Abstract
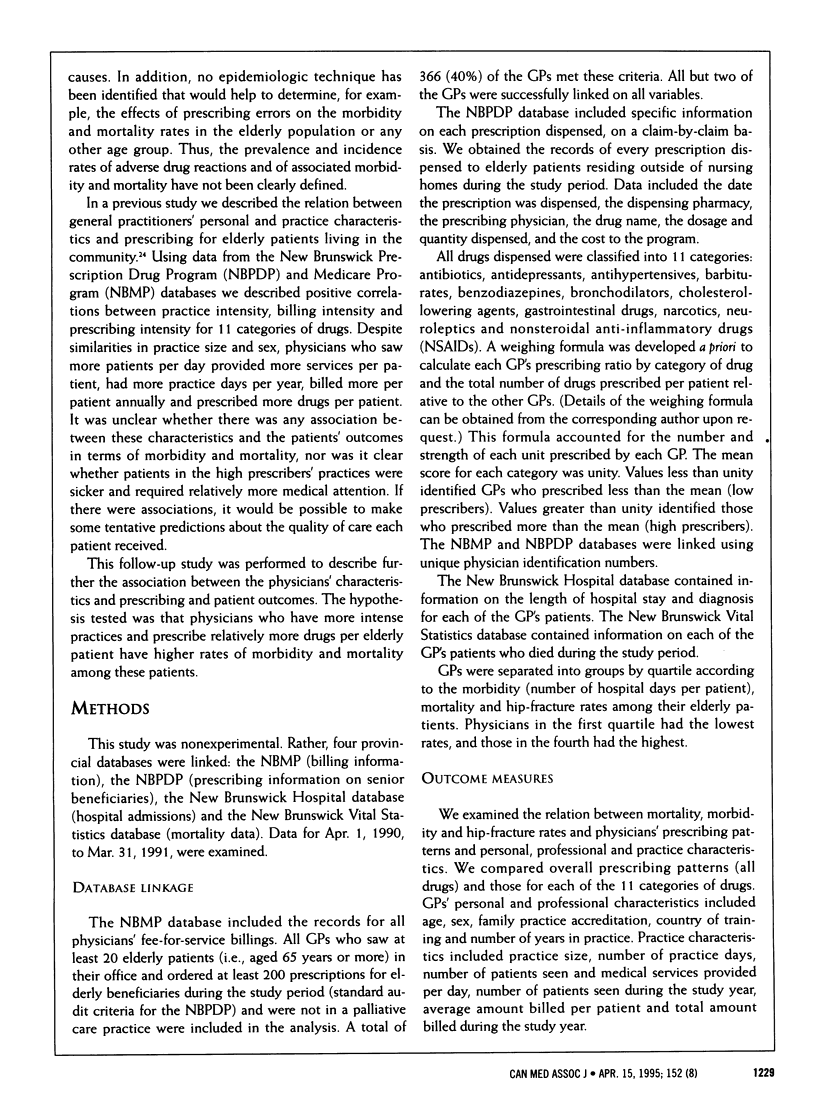
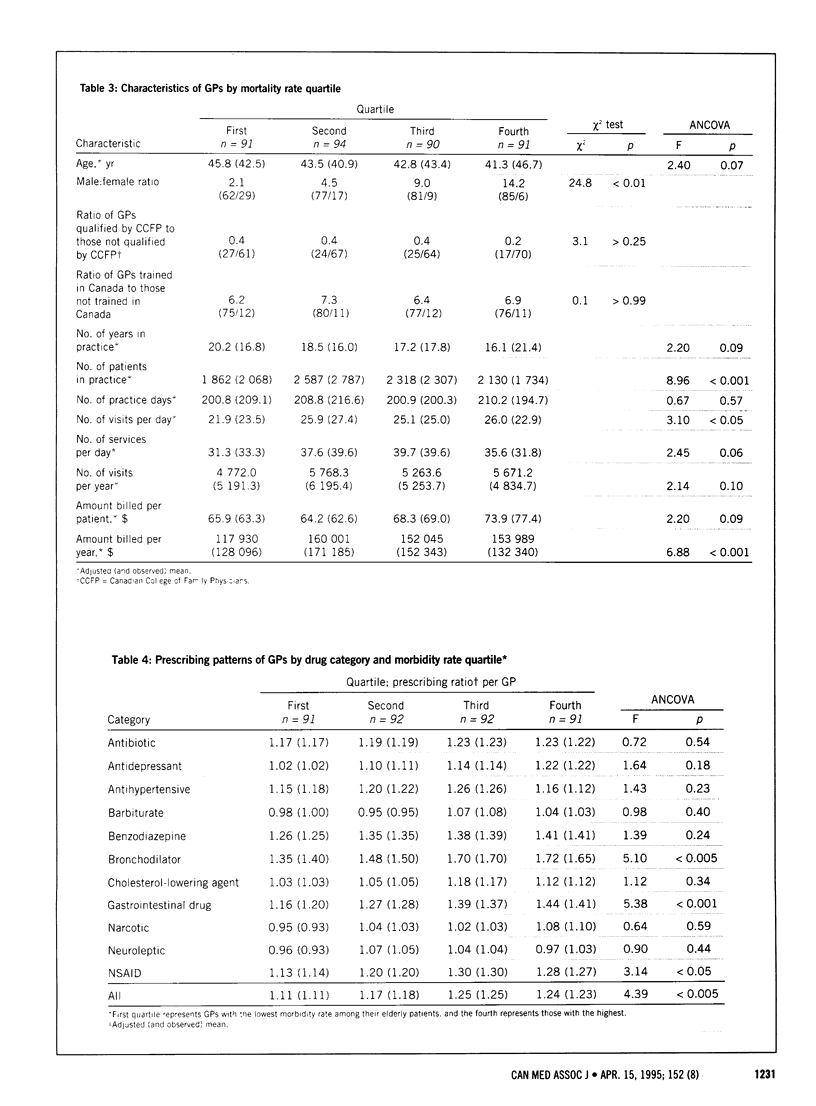
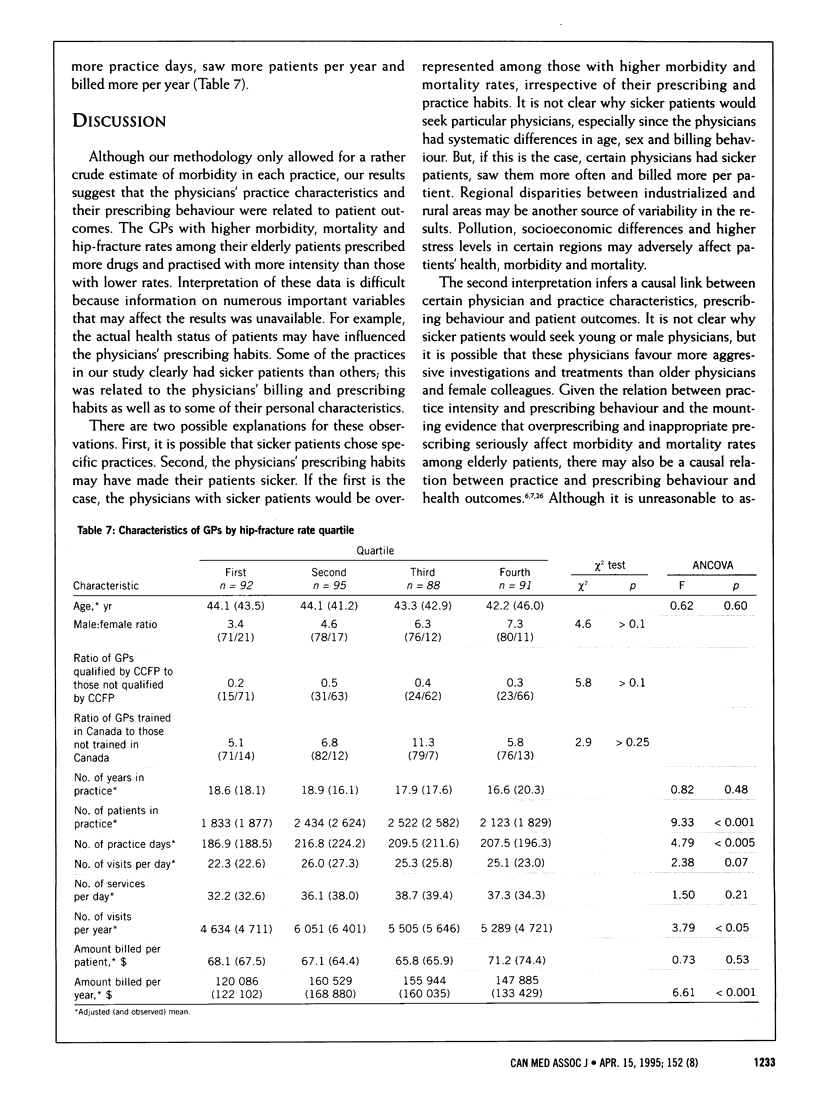
OBJECTIVE: To examine the relation between physician characteristics, prescribing behaviour and patient outcomes. DESIGN: Descriptive study linking four provincial databases. SETTING: New Brunswick. PARTICIPANTS: All 366 general practitioners (GPs) (accounting for 40% of all physicians with a general licence in New Brunswick) who ordered at least 200 prescriptions for elderly beneficiaries of the New Brunswick Prescription Drug Program and saw at least 20 elderly patients in an office setting between Apr. 1, 1990, and Mar. 31, 1991. Physicians with palliative care practices were excluded. OUTCOME MEASURES: GPs' personal, professional and practice characteristics, their prescribing patterns, and mortality, morbidity (number of days in hospital per patient) and hip-fracture rates among their elderly patients. RESULTS: Compared with the GPs who had a lower mortality rate, those with a higher mortality rate prescribed more drugs overall (p < 0.001), specifically antidepressants, bronchodilators, cholesterol-lowering agents, gastrointestinal drugs, neuroleptics and nonsteroidal anti-inflammatory drugs (NSAIDs). They also were more likely to be male (p < 0.01), had larger practices (p < 0.001), saw more patients per day (p < 0.05) and billed more per year (p < 0.001). Compared with the GPs who had a lower morbidity rate, those with a higher morbidity rate prescribed more drugs overall (p < 0.005), specifically bronchodilators, gastrointestinal drugs and NSAIDs. They also were more likely to be younger (p < 0.005) and male (p < 0.01), had fewer years in practice (p < 0.001), saw more patients per day (p < 0.05) and billed more per patient (p < 0.01). The GPs who had a higher hip-fracture rate prescribed more drugs overall (p < 0.001), notably antihypertensives, bronchodilators, cholesterol-lowering agents, gastrointestinal drugs and NSAIDs, than those who had a lower hip-fracture rate. They also had a larger practice (p < 0.001), practised more days per year (p < 0.005), had more patient visits per year (p < 0.05) and billed more per year (p < 0.001). Younger male GPs who practised with relatively more intensity and prescribed more drugs per patient had practices with higher morbidity, mortality and hip-fracture rates among their elderly patients than the other GPs. CONCLUSIONS: There is a significant relation between certain physician characteristics, their prescribing behaviour and patient outcomes. Further study is required to determine what physician characteristics and prescribing behaviours for specific illnesses contribute to patient outcomes. Regional differences should also be examined, as should incentives in this fee-for-service system. Linkage of these types of provincial databases may help in the evaluation of physicians' performance and in the development of strategic interventions and practice guidelines.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bergman U., Wiholm B. E. Drug-related problems causing admission to a medical clinic. Eur J Clin Pharmacol. 1981;20(3):193–200. doi: 10.1007/BF00544597. [DOI] [PubMed] [Google Scholar]
- Colt H. G., Shapiro A. P. Drug-induced illness as a cause for admission to a community hospital. J Am Geriatr Soc. 1989 Apr;37(4):323–326. doi: 10.1111/j.1532-5415.1989.tb05498.x. [DOI] [PubMed] [Google Scholar]
- Davidson W., Molloy D. W., Somers G., Bédard M. Relation between physician characteristics and prescribing for elderly people in New Brunswick. CMAJ. 1994 Mar 15;150(6):917–921. [PMC free article] [PubMed] [Google Scholar]
- Freeman T. R. A study of telephone prescriptions in family practice. J Fam Pract. 1980 May;10(5):857–862. [PubMed] [Google Scholar]
- Hurwitz N., Wade O. L. Intensive hospital monitoring of adverse reactions to drugs. Br Med J. 1969 Mar 1;1(5643):531–536. doi: 10.1136/bmj.1.5643.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahnigen D., Hannon C., Laxson L., LaForce F. M. Iatrogenic disease in hospitalized elderly veterans. J Am Geriatr Soc. 1982 Jun;30(6):387–390. doi: 10.1111/j.1532-5415.1982.tb02837.x. [DOI] [PubMed] [Google Scholar]
- Larson E. B., Kukull W. A., Buchner D., Reifler B. V. Adverse drug reactions associated with global cognitive impairment in elderly persons. Ann Intern Med. 1987 Aug;107(2):169–173. doi: 10.7326/0003-4819-107-2-169. [DOI] [PubMed] [Google Scholar]
- Manasse H. R., Jr Medication use in an imperfect world: drug misadventuring as an issue of public policy, Part 1. Am J Hosp Pharm. 1989 May;46(5):929–944. [PubMed] [Google Scholar]
- Manasse H. R., Jr Medication use in an imperfect world: drug misadventuring as an issue of public policy, Part 2. Am J Hosp Pharm. 1989 Jun;46(6):1141–1152. [PubMed] [Google Scholar]
- Nolan L., O'Malley K. Adverse drug reactions in the elderly. Br J Hosp Med. 1989 May;41(5):446, 448, 452-7. [PubMed] [Google Scholar]
- Popplewell P. Y., Henschke P. J. Acute admissions to a geriatric assessment unit. Med J Aust. 1982 Apr 17;1(8):343–344. doi: 10.5694/j.1326-5377.1982.tb132344.x. [DOI] [PubMed] [Google Scholar]
- Ray W. A., Griffin M. R., Downey W. Benzodiazepines of long and short elimination half-life and the risk of hip fracture. JAMA. 1989 Dec 15;262(23):3303–3307. [PubMed] [Google Scholar]
- Schmucker D. L. Drug disposition in the elderly: a review of the critical factors. J Am Geriatr Soc. 1984 Feb;32(2):144–149. doi: 10.1111/j.1532-5415.1984.tb05856.x. [DOI] [PubMed] [Google Scholar]
- Shimp L. A., Ascione F. J., Glazer H. M., Atwood B. F. Potential medication-related problems in noninstitutionalized elderly. Drug Intell Clin Pharm. 1985 Oct;19(10):766–772. doi: 10.1177/106002808501901024. [DOI] [PubMed] [Google Scholar]
- Tamblyn R. M., McLeod P. J., Abrahamowicz M., Monette J., Gayton D. C., Berkson L., Dauphinee W. D., Grad R. M., Huang A. R., Isaac L. M. Questionable prescribing for elderly patients in Quebec. CMAJ. 1994 Jun 1;150(11):1801–1809. [PMC free article] [PubMed] [Google Scholar]
- Weedle P. B., Poston J. W., Parish P. A. Drug prescribing in residential homes for elderly people in the United Kingdom. DICP. 1990 May;24(5):533–536. doi: 10.1177/106002809002400513. [DOI] [PubMed] [Google Scholar]
- Williamson J., Chopin J. M. Adverse reactions to prescribed drugs in the elderly: a multicentre investigation. Age Ageing. 1980 May;9(2):73–80. doi: 10.1093/ageing/9.2.73. [DOI] [PubMed] [Google Scholar]


