Abstract
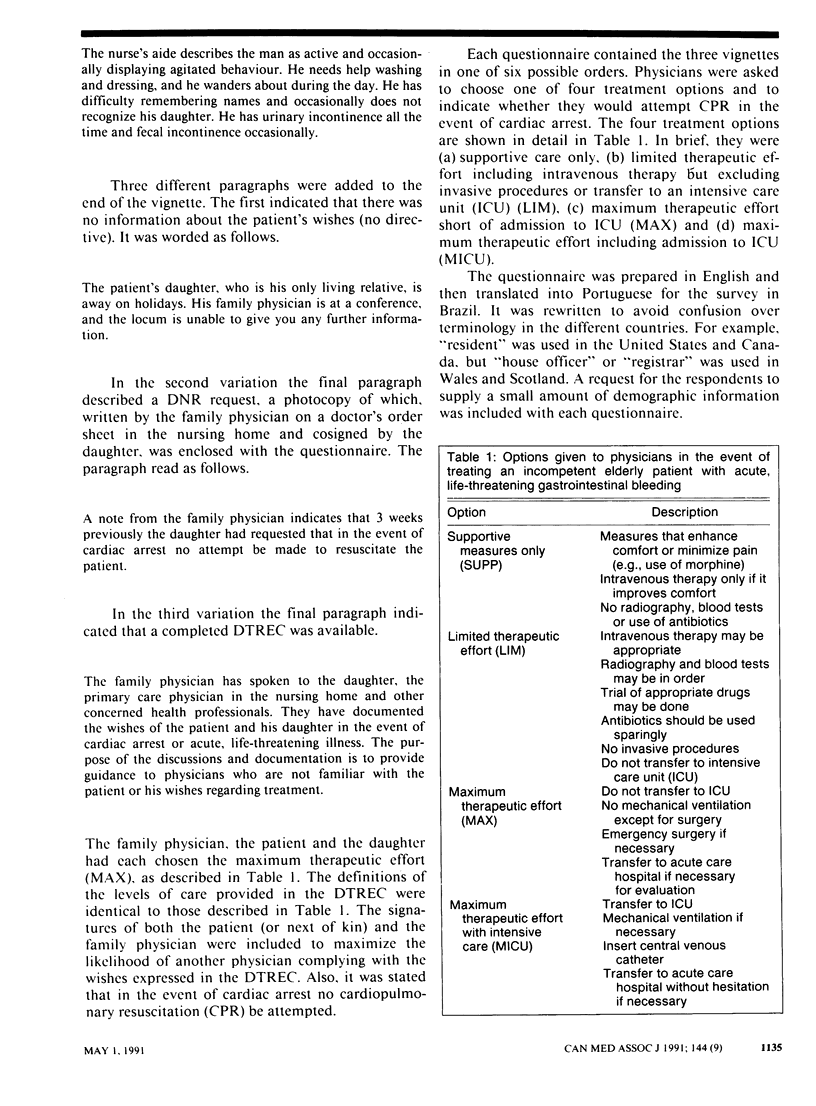
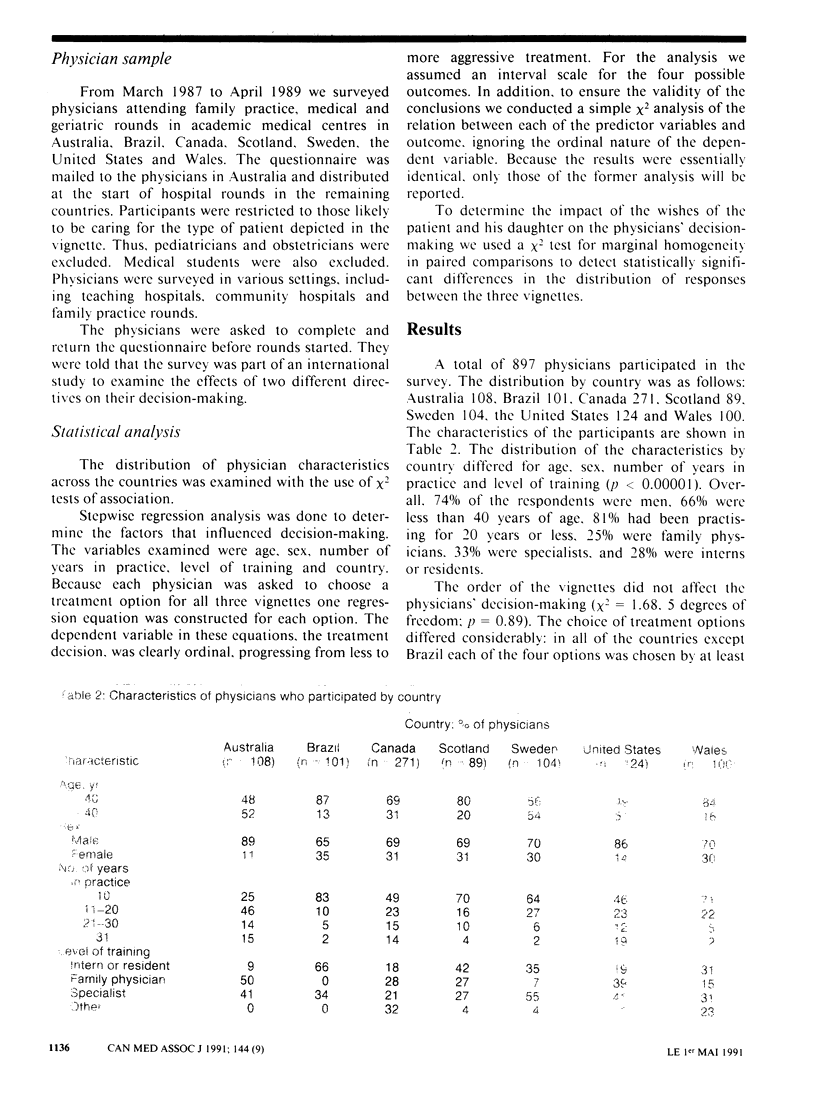
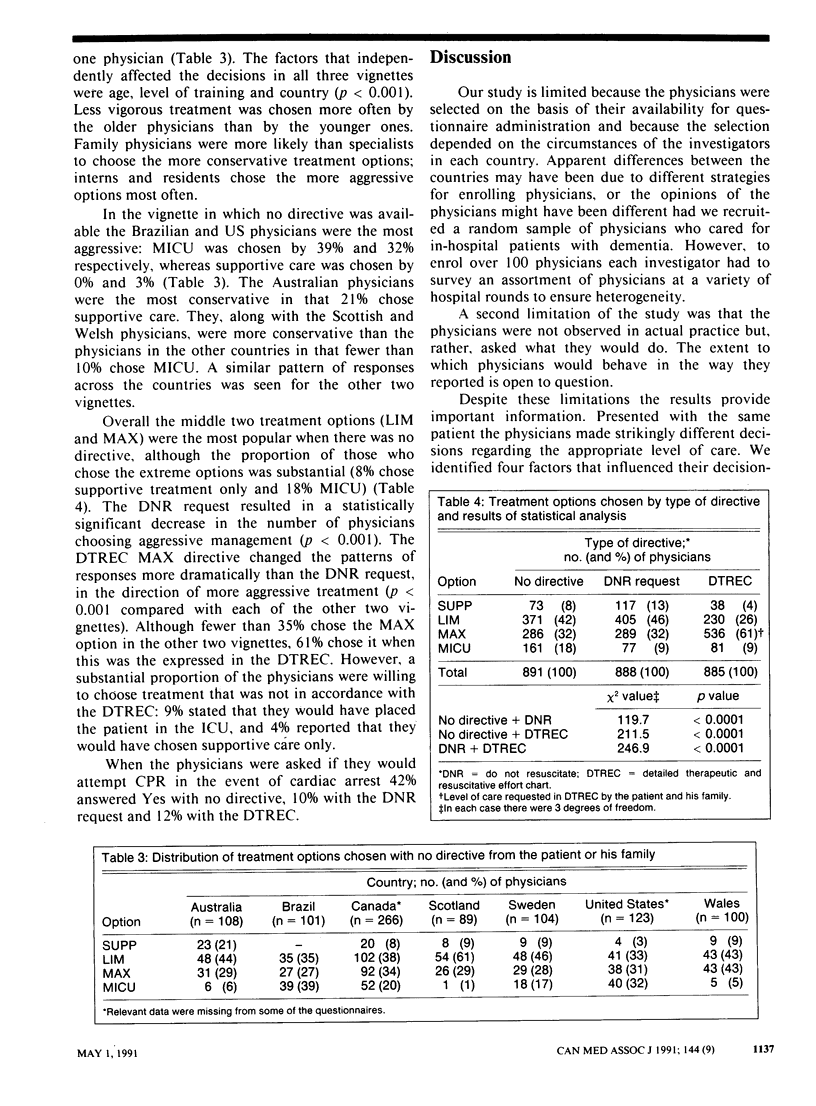
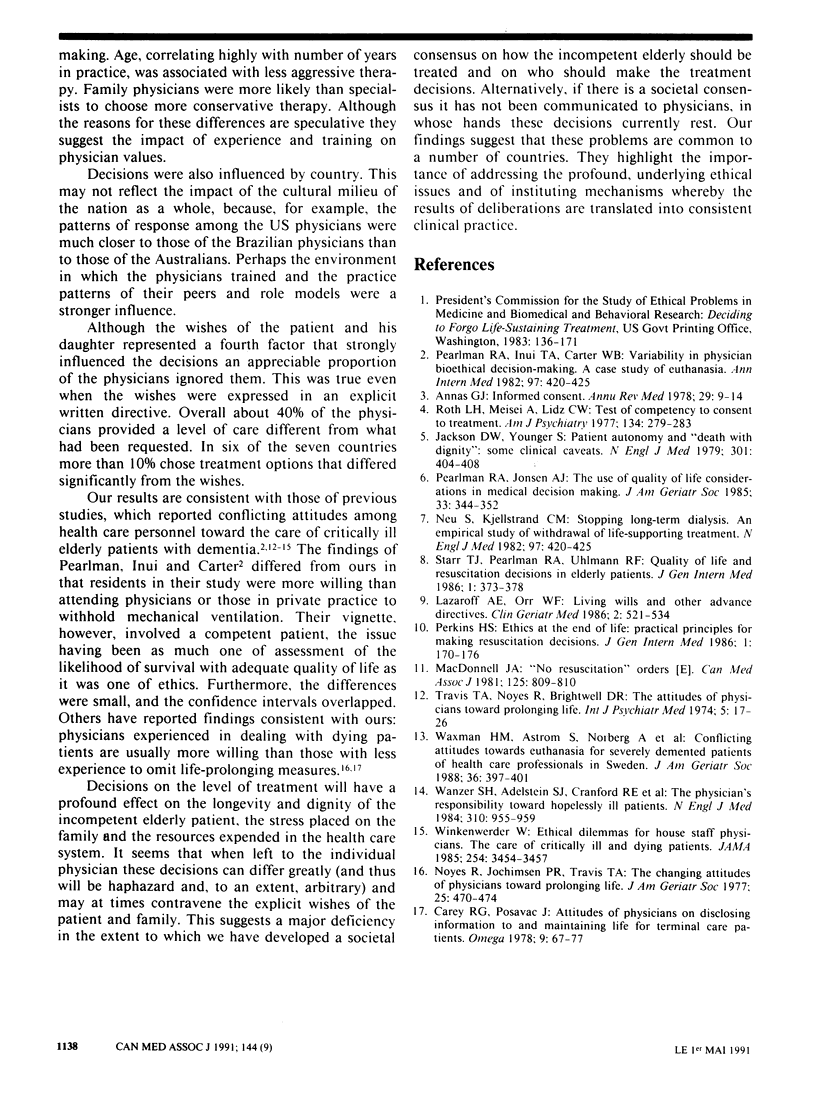
OBJECTIVES: To determine what treatment decisions physicians will make when faced with an incompetent elderly patient with life-threatening gastrointestinal bleeding and to identify the factors that affect their decisions. DESIGN: Survey. SETTING: Family practice, medical and geriatrics rounds in academic medical centres and community hospitals in seven countries. PARTICIPANTS: Physicians who regularly cared for incompetent elderly patients. OUTCOME MEASURE: A self-administered questionnaire containing three case vignettes. Each provided the same details on an incompetent elderly patient; however, one gave no information about the wishes of the patient and his family (no directive), the second provided a do-not-resuscitate (DNR) request, and the third included a detailed therapeutic and resuscitative effort chart (DTREC) requesting maximum therapeutic care without admission to the intensive care unit (ICU). The four treatment options were supportive care only, limited therapeutic care, maximum therapeutic care without admission to the ICU and maximum care with admission to the ICU. MAIN RESULTS: Treatment decisions varied and were systematically related to age, level of training and country (p less than 0.001). The older physicians and those in family medicine were less likely than the others to choose aggressive treatment options. Brazilian and US physicians were the most aggressive; Australian physicians were the most conservative. The DNR request resulted in a significant decrease in the number of physicians choosing aggressive options (p less than 0.001). The DTREC resulted in a move toward more aggressive treatment, as outlined in the directive (p less than 0.001). Overall, however, about 40% of the physicians chose a level of care different from what had been requested. Furthermore, over 10% would have tried cardiopulmonary resuscitation despite the DNR request. CONCLUSION: Treatment of incompetent elderly patients with life-threatening illness varies widely within and between countries. Uniform standards should be developed on the basis of societal values and be communicated to physicians.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Annas G. J. Informed consent. Annu Rev Med. 1978;29:9–14. doi: 10.1146/annurev.me.29.020178.000301. [DOI] [PubMed] [Google Scholar]
- Carey Raymond G., Posavac Emil J. Attitudes of physicians on disclosing information to and maintaining life for terminal patients. Omega (Westport) 1978;9(1):67–77. doi: 10.2190/7tn6-dutc-f6xq-pff8. [DOI] [PubMed] [Google Scholar]
- Jackson D. L., Youngner S. Patient autonomy and "death with dignity": some clinical caveats. N Engl J Med. 1979 Aug 23;301(8):404–408. doi: 10.1056/NEJM197908233010804. [DOI] [PubMed] [Google Scholar]
- Lazaroff A. E., Orr W. F. Living wills and other advance directives. Clin Geriatr Med. 1986 Aug;2(3):521–534. [PubMed] [Google Scholar]
- MacDonell J. A. "No resuscitation" orders. Can Med Assoc J. 1981 Oct 15;125(8):809–810. [PMC free article] [PubMed] [Google Scholar]
- Noyes R., Jr, Jochimsen P. R., Travis T. A. The changing attitudes of physicians toward prolonging life. J Am Geriatr Soc. 1977 Oct;25(10):470–474. doi: 10.1111/j.1532-5415.1977.tb00810.x. [DOI] [PubMed] [Google Scholar]
- Pearlman R. A., Inui T. S., Carter W. B. Variability in physician bioethical decision-making. A case study of euthanasia. Ann Intern Med. 1982 Sep;97(3):420–425. doi: 10.7326/0003-4819-97-3-420. [DOI] [PubMed] [Google Scholar]
- Pearlman R. A., Jonsen A. The use of quality-of-life considerations in medical decision making. J Am Geriatr Soc. 1985 May;33(5):344–352. doi: 10.1111/j.1532-5415.1985.tb07135.x. [DOI] [PubMed] [Google Scholar]
- Perkins H. S. Ethics at the end of life: practical principles for making resuscitation decisions. J Gen Intern Med. 1986 May-Jun;1(3):170–176. doi: 10.1007/BF02602333. [DOI] [PubMed] [Google Scholar]
- Roth L. H., Meisel A., Lidz C. W. Tests of competency to consent to treatment. Am J Psychiatry. 1977 Mar;134(3):279–284. doi: 10.1176/ajp.134.3.279. [DOI] [PubMed] [Google Scholar]
- Starr T. J., Pearlman R. A., Uhlmann R. F. Quality of life and resuscitation decisions in elderly patients. J Gen Intern Med. 1986 Nov-Dec;1(6):373–379. doi: 10.1007/BF02596420. [DOI] [PubMed] [Google Scholar]
- Travis T. A., Noyes R., Jr, Brightwell D. R. The attitudes of physicians toward prolonging life. Psychiatry Med. 1974 Winter;5(1):17–26. [PubMed] [Google Scholar]
- Wanzer S. H., Adelstein S. J., Cranford R. E., Federman D. D., Hook E. D., Moertel C. G., Safar P., Stone A., Taussig H. B., van Eys J. The physician's responsibility toward hopelessly ill patients. N Engl J Med. 1984 Apr 12;310(15):955–959. doi: 10.1056/NEJM198404123101505. [DOI] [PubMed] [Google Scholar]
- Waxman H. M., Astrom S., Norberg A., Winblad B. Conflicting attitudes toward euthanasia for severely demented patients of health care professionals in Sweden. J Am Geriatr Soc. 1988 May;36(5):397–401. doi: 10.1111/j.1532-5415.1988.tb02377.x. [DOI] [PubMed] [Google Scholar]
- Winkenwerder W., Jr Ethical dilemmas for house staff physicians. The care of critically ill and dying patients. JAMA. 1985 Dec 27;254(24):3454–3457. [PubMed] [Google Scholar]


