Abstract
Patients with nanophthalmos are prone to develop a chronic painless type of glaucoma in middle age, probably due to the natural increase in the size of the lens which is already relatively too large for the small eye. Although the underlying mechanism is obscure, a slowly progressive "creeping" chronic angle-closure is postulated, but gonioscopic evaluation is difficult due to the shallow anterior chamber, with grade I and slit angles. Response to medical treatment is poor and miotics may even make the condition worse by producing relative pupillary block and by relaxing the lens zonule. Ordinary glaucoma surgery is to be avoided in nanophthalmos because of the fear of postoperative ciliary-block malignant glaucoma. Periopheral iridectomy performed in five eyes at an advanced stage of the chronic angle-closure did not facilitate glaucoma control in three eyes, and in two eyes in which the operation was combined with posterior sclerotomy, the eyes became blind from vitreous hemorrhage. Lenx extraction in five eyes controlled the glaucoma but was followed by choroidal effusion and nonrhegmatogenous retinal detachements in two eyes and blindness in another eye when combined with a posterior sclerotomy. No firm therapeutic recommendations can be made on the basis of the author's experience in the six reported cases. Conventional medical therapy seems ineffectual even when begun early in the glaucoma. Conventional glaucoma surgery must be performed early, before permanent damage to the outflow mechanism occurs but removal of the lens must be anticipated. The surgeon must also remain aware of the high incidence of serious posterior-segment complications which inexplicably follow glaucoma or lens surgery in nanophthalmos, as described by Brockhurst.
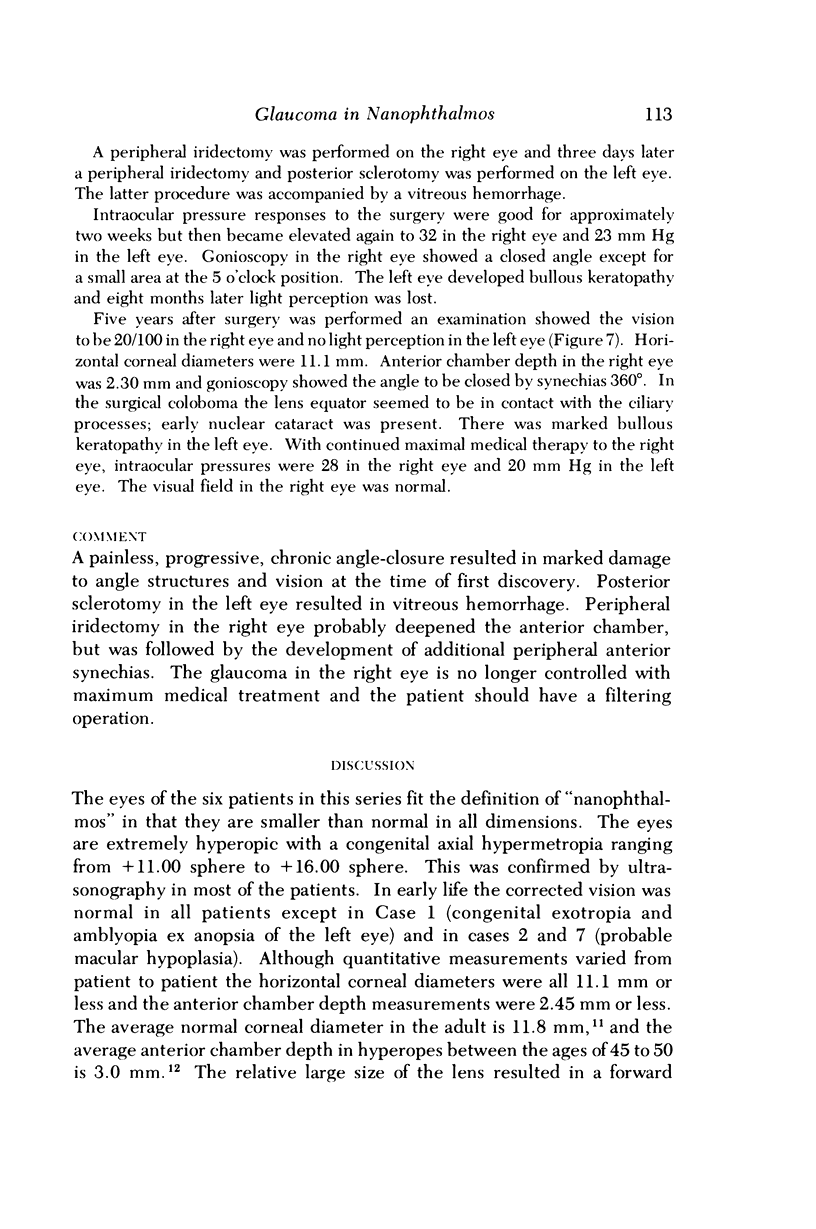
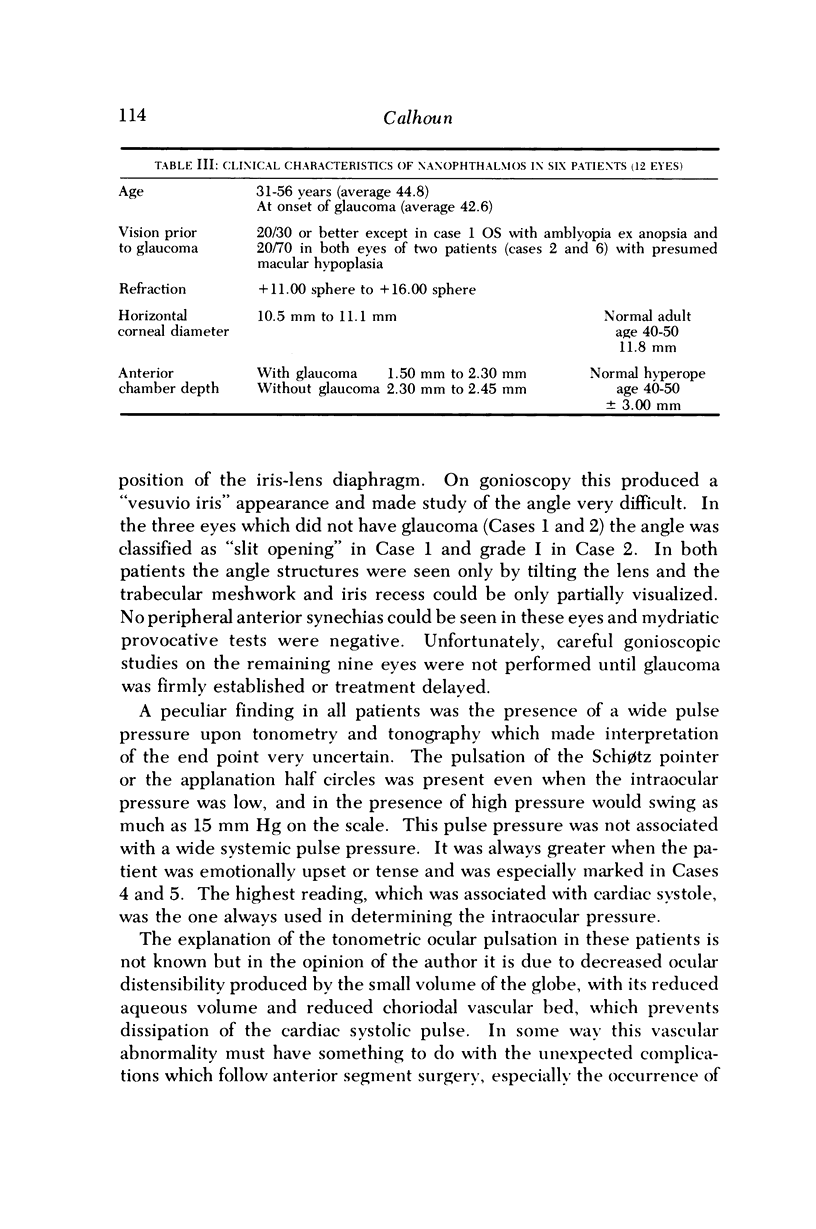
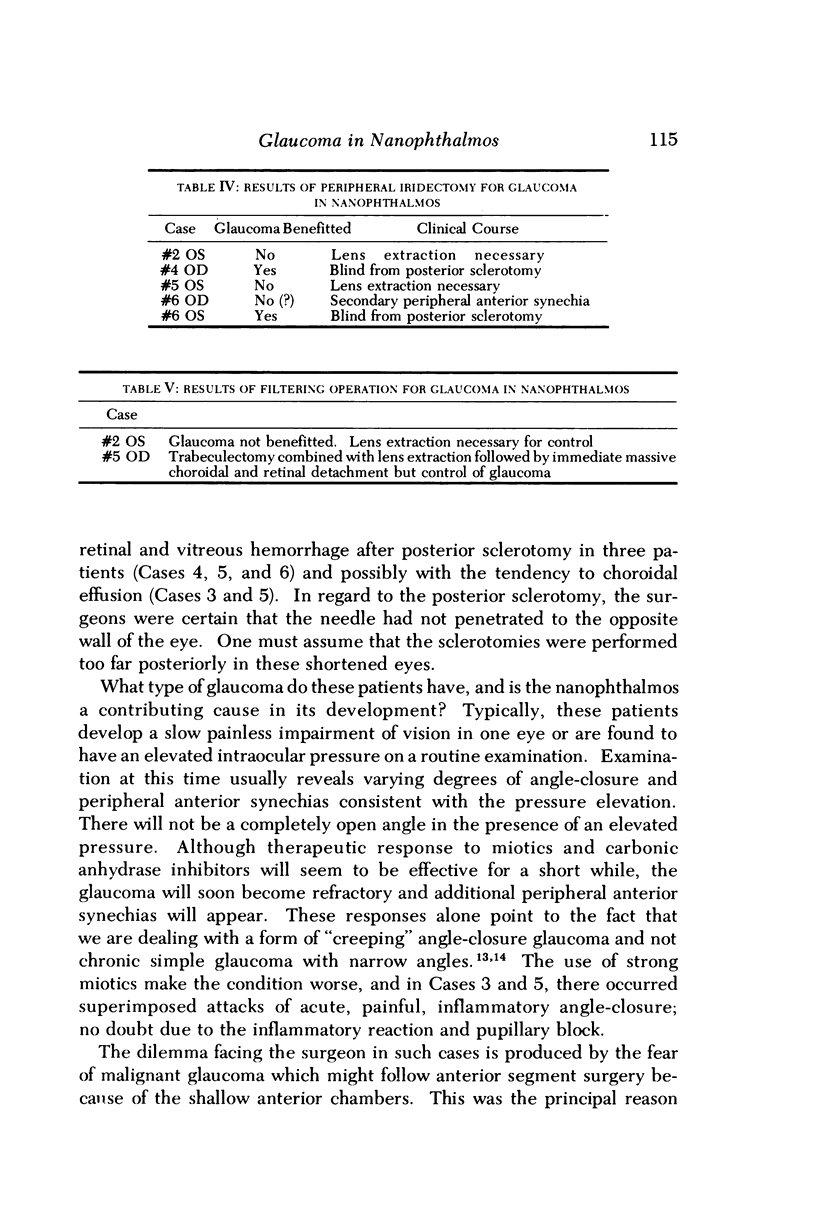
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brockhurst R. J., Lam K. W. Uveal effusion. II. Report of a case with analysis of subretinal fluid. Arch Ophthalmol. 1973 Nov;90(5):399–401. doi: 10.1001/archopht.1973.01000050401015. [DOI] [PubMed] [Google Scholar]
- Brockhurst R. J. Nanophthalmos with uveal effusion: a new clinical entity. Trans Am Ophthalmol Soc. 1974;72:371–403. [PMC free article] [PubMed] [Google Scholar]
- CALMETTES, DEODATI, HURON, BECHAC Etude de la profondeur de la chambre antérieure: variations physiologiques et au cours des amétropies. Arch Ophtalmol Rev Gen Ophtalmol. 1958 Jul-Aug;18(5):513–542. [PubMed] [Google Scholar]
- HATCHER W. F. Extreme axial hyperopia. AMA Arch Ophthalmol. 1952 Aug;48(2):161–162. doi: 10.1001/archopht.1952.00920010166006. [DOI] [PubMed] [Google Scholar]
- HERMANN P. Le syndrome microphtalmie-rétinite pigmentaire-glaucome. Arch Ophtalmol Rev Gen Ophtalmol. 1958 Jan-Feb;18(1):17–24. [PubMed] [Google Scholar]
- LOWE R. F. PRIMARY CREEPING ANGLE-CLOSURE GLAUCOMA. Br J Ophthalmol. 1964 Oct;48:544–550. doi: 10.1136/bjo.48.10.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Grady R. B. Nanophthalmos. Am J Ophthalmol. 1971 Jun;71(6):1251–1253. doi: 10.1016/0002-9394(71)90971-8. [DOI] [PubMed] [Google Scholar]
- Pollack I. P. Chronic angle-closure glaucoma; diagnosis and treatment in patients with angles that appear open. Arch Ophthalmol. 1971 Jun;85(6):676–689. doi: 10.1001/archopht.1971.00990050678006. [DOI] [PubMed] [Google Scholar]
- SCAMMON R. E., WILMER H. A. Growth of the components of the human eyeball; II. Comparison of the calculated volumes of the eyes of the newborn and of adults, and their components. Arch Ophthal. 1950 Apr;43(4):620–637. doi: 10.1001/archopht.1950.00910010631002. [DOI] [PubMed] [Google Scholar]
- SCHEPENS C. L., BROCKHURST R. J. UVEAL EFFUSION. 1. CLINICAL PICTURE. Arch Ophthalmol. 1963 Aug;70:189–201. doi: 10.1001/archopht.1963.00960050191010. [DOI] [PubMed] [Google Scholar]
- Wilkie J., Drance S. M., Schulzer M. The effects of miotics on anterior-chamber depth. Am J Ophthalmol. 1969 Jul;68(1):78–83. doi: 10.1016/0002-9394(69)94936-8. [DOI] [PubMed] [Google Scholar]