Abstract
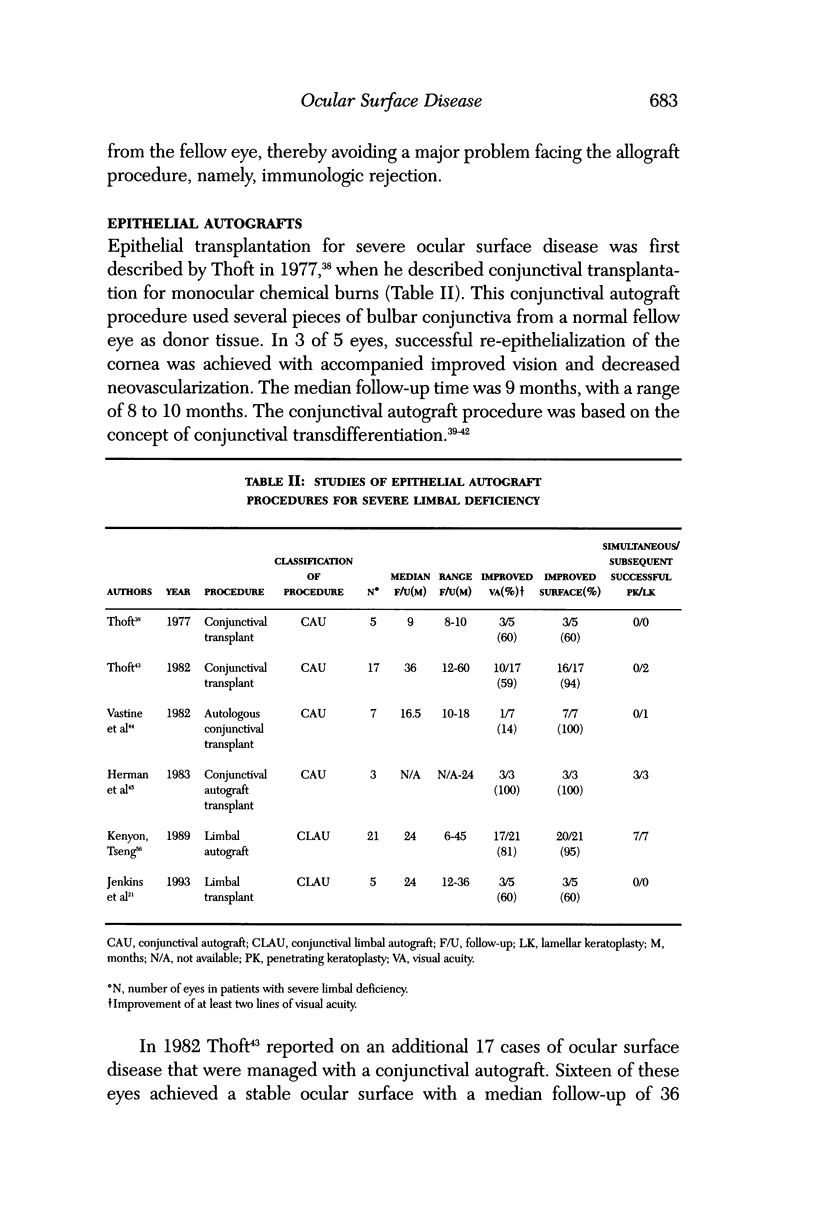
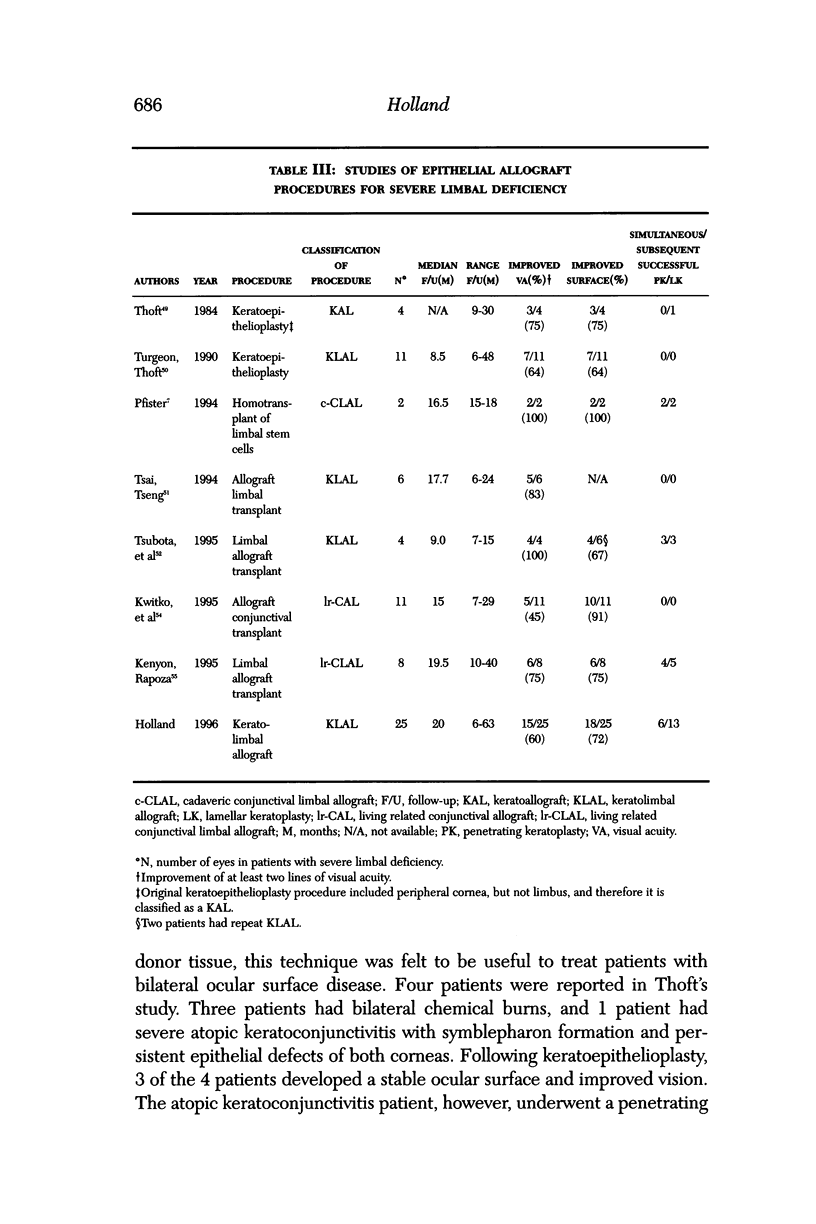
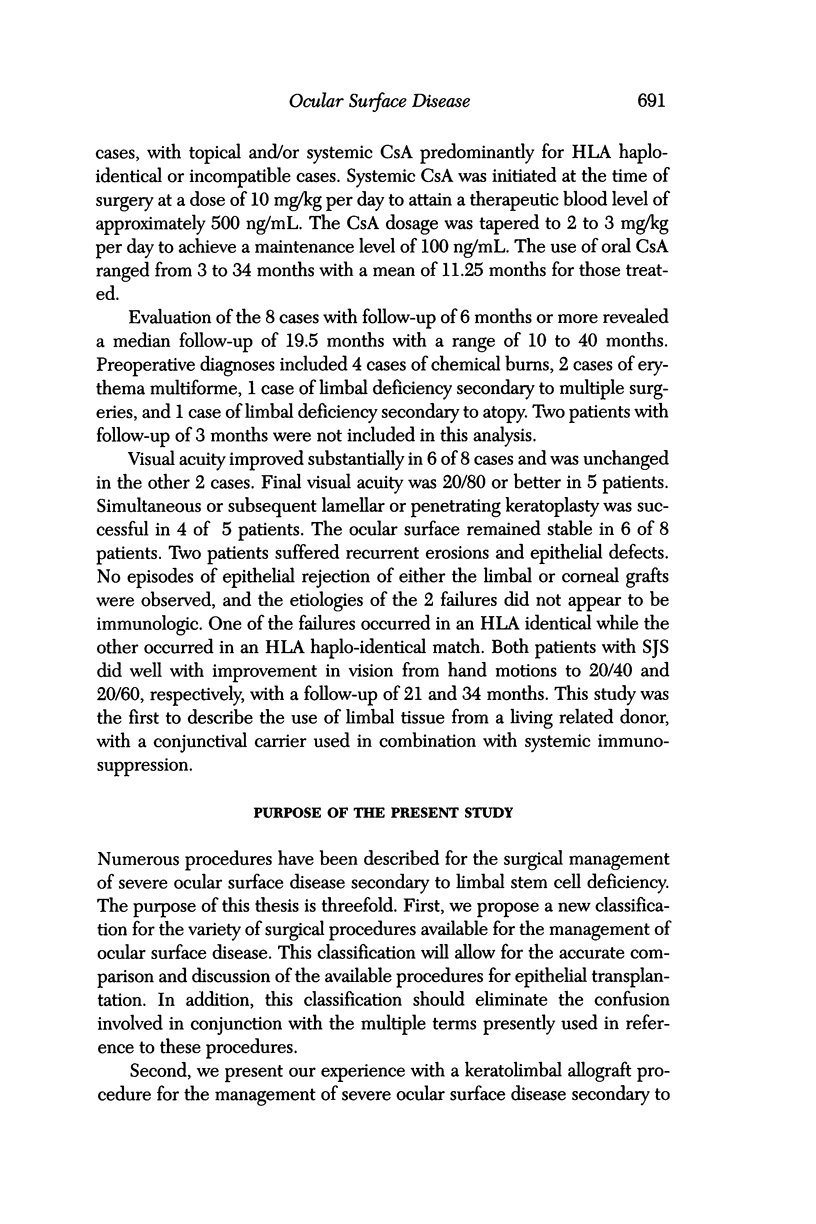
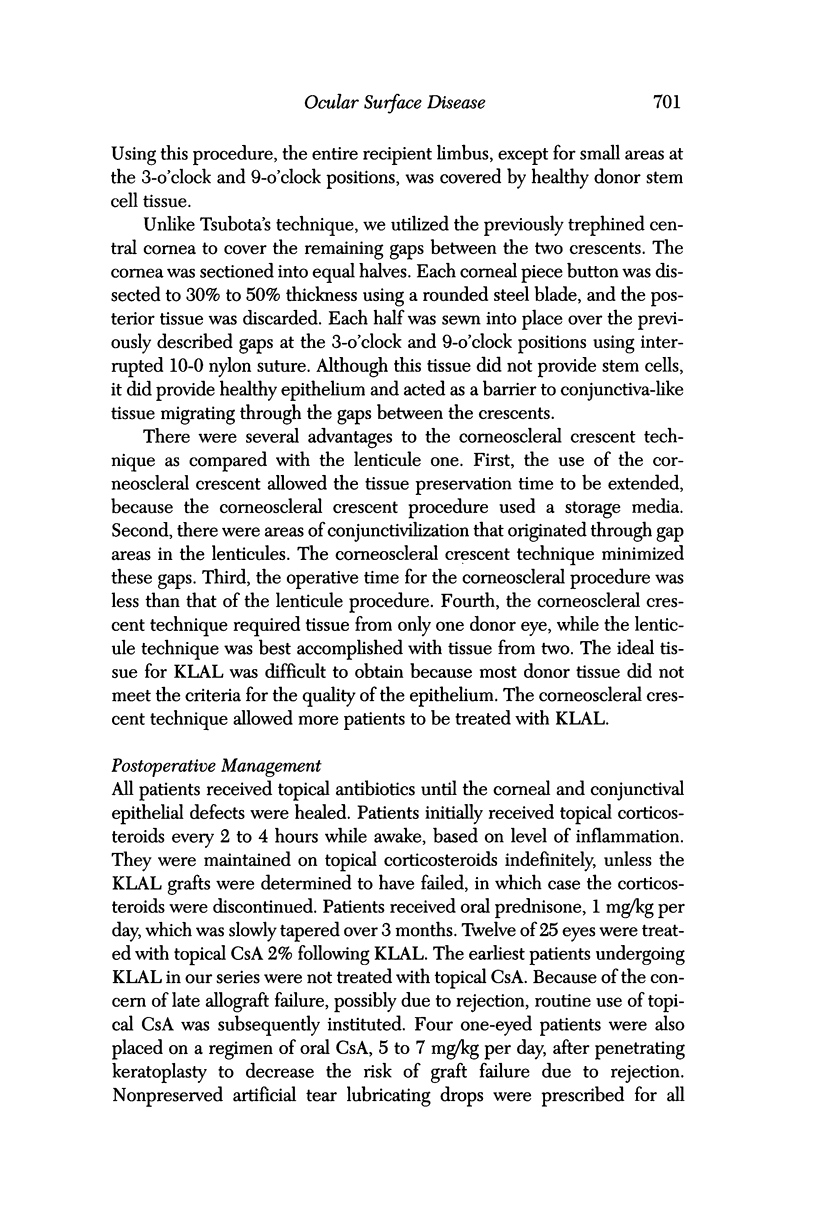
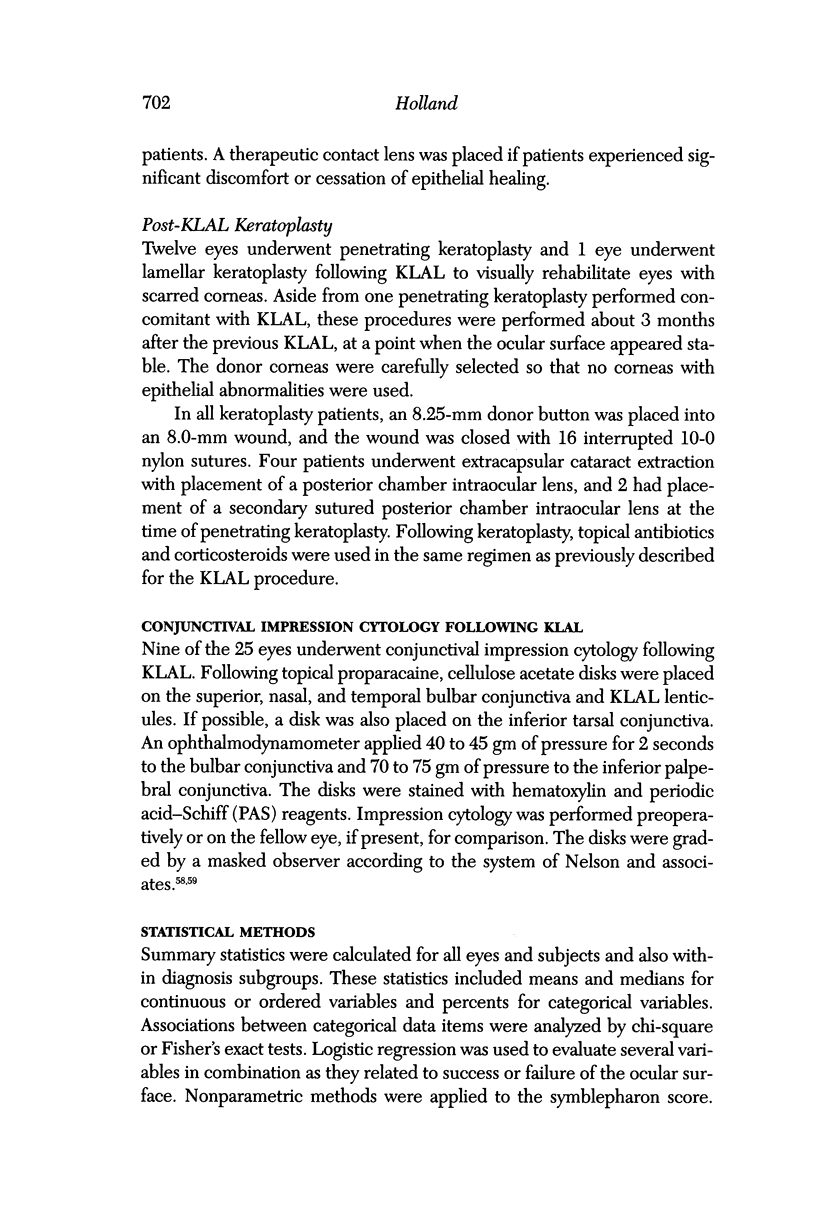
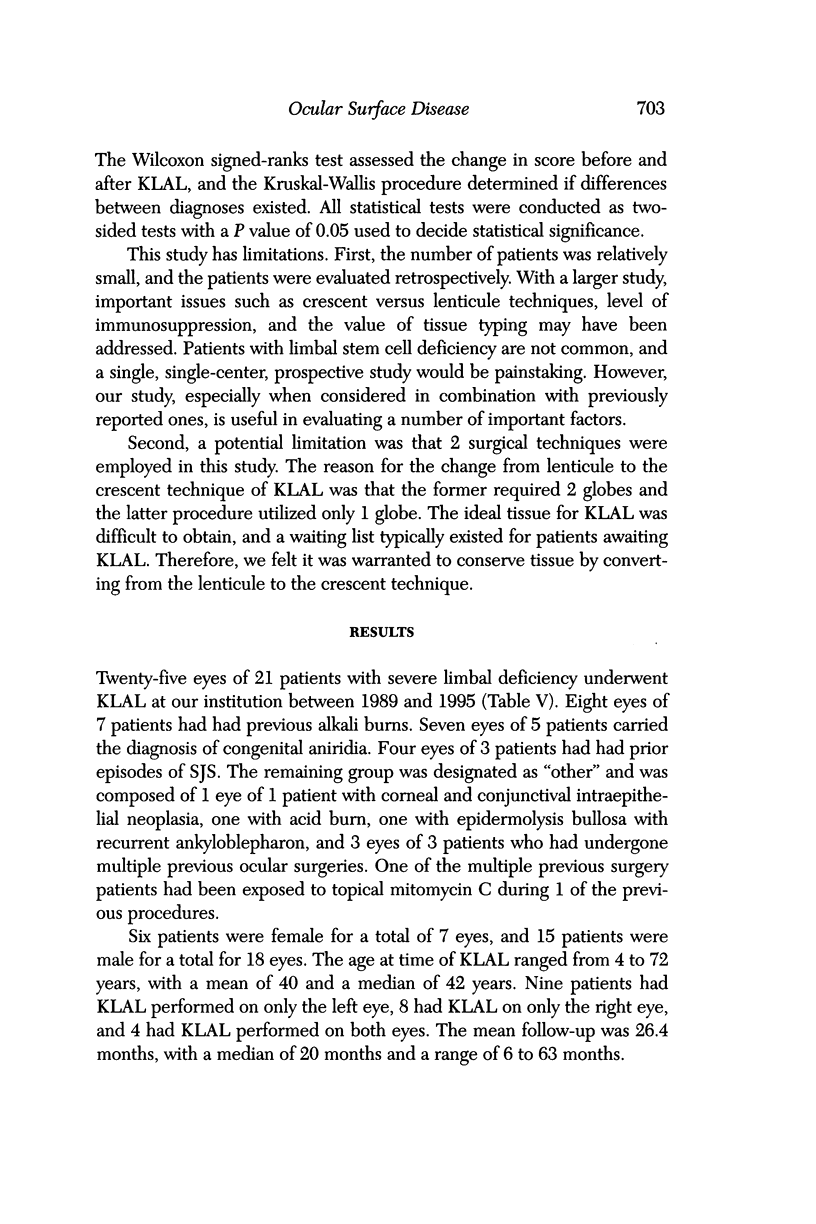
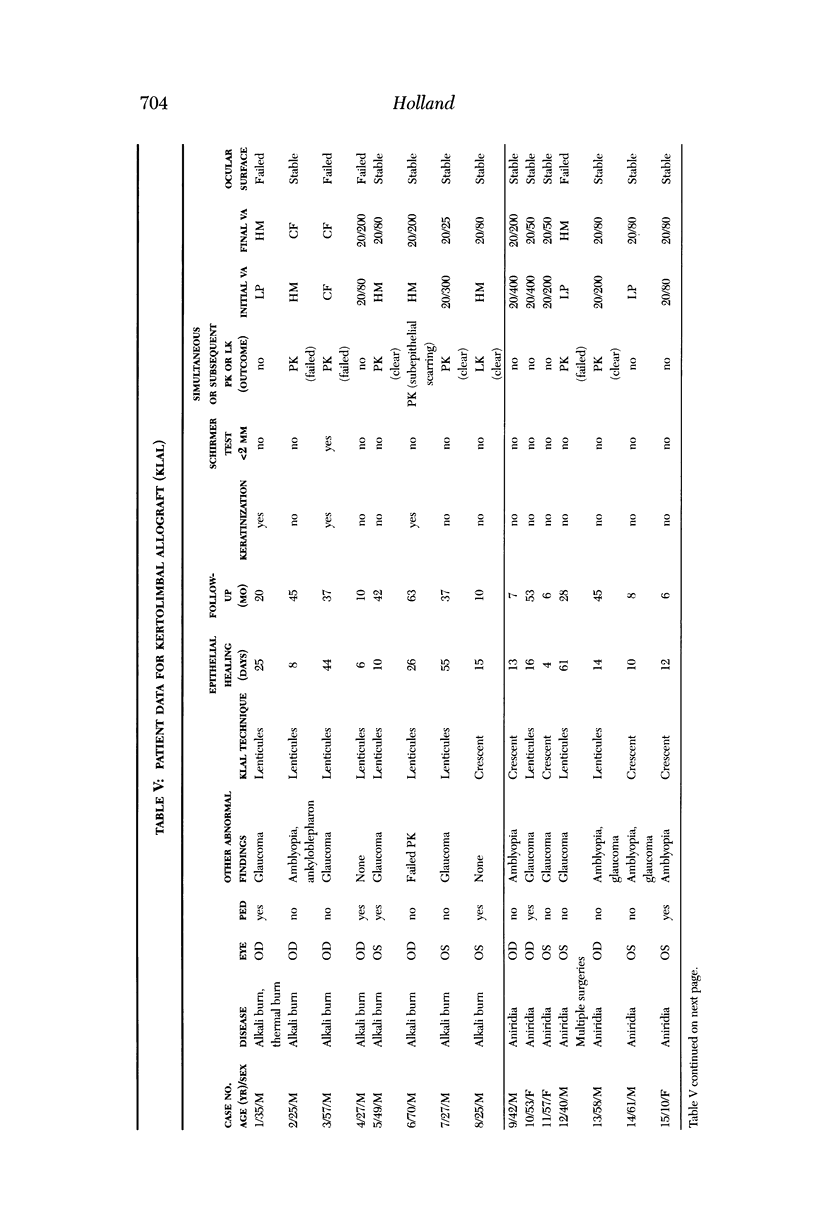
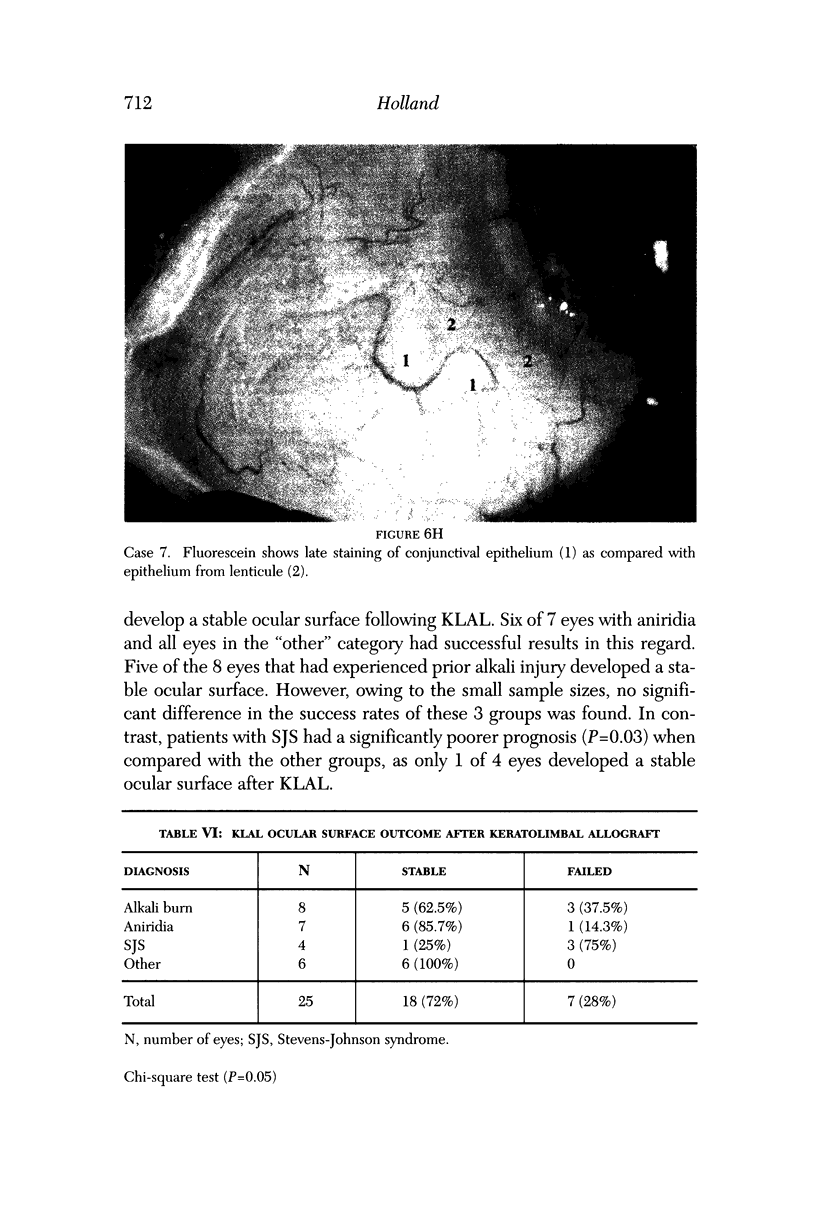
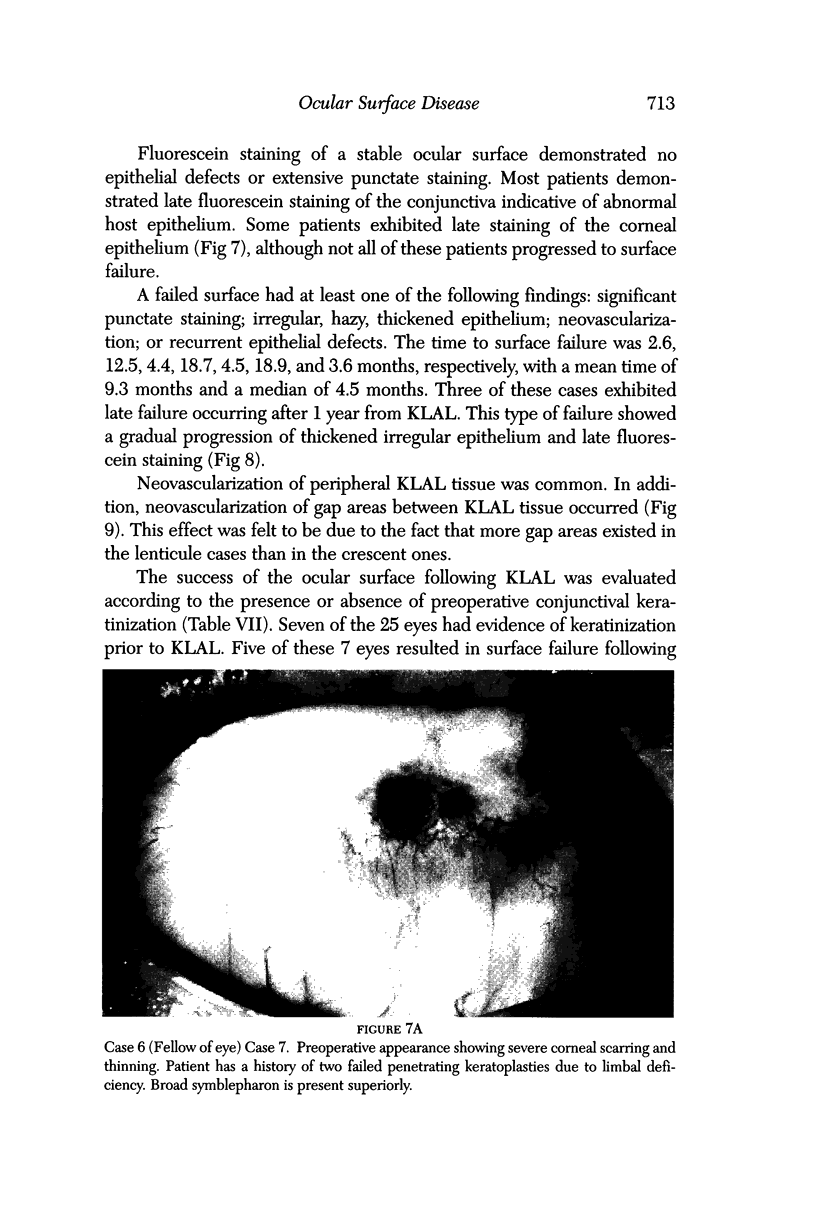
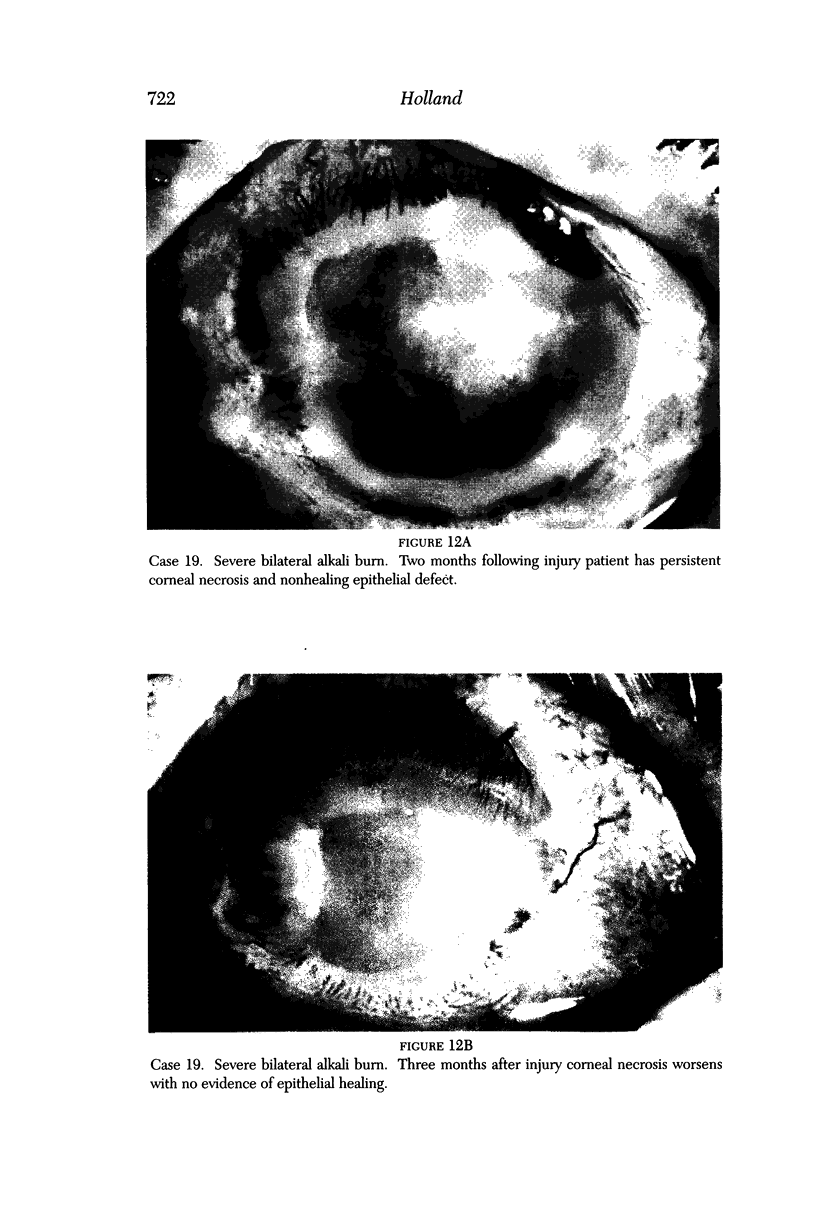
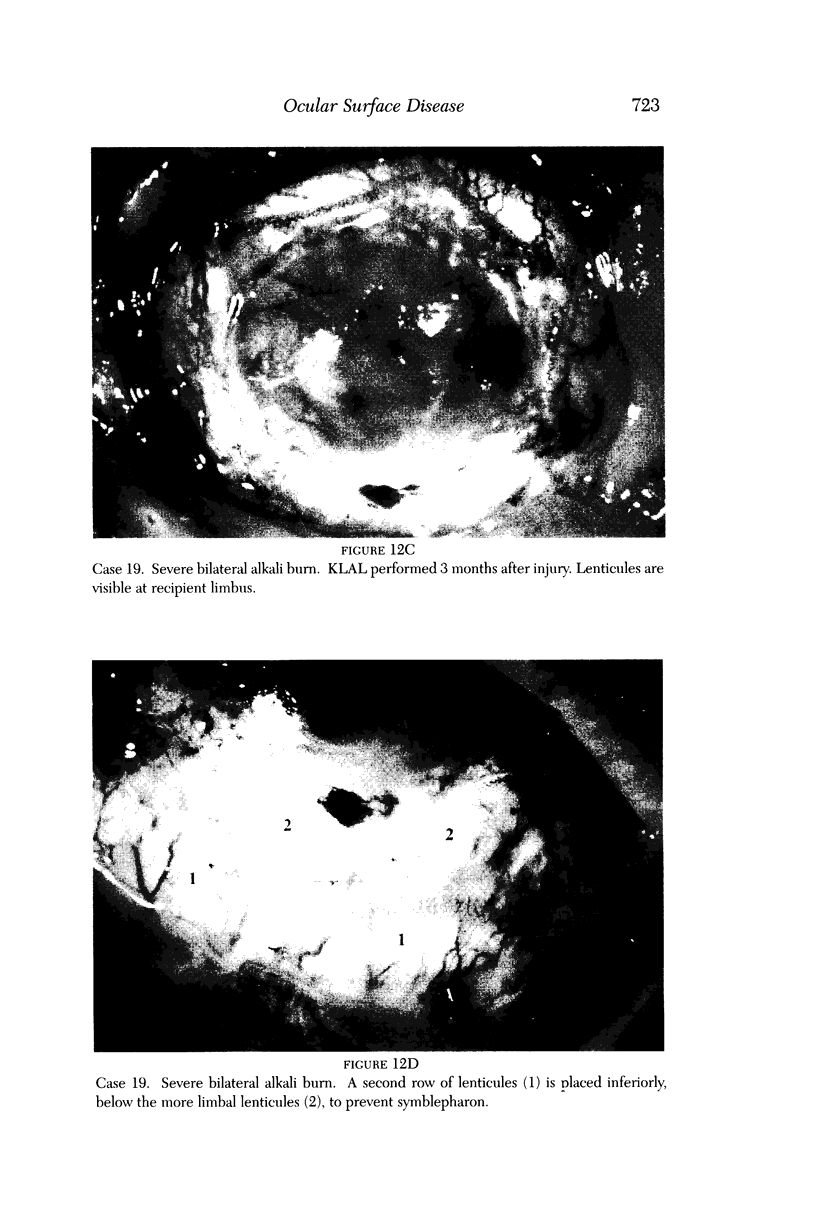
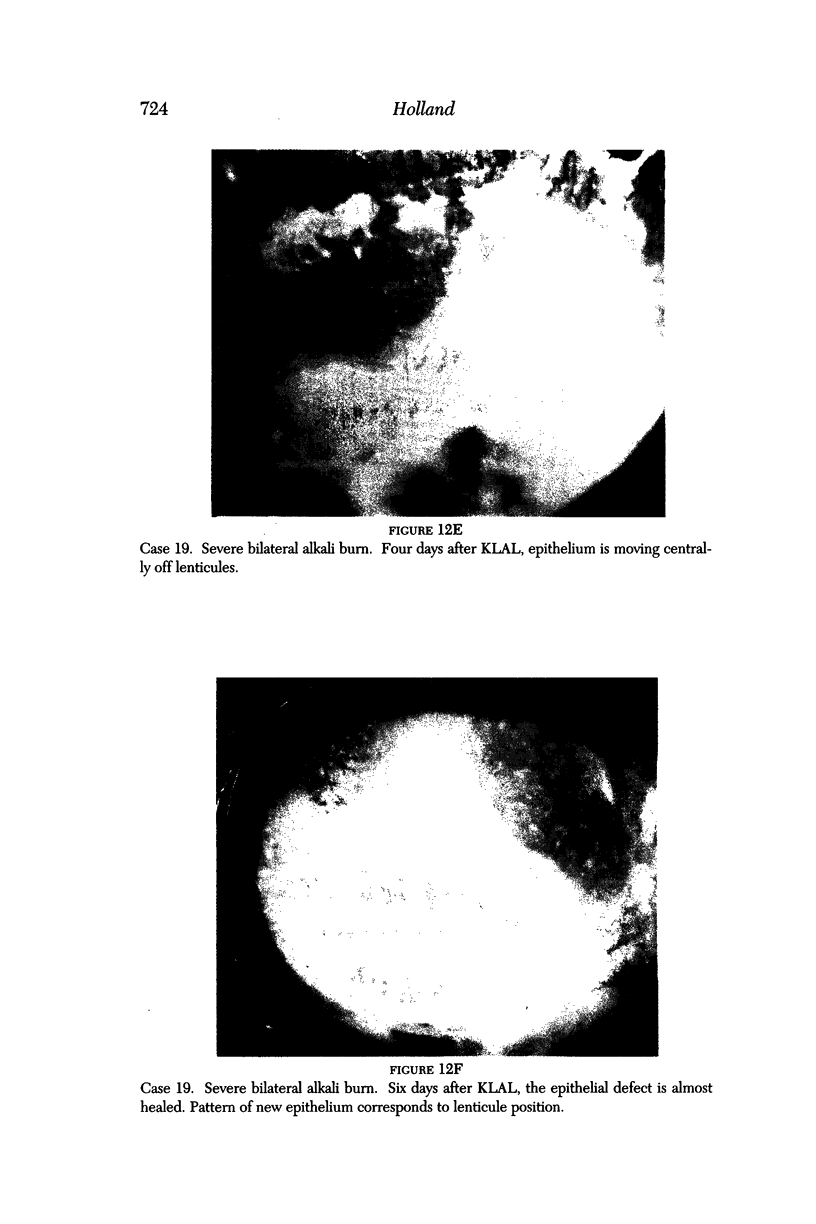
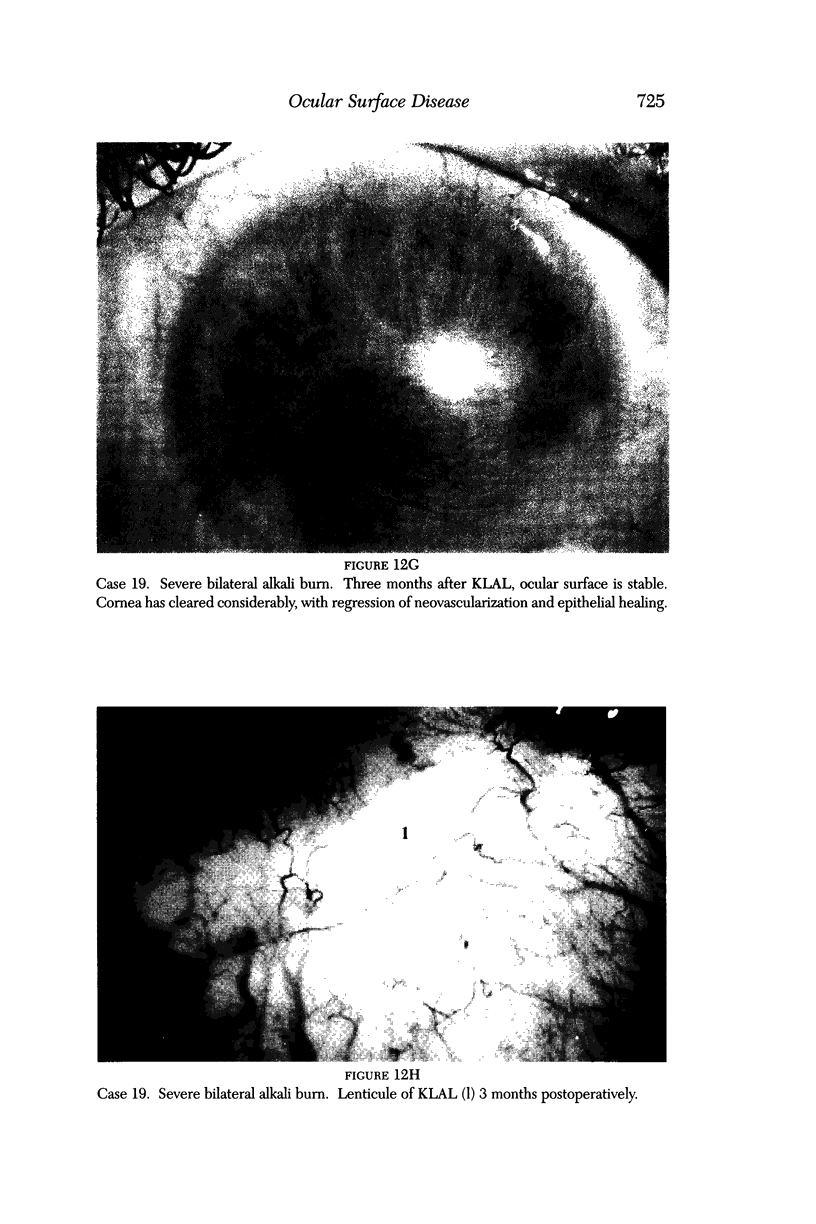
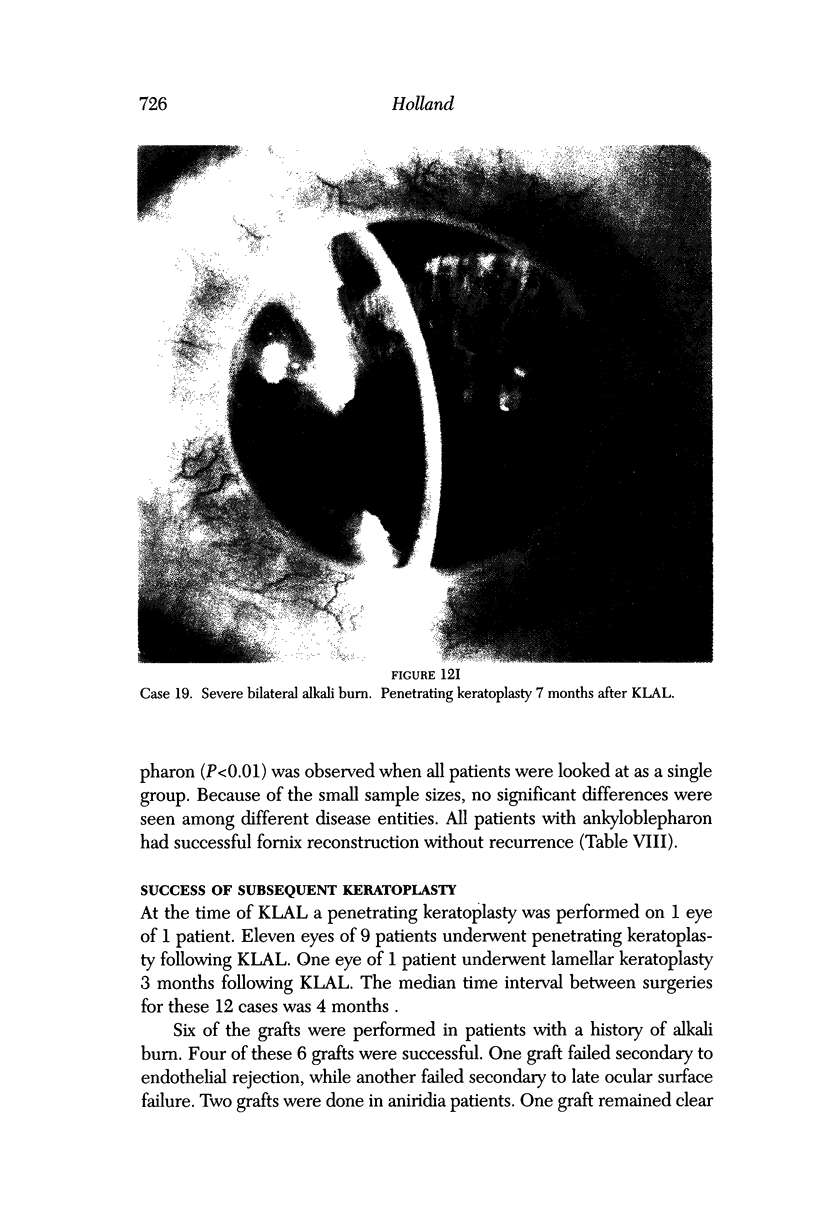
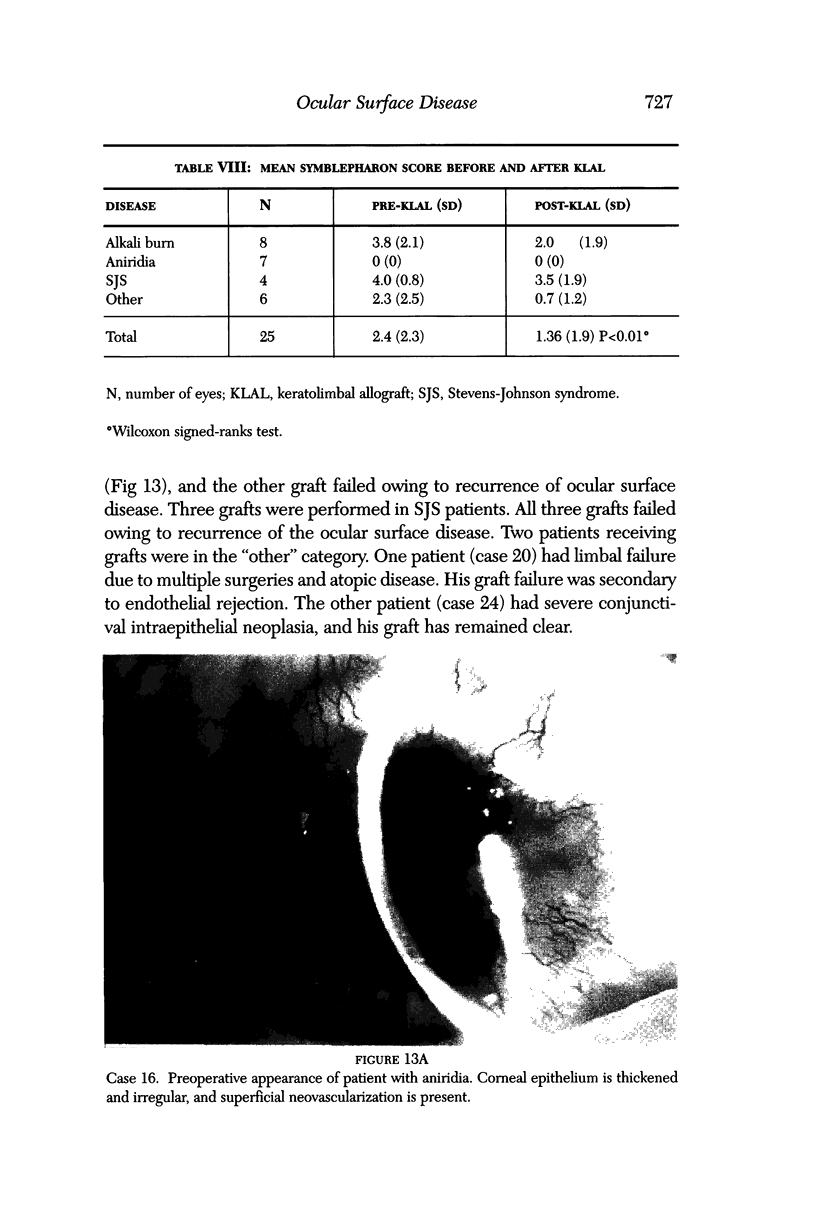
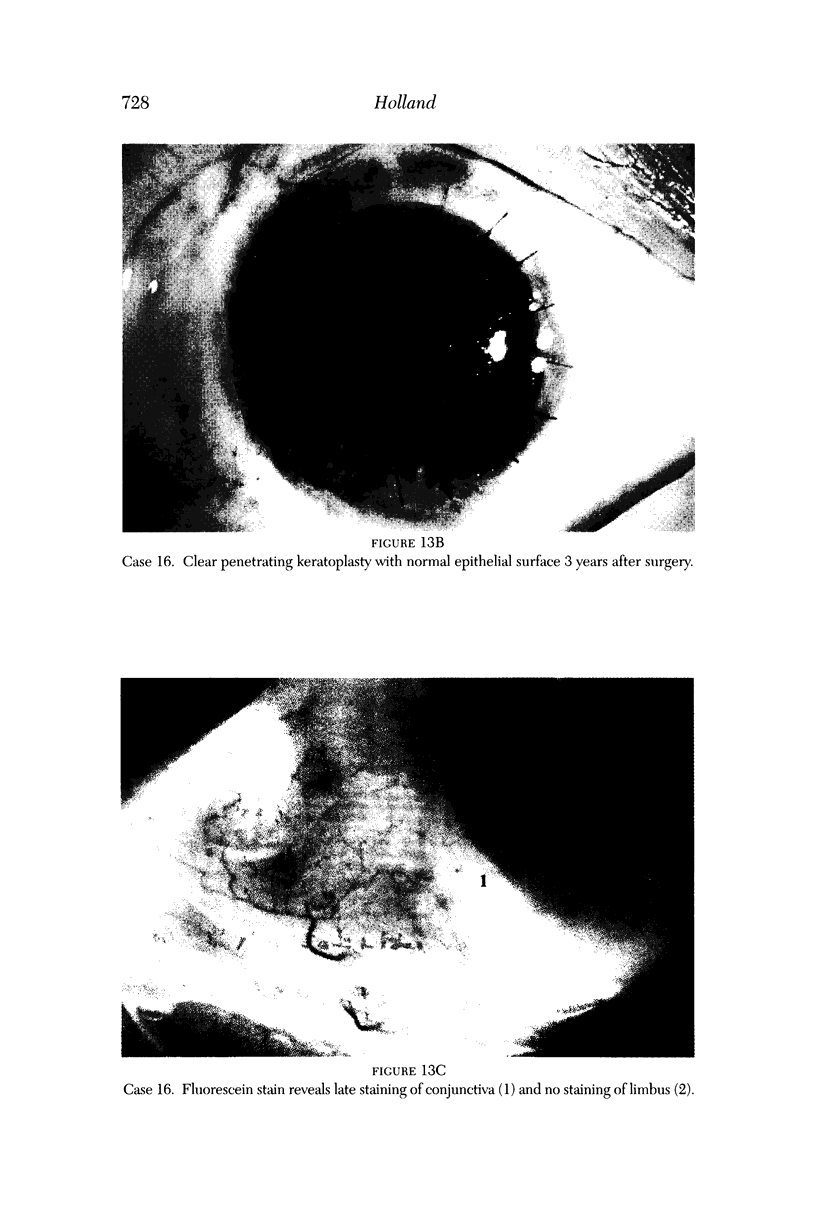
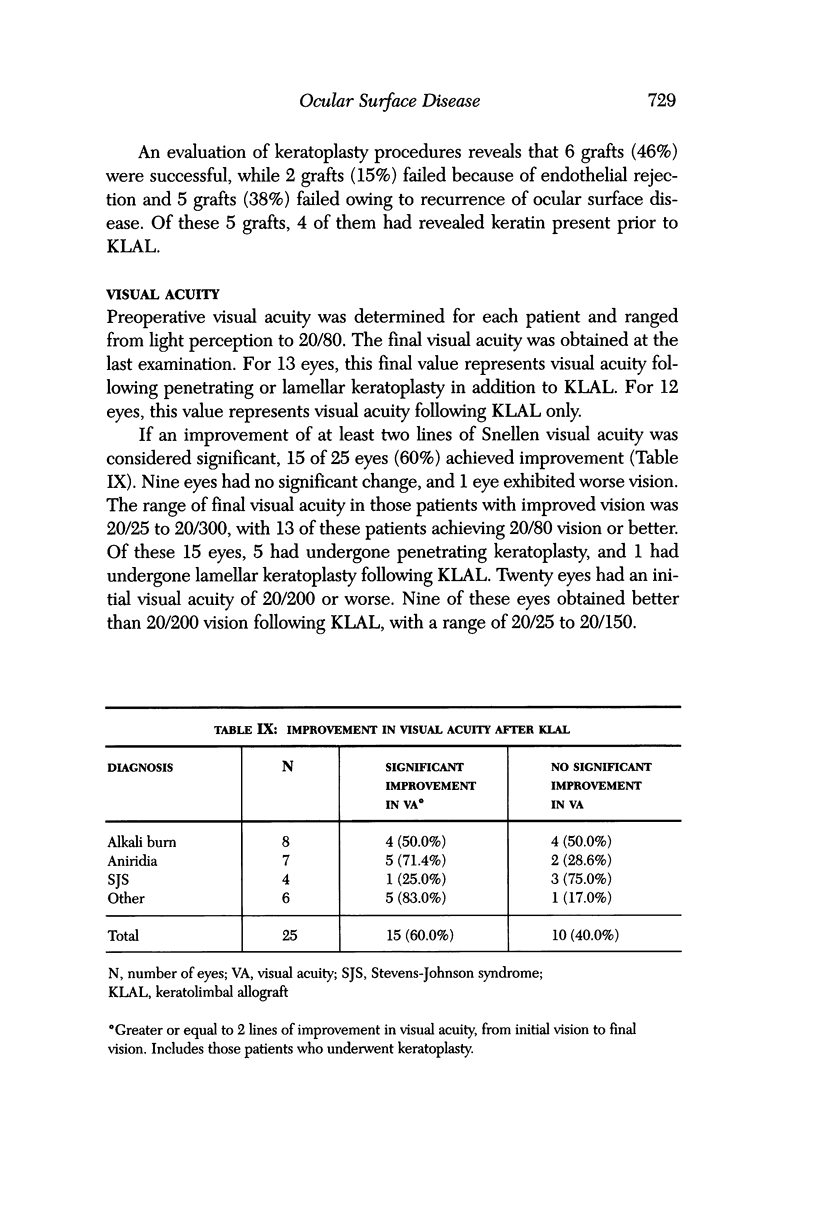
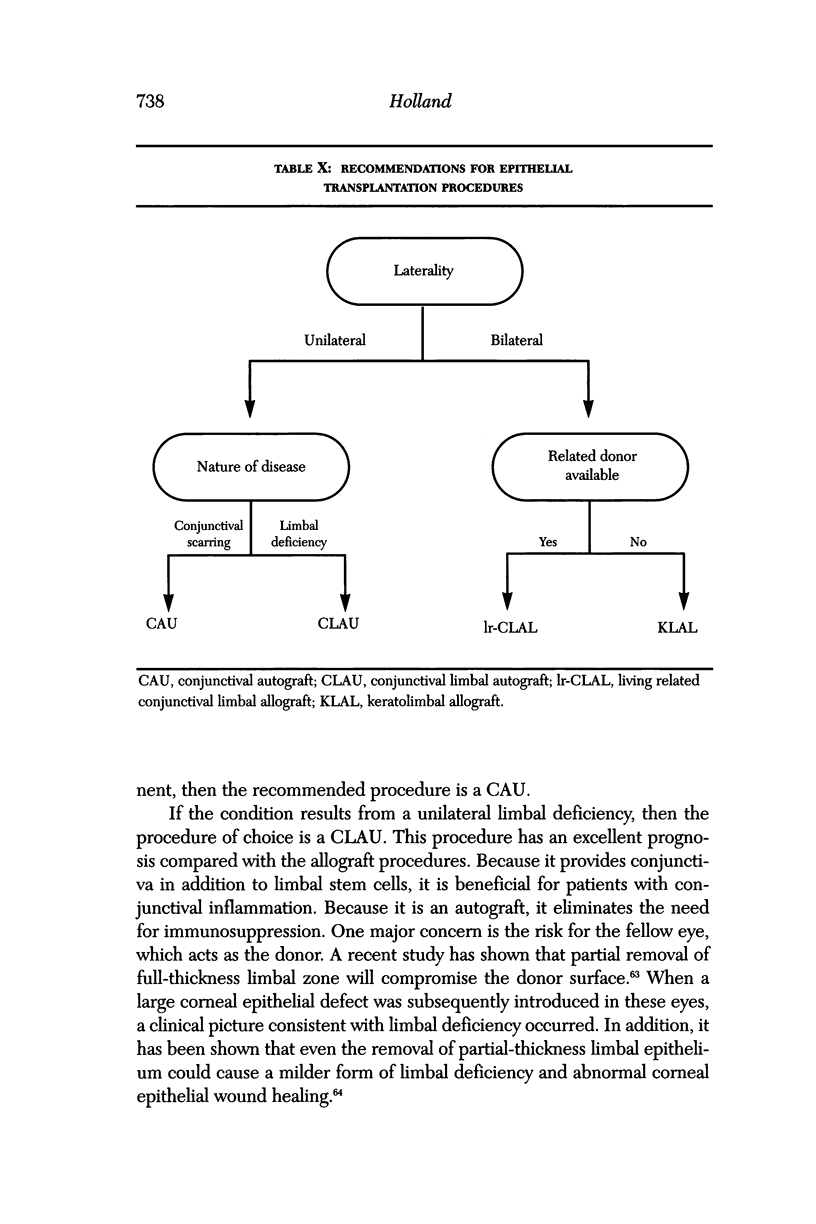
PURPOSE: First, to present a new classification of epithelial transplantation procedures for ocular surface disease; second, to present our experience with a keratolimbal allograft procedure for limbal stem cell deficiency; and third, to make recommendations for the indications and postoperative management of epithelial transplantation procedures. METHODS: A review of all epithelial transplantation procedures was performed. A classification of these procedures based on the source of donor tissue and the tissue transplanted was proposed. In addition, a review of 25 eyes of 21 patients who underwent a keratolimbal allograft was completed. Ocular surface stability, improvement of visual acuity, success of subsequent keratoplasties, and preoperative risk factors were evaluated. Results were compared with those of other epithelial transplantation procedures for ocular surface disease. On the basis of the results of published studies, as well as ours, a recommendation for the indication of the various procedures was made. RESULTS: Epithelial transplantation for ocular surface disease can be classified as one of the following procedures: conjunctival autograft (CAU), conjunctival allograft (CAL), conjunctival limbal autograft (CLAU), cadaveric conjunctival limbal allograft (c-CLAL), living related conjunctival limbal allograft (lr-CLAL), or keratolimbal allograft (KLAL). Evaluation of our keratolimbal allograft patients revealed that 18 of 25 eyes (72%) developed a stable ocular surface. Fifteen eyes (60%) demonstrated a significant improvement in visual acuity. Persistent epithelial defects and symblephara were successfully managed with this procedure. Six of 13 (46%) subsequent keratoplasties were successful. Patients with limbal deficiency due to Stevens-Johnson syndrome had a significantly worse outcome. Patients with preoperative conjunctival keratinization also had a significantly worse outcome. Indications for epithelial transplantation are as follows: For patients with unilateral cicatrizing conjunctival disease, the first option should be CAU. For patients with unilateral limbal deficiency, CLAU is the procedure of choice. For patients with bilateral disease Ir-CLAL should be considered first. If this procedure is not available, then consideration of KLAL is warranted. CONCLUSIONS: Classification of the various epithelial transplantation procedures based on anatomy is useful for an accurate comparison and discussion of the procedures. KLAL is a useful technique in the management of severe ocular surface disease due to limbal deficiency. However, patients with preoperative conjunctival keratinization have a poor prognosis. Consideration of a CLAU or a Ir-CLAL should be made for ocular surface disease on the basis of whether the disease is unilateral or bilateral. The importance of HLA and ABO typing, as well as the protocol for immunosuppression in the allograft procedures for limbal deficiency, needs further study.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alldredge O. C., Krachmer J. H. Clinical types of corneal transplant rejection. Their manifestations, frequency, preoperative correlates, and treatment. Arch Ophthalmol. 1981 Apr;99(4):599–604. doi: 10.1001/archopht.1981.03930010599002. [DOI] [PubMed] [Google Scholar]
- Brown S. I., Bloomfield S. E., Pearce D. B. A follow-up report on transplantation of the alkali-burned cornea. Am J Ophthalmol. 1974 Apr;77(4):538–542. doi: 10.1016/0002-9394(74)90468-1. [DOI] [PubMed] [Google Scholar]
- Brown S. I., Tragakis M. P., Pearce D. B. Corneal transplantation for severe alkali burns. Trans Am Acad Ophthalmol Otolaryngol. 1972 Sep-Oct;76(5):1266–1274. [PubMed] [Google Scholar]
- Chen J. J., Tseng S. C. Abnormal corneal epithelial wound healing in partial-thickness removal of limbal epithelium. Invest Ophthalmol Vis Sci. 1991 Jul;32(8):2219–2233. [PubMed] [Google Scholar]
- Chen J. J., Tseng S. C. Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci. 1990 Jul;31(7):1301–1314. [PubMed] [Google Scholar]
- Chen J. J., Tseng S. C. Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci. 1990 Jul;31(7):1301–1314. [PubMed] [Google Scholar]
- Davanger M., Evensen A. Role of the pericorneal papillary structure in renewal of corneal epithelium. Nature. 1971 Feb 19;229(5286):560–561. doi: 10.1038/229560a0. [DOI] [PubMed] [Google Scholar]
- Dua H. S., Forrester J. V. The corneoscleral limbus in human corneal epithelial wound healing. Am J Ophthalmol. 1990 Dec 15;110(6):646–656. doi: 10.1016/s0002-9394(14)77062-x. [DOI] [PubMed] [Google Scholar]
- Ebato B., Friend J., Thoft R. A. Comparison of limbal and peripheral human corneal epithelium in tissue culture. Invest Ophthalmol Vis Sci. 1988 Oct;29(10):1533–1537. [PubMed] [Google Scholar]
- Friend J., Thoft R. A. Functional competence of regenerating ocular surface epithelium. Invest Ophthalmol Vis Sci. 1978 Feb;17(2):134–139. [PubMed] [Google Scholar]
- Gipson I. K. The epithelial basement membrane zone of the limbus. Eye (Lond) 1989;3(Pt 2):132–140. doi: 10.1038/eye.1989.21. [DOI] [PubMed] [Google Scholar]
- Harris T. M., Berry E. R., Pakurar A. S., Sheppard L. B. Biochemical transformation of bulbar conjunctiva into corneal epithelium: an electrophoretic analysis. Exp Eye Res. 1985 Nov;41(5):597–605. doi: 10.1016/0014-4835(85)90032-6. [DOI] [PubMed] [Google Scholar]
- Herman W. K., Doughman D. J., Lindstrom R. L. Conjunctival autograft transplantation for unilateral ocular surface diseases. Ophthalmology. 1983 Sep;90(9):1121–1126. doi: 10.1016/s0161-6420(83)80056-6. [DOI] [PubMed] [Google Scholar]
- Huang A. J., Watson B. D., Hernandez E., Tseng S. C. Photothrombosis of corneal neovascularization by intravenous rose bengal and argon laser irradiation. Arch Ophthalmol. 1988 May;106(5):680–685. doi: 10.1001/archopht.1988.01060130742036. [DOI] [PubMed] [Google Scholar]
- Jenkins C., Tuft S., Liu C., Buckley R. Limbal transplantation in the management of chronic contact-lens-associated epitheliopathy. Eye (Lond) 1993;7(Pt 5):629–633. doi: 10.1038/eye.1993.145. [DOI] [PubMed] [Google Scholar]
- Kenyon K. R., Tseng S. C. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989 May;96(5):709–723. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- Kenyon K. R., Wagoner M. D., Hettinger M. E. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985 Nov;92(11):1461–1470. doi: 10.1016/s0161-6420(85)33831-9. [DOI] [PubMed] [Google Scholar]
- Kinoshita S., Friend J., Kiorpes T. C., Thoft R. A. Keratin-like proteins in corneal and conjunctival epithelium are different. Invest Ophthalmol Vis Sci. 1983 May;24(5):577–581. [PubMed] [Google Scholar]
- Kinoshita S., Friend J., Thoft R. A. Biphasic cell proliferation in transdifferentiation of conjunctival to corneal epithelium in rabbits. Invest Ophthalmol Vis Sci. 1983 Aug;24(8):1008–1014. [PubMed] [Google Scholar]
- Kinoshita S., Friend J., Thoft R. A. Biphasic cell proliferation in transdifferentiation of conjunctival to corneal epithelium in rabbits. Invest Ophthalmol Vis Sci. 1983 Aug;24(8):1008–1014. [PubMed] [Google Scholar]
- Kinoshita S., Friend J., Thoft R. A. Biphasic cell proliferation in transdifferentiation of conjunctival to corneal epithelium in rabbits. Invest Ophthalmol Vis Sci. 1983 Aug;24(8):1008–1014. [PubMed] [Google Scholar]
- Kolega J., Manabe M., Sun T. T. Basement membrane heterogeneity and variation in corneal epithelial differentiation. Differentiation. 1989 Oct;42(1):54–63. doi: 10.1111/j.1432-0436.1989.tb00607.x. [DOI] [PubMed] [Google Scholar]
- Kruse F. E., Chen J. J., Tsai R. J., Tseng S. C. Conjunctival transdifferentiation is due to the incomplete removal of limbal basal epithelium. Invest Ophthalmol Vis Sci. 1990 Sep;31(9):1903–1913. [PubMed] [Google Scholar]
- Kwitko S., Marinho D., Barcaro S., Bocaccio F., Rymer S., Fernandes S., Neumann J. Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology. 1995 Jul;102(7):1020–1025. doi: 10.1016/s0161-6420(95)30918-9. [DOI] [PubMed] [Google Scholar]
- Lajtha L. G. Stem cell concepts. Differentiation. 1979;14(1-2):23–34. doi: 10.1111/j.1432-0436.1979.tb01007.x. [DOI] [PubMed] [Google Scholar]
- Lajtha L. G. Stem cell concepts. Differentiation. 1979;14(1-2):23–34. doi: 10.1111/j.1432-0436.1979.tb01007.x. [DOI] [PubMed] [Google Scholar]
- Leblond C. P. The life history of cells in renewing systems. Am J Anat. 1981 Feb;160(2):114–158. doi: 10.1002/aja.1001600202. [DOI] [PubMed] [Google Scholar]
- Mackman G., Brightbill F. S., Optiz J. M. Corneal changes in aniridia. Am J Ophthalmol. 1979 Apr;87(4):497–502. doi: 10.1016/0002-9394(79)90238-1. [DOI] [PubMed] [Google Scholar]
- Margo C. E. Congenital aniridia: a histopathologic study of the anterior segment in children. J Pediatr Ophthalmol Strabismus. 1983 Sep-Oct;20(5):192–198. doi: 10.3928/0191-3913-19830901-06. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Havener V. R., Cameron J. D. Cellulose acetate impressions of the ocular surface. Dry eye states. Arch Ophthalmol. 1983 Dec;101(12):1869–1872. doi: 10.1001/archopht.1983.01040020871007. [DOI] [PubMed] [Google Scholar]
- Nelson L. B., Spaeth G. L., Nowinski T. S., Margo C. E., Jackson L. Aniridia. A review. Surv Ophthalmol. 1984 May-Jun;28(6):621–642. doi: 10.1016/0039-6257(84)90184-x. [DOI] [PubMed] [Google Scholar]
- Pfister R. R. Corneal stem cell disease: concepts, categorization, and treatment by auto- and homotransplantation of limbal stem cells. CLAO J. 1994 Jan;20(1):64–72. [PubMed] [Google Scholar]
- Potten C. S., Morris R. J. Epithelial stem cells in vivo. J Cell Sci Suppl. 1988;10:45–62. doi: 10.1242/jcs.1988.supplement_10.4. [DOI] [PubMed] [Google Scholar]
- Puangsricharern V., Tseng S. C. Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology. 1995 Oct;102(10):1476–1485. doi: 10.1016/s0161-6420(95)30842-1. [DOI] [PubMed] [Google Scholar]
- Ronk J. F., Ruiz-Esmenjaud S., Osorio M., Bacigalupi M., Goosey J. D. Limbal conjunctival autograft in a subacute alkaline corneal burn. Cornea. 1994 Sep;13(5):465–468. doi: 10.1097/00003226-199409000-00017. [DOI] [PubMed] [Google Scholar]
- Rubsamen P. E., Irvin W. D., McCuen B. W., 2nd, Smiddy W. E., Bowman C. B. Primary intraocular lens implantation in the setting of penetrating ocular trauma. Ophthalmology. 1995 Jan;102(1):101–107. doi: 10.1016/s0161-6420(95)31073-1. [DOI] [PubMed] [Google Scholar]
- Schermer A., Galvin S., Sun T. T. Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. J Cell Biol. 1986 Jul;103(1):49–62. doi: 10.1083/jcb.103.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro M. S., Friend J., Thoft R. A. Corneal re-epithelialization from the conjunctiva. Invest Ophthalmol Vis Sci. 1981 Jul;21(1 Pt 1):135–142. [PubMed] [Google Scholar]
- The Association for Research in Vision and Ophthalmology. Annual spring meeting. Sarasota, Florida, May 4-8, 1987. Abstracts. Invest Ophthalmol Vis Sci. 1987 Mar;28(3 Suppl):1–430. [PubMed] [Google Scholar]
- Thoft R. A. Conjunctival transplantation. Arch Ophthalmol. 1977 Aug;95(8):1425–1427. doi: 10.1001/archopht.1977.04450080135017. [DOI] [PubMed] [Google Scholar]
- Thoft R. A., Friend J. Biochemical transformation of regenerating ocular surface epithelium. Invest Ophthalmol Vis Sci. 1977 Jan;16(1):14–20. [PubMed] [Google Scholar]
- Thoft R. A. Indications for conjunctival transplantation. Ophthalmology. 1982 Apr;89(4):335–339. doi: 10.1016/s0161-6420(82)34784-3. [DOI] [PubMed] [Google Scholar]
- Thoft R. A. Keratoepithelioplasty. Am J Ophthalmol. 1984 Jan;97(1):1–6. doi: 10.1016/0002-9394(84)90438-0. [DOI] [PubMed] [Google Scholar]
- Thoft R. A., Sugar J. Graft failure in keratoepithelioplasty. Cornea. 1993 Jul;12(4):362–365. doi: 10.1097/00003226-199307000-00014. [DOI] [PubMed] [Google Scholar]
- Tsai R. J., Sun T. T., Tseng S. C. Comparison of limbal and conjunctival autograft transplantation in corneal surface reconstruction in rabbits. Ophthalmology. 1990 Apr;97(4):446–455. doi: 10.1016/s0161-6420(90)32575-7. [DOI] [PubMed] [Google Scholar]
- Tsai R. J., Tseng S. C. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994 Sep;13(5):389–400. doi: 10.1097/00003226-199409000-00003. [DOI] [PubMed] [Google Scholar]
- Tseng S. C. Concept and application of limbal stem cells. Eye (Lond) 1989;3(Pt 2):141–157. doi: 10.1038/eye.1989.22. [DOI] [PubMed] [Google Scholar]
- Tseng S. C., Hirst L. W., Farazdaghi M., Green W. R. Goblet cell density and vascularization during conjunctival transdifferentiation. Invest Ophthalmol Vis Sci. 1984 Oct;25(10):1168–1176. [PubMed] [Google Scholar]
- Tseng S. C. Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology. 1985 Jun;92(6):728–733. doi: 10.1016/s0161-6420(85)33967-2. [DOI] [PubMed] [Google Scholar]
- Tsubota K., Toda I., Saito H., Shinozaki N., Shimazaki J. Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology. 1995 Oct;102(10):1486–1496. doi: 10.1016/s0161-6420(95)30841-x. [DOI] [PubMed] [Google Scholar]
- Tugal-Tutkun I., Akova Y. A., Foster C. S. Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology. 1995 Apr;102(4):576–585. doi: 10.1016/s0161-6420(95)30980-3. [DOI] [PubMed] [Google Scholar]
- Turgeon P. W., Nauheim R. C., Roat M. I., Stopak S. S., Thoft R. A. Indications for keratoepithelioplasty. Arch Ophthalmol. 1990 Feb;108(2):233–236. doi: 10.1001/archopht.1990.01070040085036. [DOI] [PubMed] [Google Scholar]
- Vastine D. W., Stewart W. B., Schwab I. R. Reconstruction of the periocular mucous membrane by autologous conjunctival transplantation. Ophthalmology. 1982 Sep;89(9):1072–1081. doi: 10.1016/s0161-6420(82)34681-3. [DOI] [PubMed] [Google Scholar]
- Zieske J. D. Perpetuation of stem cells in the eye. Eye (Lond) 1994;8(Pt 2):163–169. doi: 10.1038/eye.1994.41. [DOI] [PubMed] [Google Scholar]