Abstract
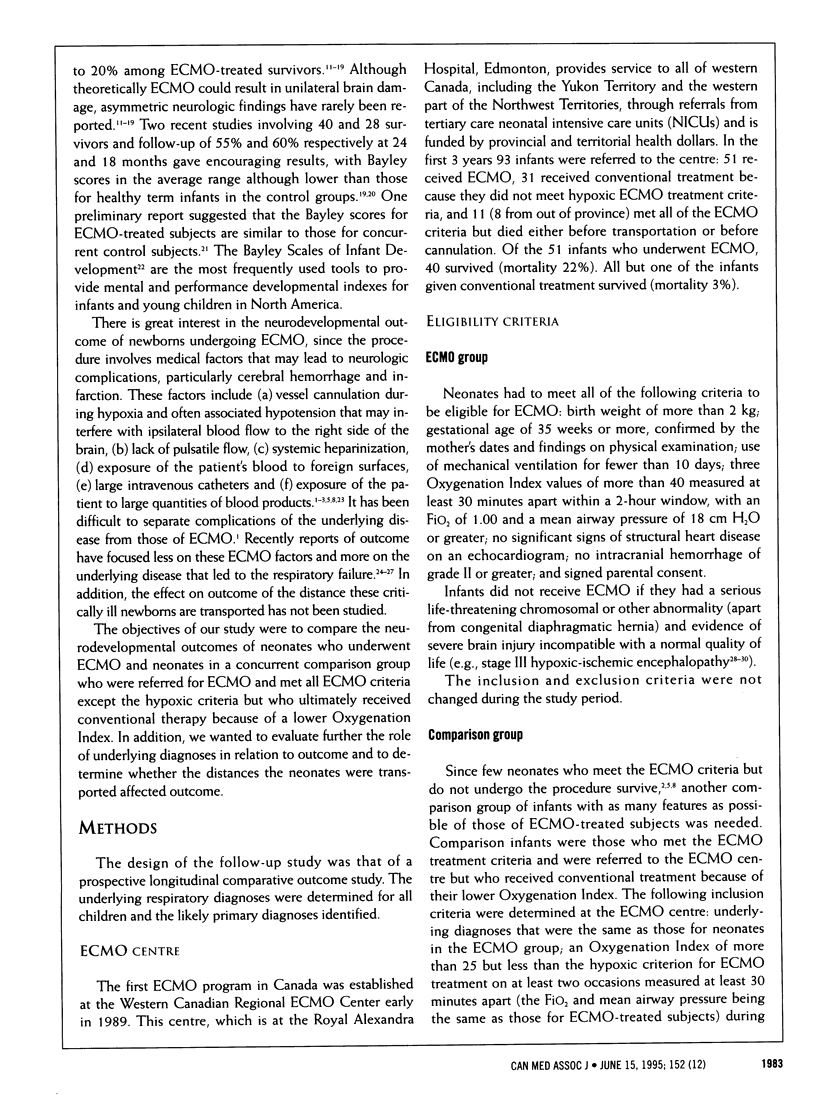
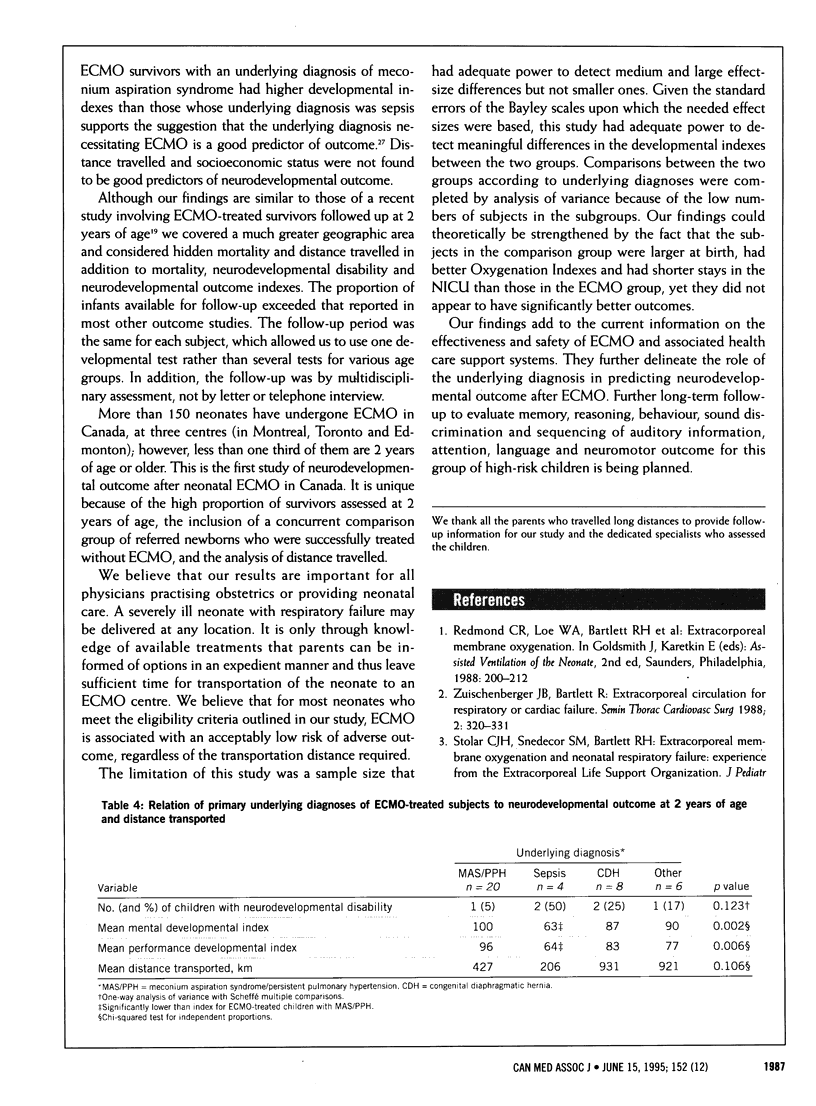
OBJECTIVE: To determine the neurodevelopmental outcome of neonates who underwent extracorporeal membrane oxygenation (ECMO group) and similarly critically ill newborns with a lower Oxygenation Index who underwent conventional treatment (comparison group), and to determine whether factors such as the underlying diagnosis and the distance transported from outlying areas affect outcome. DESIGN: Multicentre prospective longitudinal comparative outcome study. SETTING: An ECMO centre providing services to all of western Canada and four tertiary care neonatal follow-up clinics. SUBJECTS: All neonates who received treatment between February 1989 and January 1992 at the Western Canadian Regional ECMO Center and who were alive at 2 years of age; 38 (95%) of the 40 surviving ECMO-treated subjects and 26 (87%) of the 30 surviving comparison subjects were available for follow-up. INTERVENTIONS: ECMO or conventional therapy for respiratory failure. OUTCOME MEASURES: Neurodevelopmental disability (one or more of cerebral palsy, visual or hearing loss, seizures, severe cognitive disability), and mental and performance developmental indexes of the Bayley Scales of Infant Development. RESULTS: Six (16%) of the ECMO-treated children had neurodevelopmental disabilities at 2 years of age, as compared with 1 (4%) of the comparison subjects; the difference was not statistically significant. The mean mental developmental index (91.8 [standard deviation (SD) 19.5] v. 100.5 [SD 25.4]) and the mean performance developmental index (87.2 [SD 20.0] v. 96.4 [SD 20.9]) did not differ significantly between the ECMO group and the comparison group respectively. Among the ECMO-treated subjects those whose underlying diagnosis was sepsis had the lowest Bayley indexes, significantly lower than those whose underlying diagnosis was meconium aspiration syndrome. The distance transported did not affect outcome. CONCLUSIONS: Neurodevelopmental disability and delay occurred in both groups. The underlying diagnosis appears to affect outcome, whereas distance transported does not. These findings support early transfer for ECMO of critically ill neonates with respiratory failure who do not respond to conventional treatment. Larger multicentre studies involving long-term follow-up are needed to confirm these findings.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BAX M. C. TERMINOLOGY AND CLASSIFICATION OF CEREBRAL PALSY. Dev Med Child Neurol. 1964 Jun;6:295–297. doi: 10.1111/j.1469-8749.1964.tb10791.x. [DOI] [PubMed] [Google Scholar]
- Bartlett R. H., Gazzaniga A. B., Jefferies M. R., Huxtable R. F., Haiduc N. J., Fong S. W. Extracorporeal membrane oxygenation (ECMO) cardiopulmonary support in infancy. Trans Am Soc Artif Intern Organs. 1976;22:80–93. [PubMed] [Google Scholar]
- Bartlett R. H., Gazzaniga A. B., Toomasian J., Coran A. G., Roloff D., Rucker R., Corwin A. G. Extracorporeal membrane oxygenation (ECMO) in neonatal respiratory failure. 100 cases. Ann Surg. 1986 Sep;204(3):236–245. doi: 10.1097/00000658-198609000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett R. H., Roloff D. W., Cornell R. G., Andrews A. F., Dillon P. W., Zwischenberger J. B. Extracorporeal circulation in neonatal respiratory failure: a prospective randomized study. Pediatrics. 1985 Oct;76(4):479–487. [PubMed] [Google Scholar]
- Boedy R. F., Howell C. G., Kanto W. P., Jr Hidden mortality rate associated with extracorporeal membrane oxygenation. J Pediatr. 1990 Sep;117(3):462–464. doi: 10.1016/s0022-3476(05)81098-4. [DOI] [PubMed] [Google Scholar]
- Flusser H., Dodge N. N., Engle W. E., Garg B. P., West K. W. Neurodevelopmental outcome and respiratory morbidity for extracorporeal membrane oxygenation survivors at 1 year of age. J Perinatol. 1993 Jul-Aug;13(4):266–271. [PubMed] [Google Scholar]
- Glass P., Miller M., Short B. Morbidity for survivors of extracorporeal membrane oxygenation: neurodevelopmental outcome at 1 year of age. Pediatrics. 1989 Jan;83(1):72–78. [PubMed] [Google Scholar]
- Griffin M. P., Minifee P. K., Landry S. H., Allison P. L., Swischuk L. E., Zwischenberger J. B. Neurodevelopmental outcome in neonates after extracorporeal membrane oxygenation: cranial magnetic resonance imaging and ultrasonography correlation. J Pediatr Surg. 1992 Jan;27(1):33–35. doi: 10.1016/0022-3468(92)90099-s. [DOI] [PubMed] [Google Scholar]
- Hofkosh D., Thompson A. E., Nozza R. J., Kemp S. S., Bowen A., Feldman H. M. Ten years of extracorporeal membrane oxygenation: neurodevelopmental outcome. Pediatrics. 1991 Apr;87(4):549–555. [PubMed] [Google Scholar]
- Kirkpatrick B. V., Krummel T. M., Mueller D. G., Ormazabal M. A., Greenfield L. J., Salzberg A. M. Use of extracorporeal membrane oxygenation for respiratory failure in term infants. Pediatrics. 1983 Dec;72(6):872–876. [PubMed] [Google Scholar]
- O'Rourke P. P., Crone R. K., Vacanti J. P., Ware J. H., Lillehei C. W., Parad R. B., Epstein M. F. Extracorporeal membrane oxygenation and conventional medical therapy in neonates with persistent pulmonary hypertension of the newborn: a prospective randomized study. Pediatrics. 1989 Dec;84(6):957–963. [PubMed] [Google Scholar]
- Robertson C. M., Finer N. N., Grace M. G. School performance of survivors of neonatal encephalopathy associated with birth asphyxia at term. J Pediatr. 1989 May;114(5):753–760. doi: 10.1016/s0022-3476(89)80132-5. [DOI] [PubMed] [Google Scholar]
- Robertson C. M., Finer N. N. Long-term follow-up of term neonates with perinatal asphyxia. Clin Perinatol. 1993 Jun;20(2):483–500. [PubMed] [Google Scholar]
- Robertson C., Finer N. Term infants with hypoxic-ischemic encephalopathy: outcome at 3.5 years. Dev Med Child Neurol. 1985 Aug;27(4):473–484. doi: 10.1111/j.1469-8749.1985.tb04571.x. [DOI] [PubMed] [Google Scholar]
- Saigal S., Rosenbaum P., Hattersley B., Milner R. Decreased disability rate among 3-year-old survivors weighing 501 to 1000 grams at birth and born to residents of a geographically defined region from 1981 to 1984 compared with 1977 to 1980. J Pediatr. 1989 May;114(5):839–846. doi: 10.1016/s0022-3476(89)80150-7. [DOI] [PubMed] [Google Scholar]
- Sarnat H. B., Sarnat M. S. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976 Oct;33(10):696–705. doi: 10.1001/archneur.1976.00500100030012. [DOI] [PubMed] [Google Scholar]
- Schumacher R. E., Palmer T. W., Roloff D. W., LaClaire P. A., Bartlett R. H. Follow-up of infants treated with extracorporeal membrane oxygenation for newborn respiratory failure. Pediatrics. 1991 Apr;87(4):451–457. [PubMed] [Google Scholar]
- Taylor G. A., Fitz C. R., Glass P., Short B. L. CT of cerebrovascular injury after neonatal extracorporeal membrane oxygenation: implications for neurodevelopmental outcome. AJR Am J Roentgenol. 1989 Jul;153(1):121–126. doi: 10.2214/ajr.153.1.121. [DOI] [PubMed] [Google Scholar]
- Toomasian J. M., Snedecor S. M., Cornell R. G., Cilley R. E., Bartlett R. H. National experience with extracorporeal membrane oxygenation for newborn respiratory failure. Data from 715 cases. ASAIO Trans. 1988 Apr-Jun;34(2):140–147. doi: 10.1097/00002480-198804000-00011. [DOI] [PubMed] [Google Scholar]
- Van Meurs K. P., Newman K. D., Anderson K. D., Short B. L. Effect of extracorporeal membrane oxygenation on survival of infants with congenital diaphragmatic hernia. J Pediatr. 1990 Dec;117(6):954–960. doi: 10.1016/s0022-3476(05)80144-1. [DOI] [PubMed] [Google Scholar]
- Van Meurs K. P., Robbins S. T., Reed V. L., Karr S. S., Wagner A. E., Glass P., Anderson K. D., Short B. L. Congenital diaphragmatic hernia: long-term outcome in neonates treated with extracorporeal membrane oxygenation. J Pediatr. 1993 Jun;122(6):893–899. doi: 10.1016/s0022-3476(09)90013-0. [DOI] [PubMed] [Google Scholar]
- Wildin S. R., Landry S. H., Zwischenberger J. B. Prospective, controlled study of developmental outcome in survivors of extracorporeal membrane oxygenation: the first 24 months. Pediatrics. 1994 Mar;93(3):404–408. [PubMed] [Google Scholar]
- Zwischenberger J. B., Bartlett R. H. Extracorporeal circulation for respiratory or cardiac failure. Semin Thorac Cardiovasc Surg. 1990 Oct;2(4):320–331. [PubMed] [Google Scholar]


