Abstract
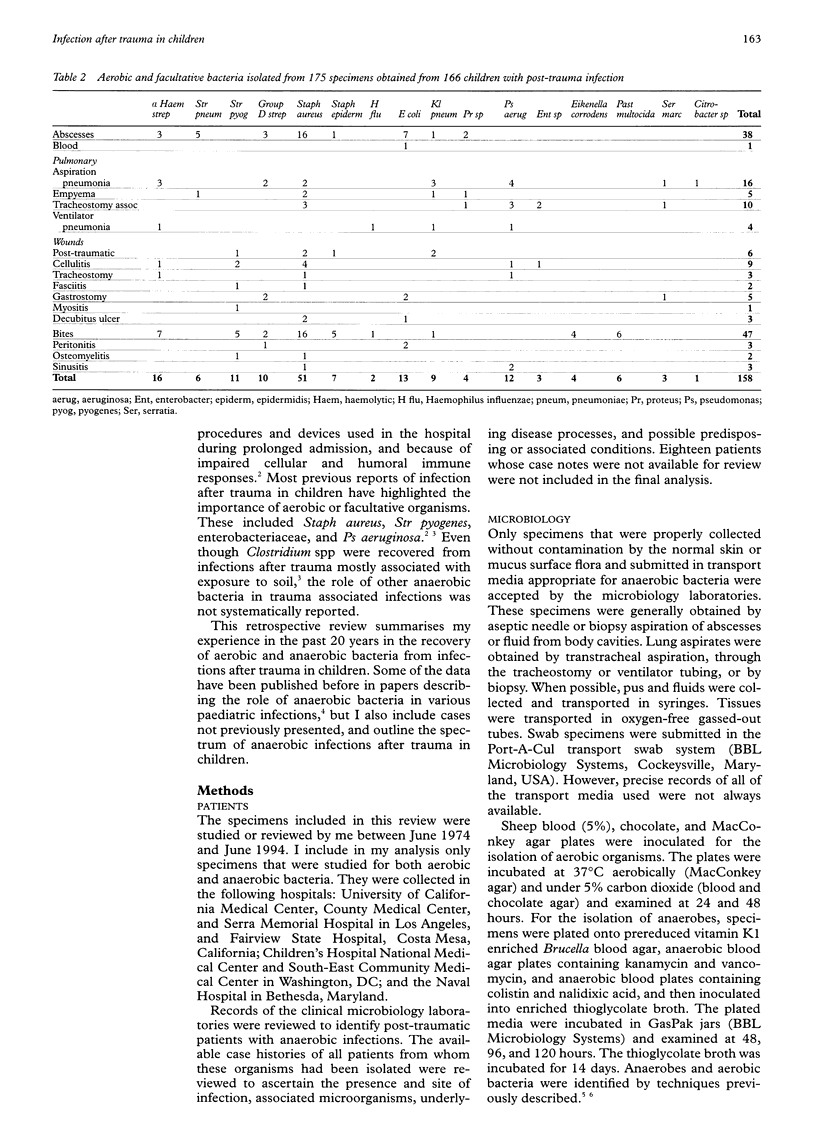
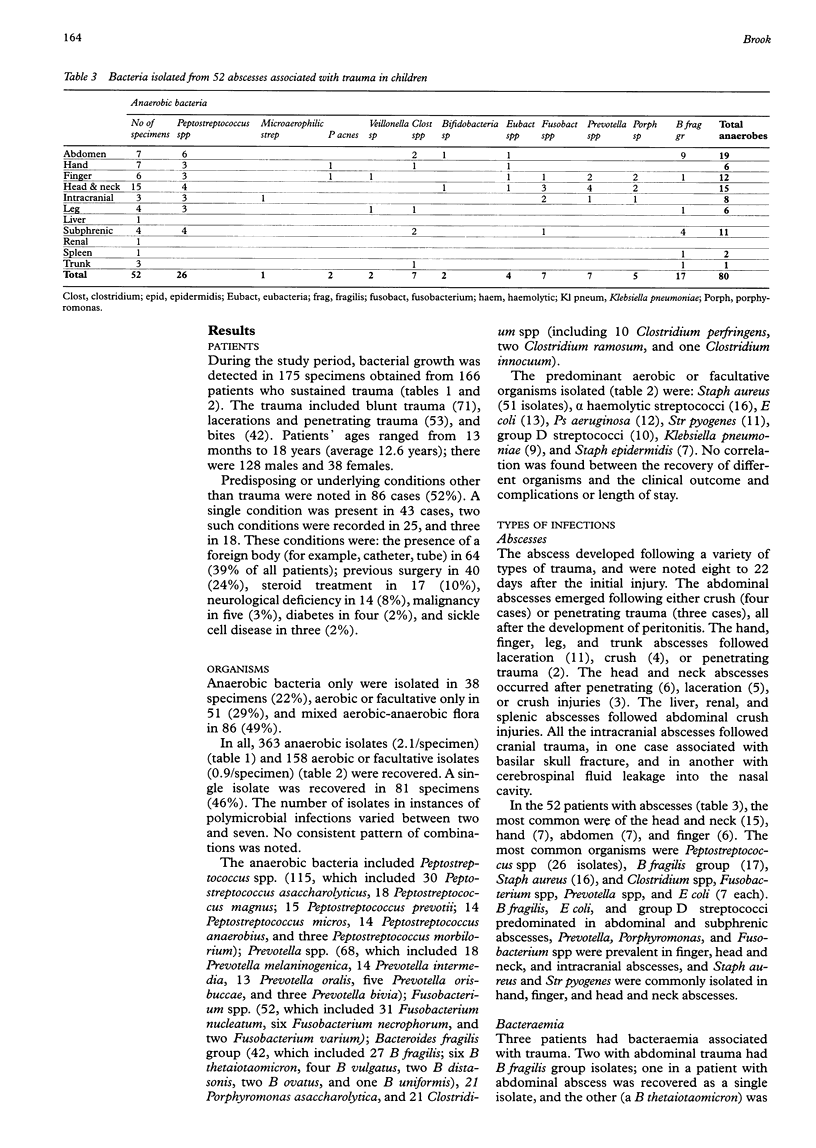
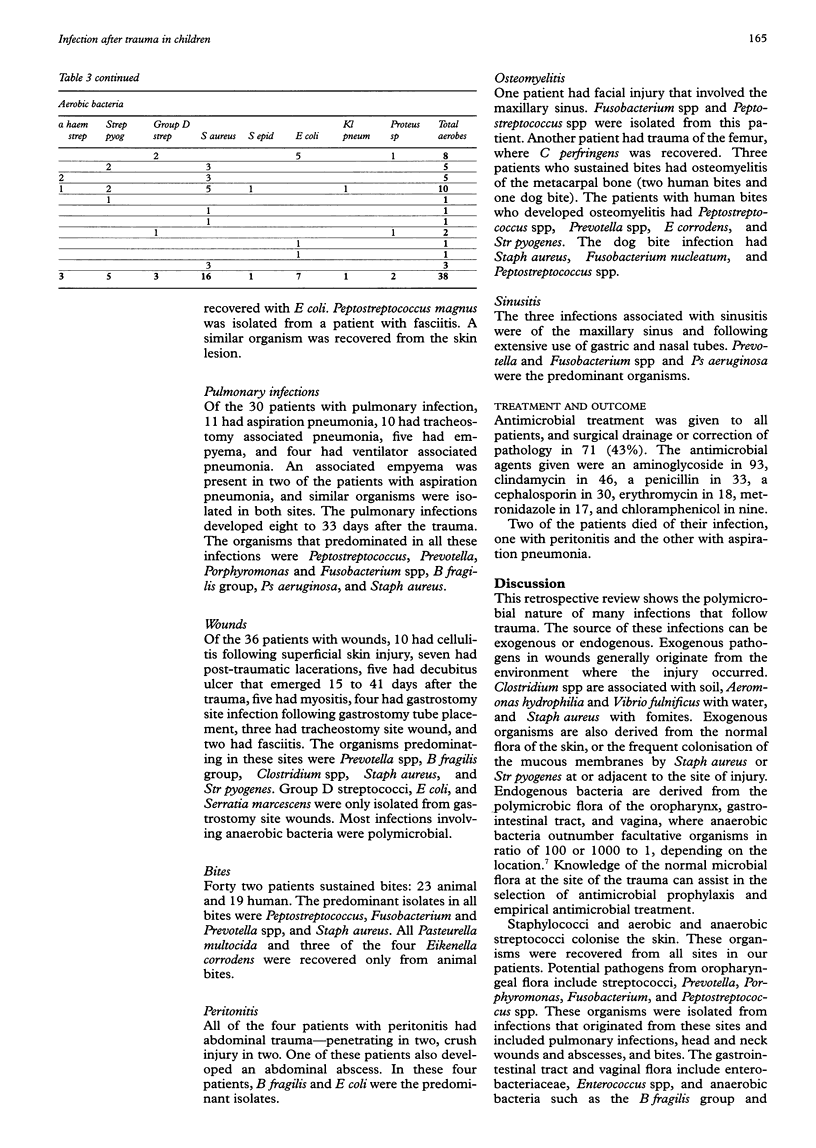
OBJECTIVE: To review the recovery of aerobic and anaerobic bacteria from infections after trauma in children over a 20 year period. METHODS: Only specimens that were studied for both aerobic and anaerobic bacteria were included in the analysis. They were collected from seven separate centres in which the microbiology laboratories only accepted specimens that were properly collected without contamination and were submitted in appropriate transport media. Anaerobes and aerobic bacteria were cultured and identified using standard techniques. Clinical records were reviewed to identify post-trauma patients. RESULTS: From 1974 to 1994, 175 specimens obtained from 166 children with trauma showed bacterial growth. The trauma included blunt trauma (71), lacerations (48), bites (42), and open fractures (5). Anaerobic bacteria only were isolated in 38 specimens (22%), aerobic bacteria only in 51 (29%), and mixed aerobic-anaerobic flora in 86 (49%); 363 anaerobic (2.1/specimen) and 158 aerobic or facultative isolates (0.9/specimen) were recovered. The predominant anaerobic bacteria included Peptostreptococcus spp (115 isolates), Prevotella spp (68), Fusobacterium spp (52), B fragilis group (42), and Clostridium spp (21). The predominant aerobic bacteria included Staph aureus (51), E coli (13), Ps aeruginosa (12), Str pyogenes (11) and Klebsiella pneumoniae (9). Principal infections were: abscesses (52), bacteraemia (3), pulmonary infections (30, including aspiration pneumonia, tracheostomy associated pneumonia, empyema, and ventilator associated pneumonia), wounds (36, including cellulitis, post-traumatic wounds, decubitus ulcers, myositis, gastrostomy and tracheostomy site wounds, and fasciitis), bites (42, including 23 animal and 19 human), peritonitis (4), osteomyelitis (5), and sinusitis (3). Staph aureus and Str pyogenes were isolated at all sites. However, organisms of the oropharyngeal flora predominated in infections that originated from head and neck wounds and abscesses, and bites, and those from the gastrointestinal tract predominated in infections that originated from peritonitis, abdominal abscesses, and decubitus ulcers. CONCLUSIONS: Many infections that follow trauma in children involve multiple organisms.
Full text
PDF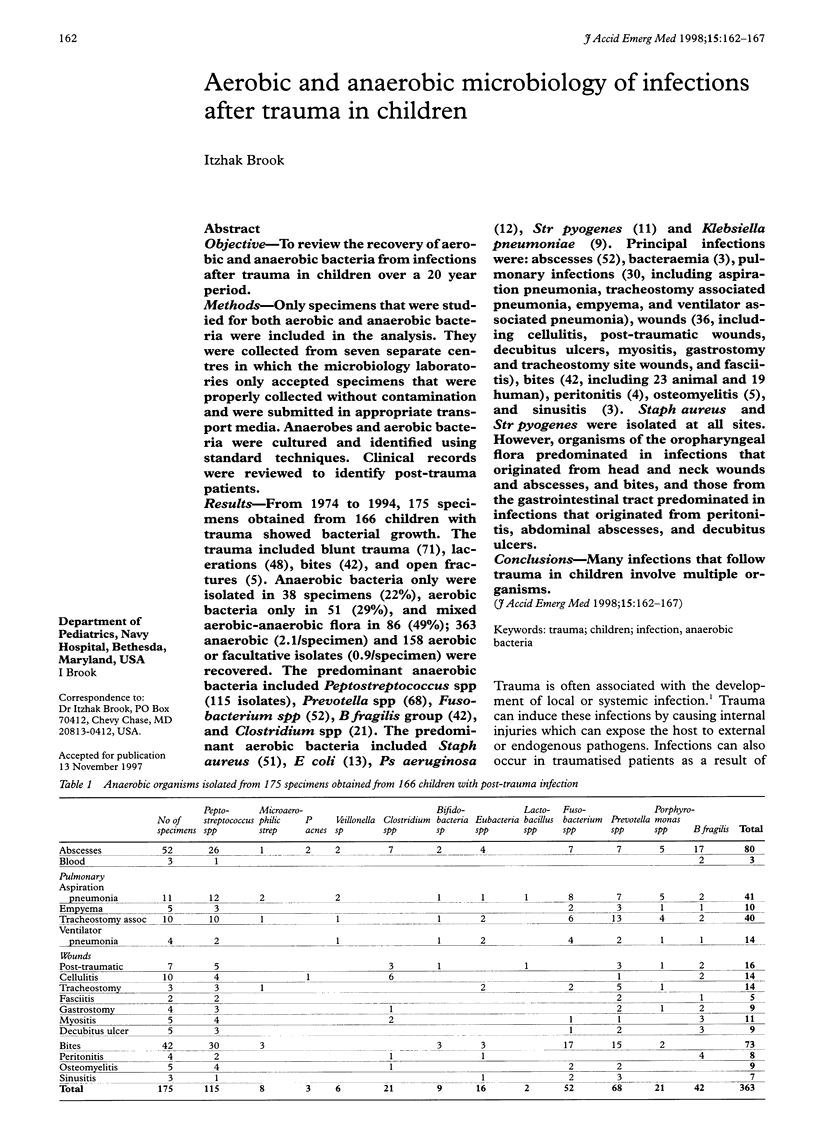

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- APPELBAUM E. Meningitis following trauma to the head and face. JAMA. 1960 Aug 20;173:1818–1822. doi: 10.1001/jama.1960.03020340036010. [DOI] [PubMed] [Google Scholar]
- Brook I. Bacterial studies of peritoneal cavity and postoperative surgical wound drainage following perforated appendix in children. Ann Surg. 1980 Aug;192(2):208–212. doi: 10.1097/00000658-198008000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook I., Finegold S. M. Bacteriology of aspiration pneumonia in children. Pediatrics. 1980 Jun;65(6):1115–1120. [PubMed] [Google Scholar]
- Brook I., Frazier E. H. Clinical and microbiological features of necrotizing fasciitis. J Clin Microbiol. 1995 Sep;33(9):2382–2387. doi: 10.1128/jcm.33.9.2382-2387.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook I. Management of infection following intra-abdominal trauma. Ann Emerg Med. 1988 Jun;17(6):626–632. doi: 10.1016/s0196-0644(88)80405-0. [DOI] [PubMed] [Google Scholar]
- Dellinger E. P. Antibiotic prophylaxis in trauma: penetrating abdominal injuries and open fractures. Rev Infect Dis. 1991 Sep-Oct;13 (Suppl 10):S847–S857. doi: 10.1093/clinids/13.supplement_10.s847. [DOI] [PubMed] [Google Scholar]
- Nichols R. L., Smith J. W. Gas in the wound: what does it mean? Surg Clin North Am. 1975 Dec;55(6):1289–1296. doi: 10.1016/s0039-6109(16)40783-8. [DOI] [PubMed] [Google Scholar]
- Renwick S. E., Ritterbusch J. F. Pyomyositis in children. J Pediatr Orthop. 1993 Nov-Dec;13(6):769–772. doi: 10.1097/01241398-199311000-00016. [DOI] [PubMed] [Google Scholar]
- Wang K. C., Shih C. H. Necrotizing fasciitis of the extremities. J Trauma. 1992 Feb;32(2):179–182. doi: 10.1097/00005373-199202000-00011. [DOI] [PubMed] [Google Scholar]


