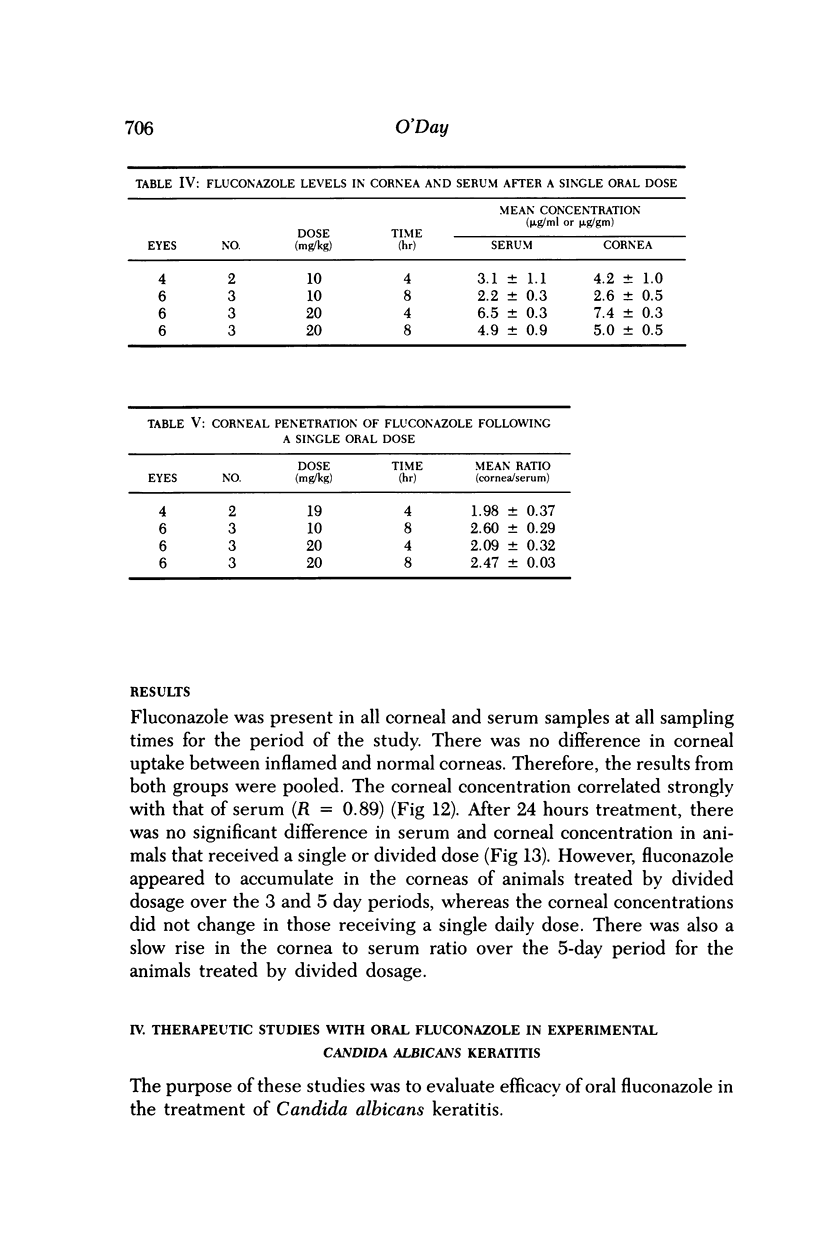
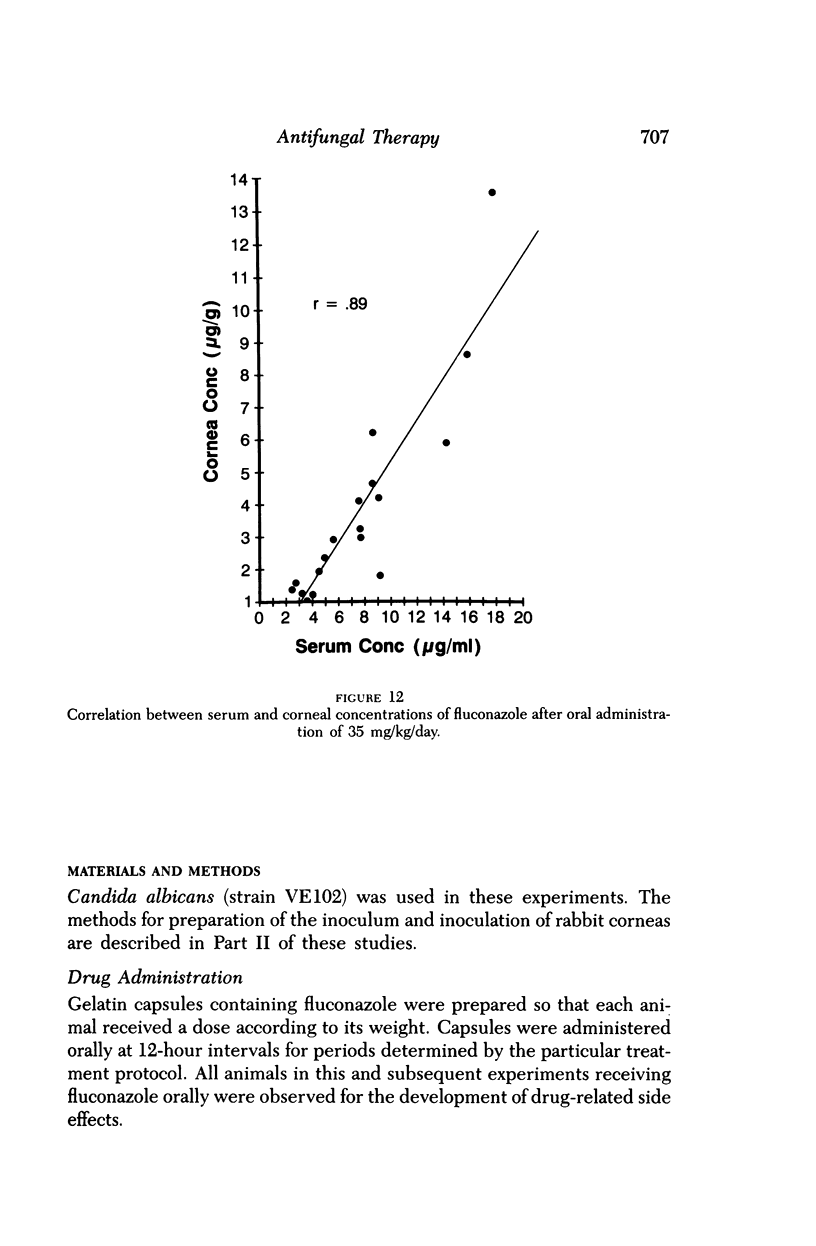
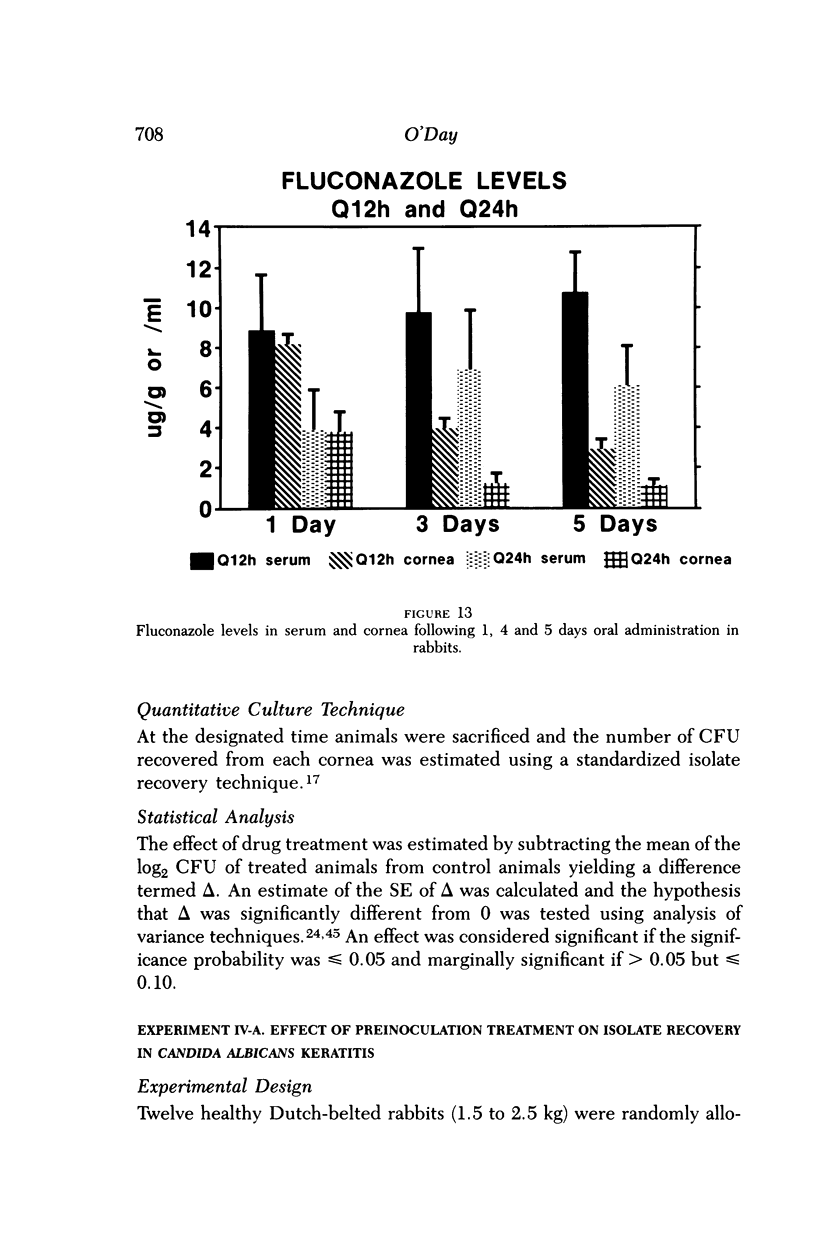
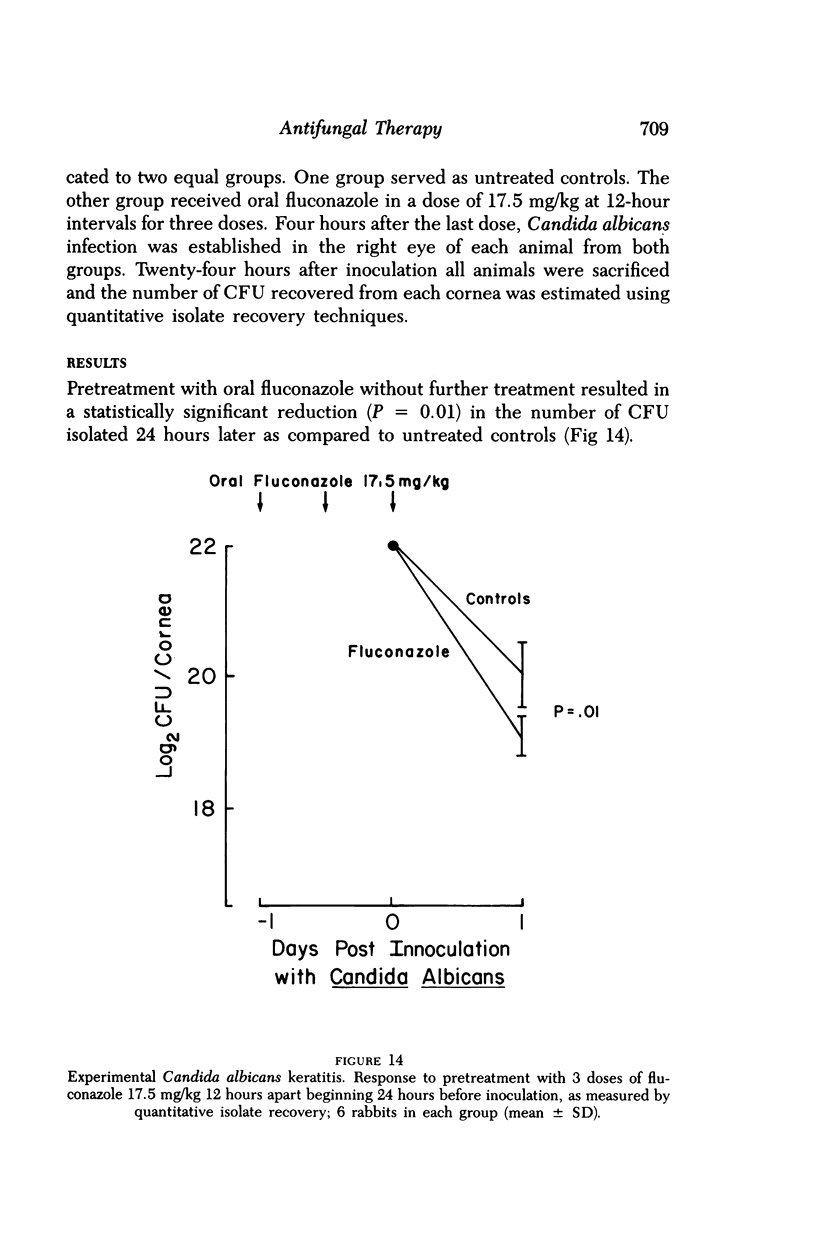
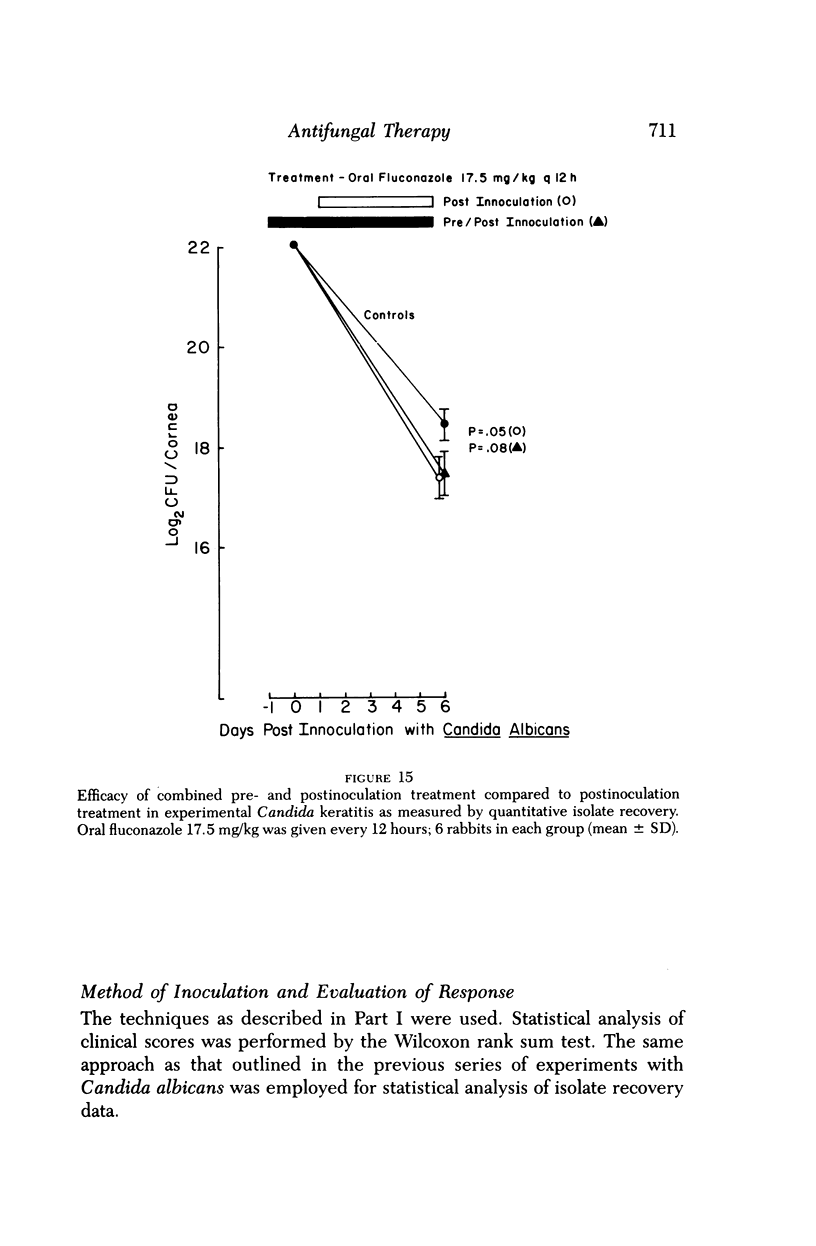
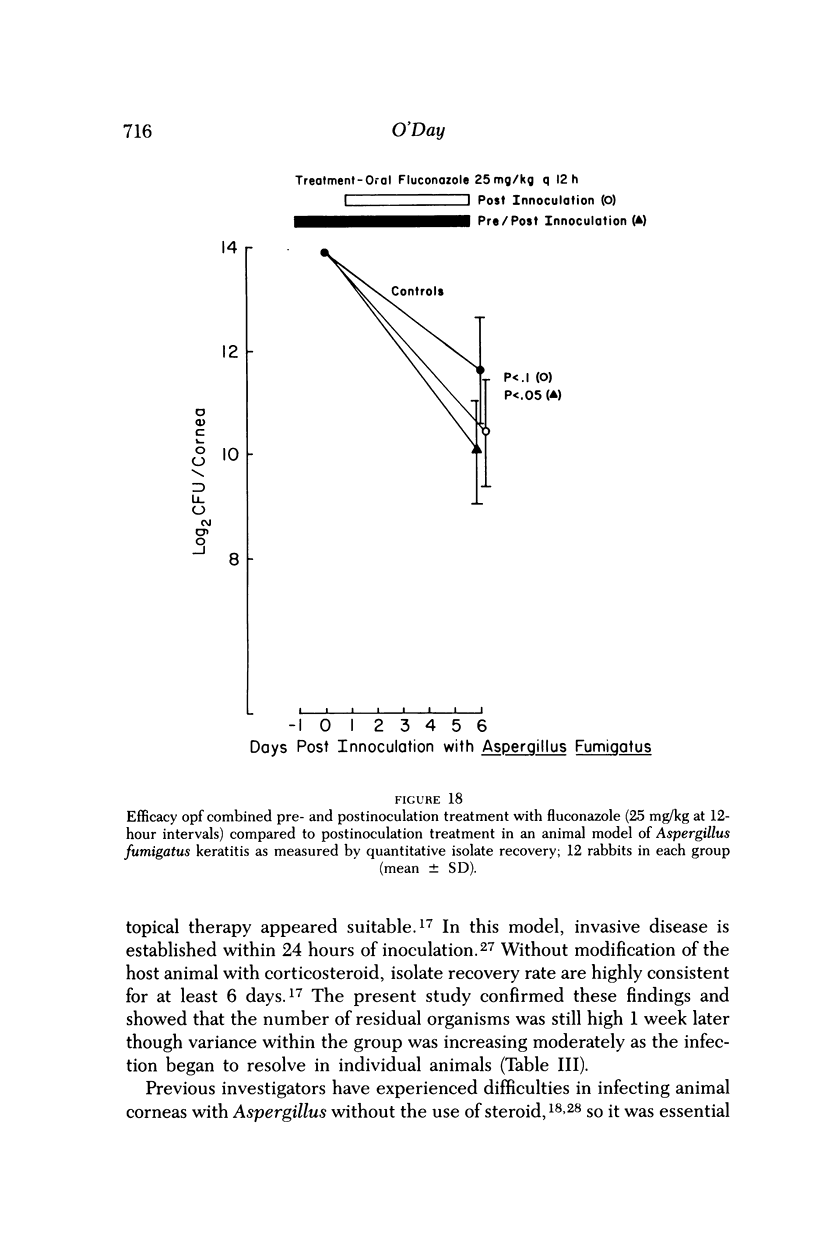
Fluconazole, an experimental azole antifungal agent with good tissue penetration following oral administration, offers the possibility of a new approach to the treatment of keratomycosis. Its efficacy as an orally administered agent was investigated in two models of experimental fungal infection in Dutch-belted rabbits. The study proceeded in three stages. In the first, a model of keratitis due to Aspergillus fumigatus was developed, the suitability of quantitative isolate recovery techniques for the evaluation of the disease caused by this organism was confirmed, and the correlation between the severity of clinical disease scored nonparametrically and the isolate recovery rate was established. The model was found to be most useful for study during the first 5 days of infection. The natural course of experimental Candida alibcans keratitis was evaluated and, on the basis of quantitative isolate recovery techniques, this model was found to be appropriate for studies lasting up to 1 week. In the second stage, corneal uptake following oral administration of fluconazole was studied in Dutch-belted rabbits. The drug was found to readily penetrate the cornea in amounts that correlated with serum levels (R = 0.89). Eight hours following a single 20 mg/kg dose, the corneal level was 7.4 mg/gm, almost double the amount when a 10 mg/kg dose was administered. When given in a twice daily divided dose, fluconazole accumulated steadily in the corneas over a period of 5 days. The presence of inflammation induced by fungal infection did not influence corneal uptake. In the final stage, the efficacy of orally administered fluconazole in the treatment of keratomycosis was evaluated. Overall, a significant therapeutic effect was observed with both infections. Treatment of the animals with oral fluconazole for 1 day prior to inoculation with Candida albicans led to a significant decrease in isolate recovery 1 day later (P = 0.01). However, when treatment was continued for 5 days following inoculation, no additive effect of pretreatment was noted. Pretreatment for 1 day followed by 5 days postinoculation treatment led to a significant decrease in clinical disease (P less than 0.05) and isolate recovery (P = 0.05). A beneficial effect of pretreatment compared to treatment begun 1 day postinoculation, as measured by a reduction in clinical severity and isolate recovery, was also noted. On the basis of these short-term therapeutic studies and the excellent corneal penetration of fluconazole, further investigation of oral therapy of keratomycosis appears warranted.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BURDA C. D., FISHER E., Jr The use of cortisone in establishing experimental fungal keratitis in rats: a preliminary report. Am J Ophthalmol. 1959 Sep;48(3):330–335. [PubMed] [Google Scholar]
- Beggs W. H., Hughes C. E. Exploitation of the direct cell damaging action of antifungal azoles. Diagn Microbiol Infect Dis. 1987 Jan;6(1):1–3. doi: 10.1016/0732-8893(87)90108-8. [DOI] [PubMed] [Google Scholar]
- Davis S. D., Sarff L. D., Hyndiuk R. A. Topical tobramycin therapy of experimental Pseudomonas keratitis: an evaluation of some factors that potentially enhance efficacy. Arch Ophthalmol. 1978 Jan;96(1):123–125. doi: 10.1001/archopht.1978.03910050079020. [DOI] [PubMed] [Google Scholar]
- Dupont B., Drouhet E. Early experience with itraconazole in vitro and in patients: pharmacokinetic studies and clinical results. Rev Infect Dis. 1987 Jan-Feb;9 (Suppl 1):S71–S76. doi: 10.1093/clinids/9.supplement_1.s71. [DOI] [PubMed] [Google Scholar]
- Ellison A. C., Newmark E., Kaufman H. E. Chemotherapy of experimental keratomycosis. Am J Ophthalmol. 1969 Nov;68(5):812–819. doi: 10.1016/0002-9394(69)94573-5. [DOI] [PubMed] [Google Scholar]
- Forster R. K., Rebell G. Animal model of Fusarium solani keratitis. Am J Ophthalmol. 1975 Mar;79(3):510–515. doi: 10.1016/0002-9394(75)90629-7. [DOI] [PubMed] [Google Scholar]
- Foster C. S., Stefanyszyn M. Intraocular penetration of miconazole in rabbits. Arch Ophthalmol. 1979 Sep;97(9):1703–1706. doi: 10.1001/archopht.1979.01020020271017. [DOI] [PubMed] [Google Scholar]
- Foulds G., Brennan D. R., Wajszczuk C., Catanzaro A., Garg D. C., Knopf W., Rinaldi M., Weidler D. J. Fluconazole penetration into cerebrospinal fluid in humans. J Clin Pharmacol. 1988 Apr;28(4):363–366. doi: 10.1002/j.1552-4604.1988.tb03159.x. [DOI] [PubMed] [Google Scholar]
- Garcia de Lomas J., Fons M. A., Nogueira J. M., Rustom F., Borrás R., Buesa F. J. Chemotherapy of Aspergillus fumigatus keratitis: an experimental study. Mycopathologia. 1985 Mar;89(3):135–138. doi: 10.1007/BF00447021. [DOI] [PubMed] [Google Scholar]
- Humphrey M. J., Jevons S., Tarbit M. H. Pharmacokinetic evaluation of UK-49,858, a metabolically stable triazole antifungal drug, in animals and humans. Antimicrob Agents Chemother. 1985 Nov;28(5):648–653. doi: 10.1128/aac.28.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishibashi Y., Matsumoto Y. Intravenous miconazole in the treatment of keratomycosis. Am J Ophthalmol. 1984 May;97(5):646–647. doi: 10.1016/0002-9394(84)90389-1. [DOI] [PubMed] [Google Scholar]
- Ishibashi Y., Matsumoto Y. Intravenous miconazole therapy for experimental keratomycosis in rabbits. Sabouraudia. 1985 Feb;23(1):55–61. doi: 10.1080/00362178585380091. [DOI] [PubMed] [Google Scholar]
- Ishibashi Y., Matsumoto Y. Oral ketoconazole therapy for experimental candida albicans keratitis in rabbits. Sabouraudia. 1984;22(4):323–330. [PubMed] [Google Scholar]
- Ishibashi Y. Oral ketoconazole therapy for keratomycosis. Am J Ophthalmol. 1983 Mar;95(3):342–345. doi: 10.1016/s0002-9394(14)78302-3. [DOI] [PubMed] [Google Scholar]
- Johns K. J., O'Day D. M. Pharmacologic management of keratomycoses. Surv Ophthalmol. 1988 Nov-Dec;33(3):178–188. doi: 10.1016/0039-6257(88)90086-0. [DOI] [PubMed] [Google Scholar]
- Jones D. B. Decision-making in the management of microbial keratitis. Ophthalmology. 1981 Aug;88(8):814–820. doi: 10.1016/s0161-6420(81)34943-4. [DOI] [PubMed] [Google Scholar]
- Jones D. B., Forster F. K., Rebell G. Fusarium solani keratitis treated with natamycin (pimaricin): eighteen consecutive cases. Arch Ophthalmol. 1972 Aug;88(2):147–154. doi: 10.1001/archopht.1972.01000030149004. [DOI] [PubMed] [Google Scholar]
- Komadina T. G., Wilkes T. D., Shock J. P., Ulmer W. C., Jackson J., Bradsher R. W. Treatment of Aspergillus fumigatus keratitis in rabbits with oral and topical ketoconazole. Am J Ophthalmol. 1985 Apr 15;99(4):476–479. doi: 10.1016/0002-9394(85)90017-0. [DOI] [PubMed] [Google Scholar]
- Kupferman A., Leibowitz H. M. Quantitation of bacterial infection and antibiotic effect in the cornea. Arch Ophthalmol. 1976 Nov;94(11):1981–1984. doi: 10.1001/archopht.1976.03910040687017. [DOI] [PubMed] [Google Scholar]
- LEY A. P. Experimental fungus infections of the cornea; a preliminary report. Am J Ophthalmol. 1956 Oct;42(4 Pt 2):59–71. doi: 10.1016/0002-9394(56)90356-7. [DOI] [PubMed] [Google Scholar]
- Leibowitz H. M., Kupferman A. Topically administered corticosteroids: effect on antibiotic-treated bacterial keratitis. Arch Ophthalmol. 1980 Jul;98(7):1287–1290. doi: 10.1001/archopht.1980.01020040139024. [DOI] [PubMed] [Google Scholar]
- Newmark E., Ellison A. C., Kaufman H. E. Combined pimaricin and dexamethasone therapy of keratomycosis. Am J Ophthalmol. 1971 Mar;71(3):718–722. doi: 10.1016/0002-9394(71)90434-x. [DOI] [PubMed] [Google Scholar]
- O'Day D. M., Ray W. A., Head W. S., Robinson R. D. Influence of the corneal epithelium on the efficacy of topical antifungal agents. Invest Ophthalmol Vis Sci. 1984 Jul;25(7):855–859. [PubMed] [Google Scholar]
- O'Day D. M., Ray W. A., Robinson R. D., Head W. S. Correlation of in vitro and in vivo susceptibility of Candida albicans to amphotericin B and natamycin. Invest Ophthalmol Vis Sci. 1987 Mar;28(3):596–603. [PubMed] [Google Scholar]
- O'Day D. M., Ray W. A., Robinson R. D., Head W. S., Savage A. M. The influence of yeast growth phase in vivo on the efficacy of topical polyenes. Curr Eye Res. 1987 Feb;6(2):363–368. doi: 10.3109/02713688709025189. [DOI] [PubMed] [Google Scholar]
- O'Day D. M., Robinson R., Head W. S. Efficacy of antifungal agents in the cornea. I. A comparative study. Invest Ophthalmol Vis Sci. 1983 Aug;24(8):1098–1102. [PubMed] [Google Scholar]
- O'Day D. M. Selection of appropriate antifungal therapy. Cornea. 1987;6(4):238–245. doi: 10.1097/00003226-198706040-00002. [DOI] [PubMed] [Google Scholar]
- Odds F. C., Cheesman S. L., Abbott A. B. Antifungal effects of fluconazole (UK 49858), a new triazole antifungal, in vitro. J Antimicrob Chemother. 1986 Oct;18(4):473–478. doi: 10.1093/jac/18.4.473. [DOI] [PubMed] [Google Scholar]
- Ohno S., Fuerst D. J., Okumoto M., Grabner G., Smolin G. The effect of K-582, a new antifungal agent, on experimental Candida keratitis. Invest Ophthalmol Vis Sci. 1983 Dec;24(12):1626–1629. [PubMed] [Google Scholar]
- Oji E. O. Development of quantitative methods of measuring antifungal drug effects in the rabbit cornea. Br J Ophthalmol. 1981 Feb;65(2):89–96. doi: 10.1136/bjo.65.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palou de Fernandez E., Patino M. M., Graybill J. R., Tarbit M. H. Treatment of cryptococcal meningitis in mice with fluconazole. J Antimicrob Chemother. 1986 Aug;18(2):261–270. doi: 10.1093/jac/18.2.261. [DOI] [PubMed] [Google Scholar]
- Ray W. A., O'Day D. M., Head W. S., Robinson R. Statistical analysis for experimental models of ocular disease: continuous response measures. Curr Eye Res. 1985 May;4(5):585–597. doi: 10.3109/02713688508999990. [DOI] [PubMed] [Google Scholar]
- Richards A. B., Jones B. R., Whitwell J., Clayton Y. M. Corneal and intra-ocular infection by Candida albicans treated with 5-fluorocytosine. Trans Ophthalmol Soc U K. 1970;89:867–885. [PubMed] [Google Scholar]
- Richardson K., Brammer K. W., Marriott M. S., Troke P. F. Activity of UK-49,858, a bis-triazole derivative, against experimental infections with Candida albicans and Trichophyton mentagrophytes. Antimicrob Agents Chemother. 1985 May;27(5):832–835. doi: 10.1128/aac.27.5.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers T. E., Galgiani J. N. Activity of fluconazole (UK 49,858) and ketoconazole against Candida albicans in vitro and in vivo. Antimicrob Agents Chemother. 1986 Sep;30(3):418–422. doi: 10.1128/aac.30.3.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern G. A., Okumoto M., Smolin G. Combined amphotericin B and rifampin treatment of experimental Candida albicans keratitis. Arch Ophthalmol. 1979 Apr;97(4):721–722. doi: 10.1001/archopht.1979.01020010373020. [DOI] [PubMed] [Google Scholar]
- Thomas P. A., Abraham D. J., Kalavathy C. M., Rajasekaran J. Oral itraconazole therapy for mycotic keratitis. Mycoses. 1988 May;31(5):271–279. doi: 10.1111/j.1439-0507.1988.tb03986.x. [DOI] [PubMed] [Google Scholar]
- Troke P. F., Andrews R. J., Brammer K. W., Marriott M. S., Richardson K. Efficacy of UK-49,858 (fluconazole) against Candida albicans experimental infections in mice. Antimicrob Agents Chemother. 1985 Dec;28(6):815–818. doi: 10.1128/aac.28.6.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troke P. F., Andrews R. J., Marriott M. S., Richardson K. Efficacy of fluconazole (UK-49,858) against experimental aspergillosis and cryptococcosis in mice. J Antimicrob Chemother. 1987 May;19(5):663–670. doi: 10.1093/jac/19.5.663. [DOI] [PubMed] [Google Scholar]
- Van Cutsem J., Van Gerven F., Janssen P. A. Activity of orally, topically, and parenterally administered itraconazole in the treatment of superficial and deep mycoses: animal models. Rev Infect Dis. 1987 Jan-Feb;9 (Suppl 1):S15–S32. doi: 10.1093/clinids/9.supplement_1.s15. [DOI] [PubMed] [Google Scholar]