Abstract
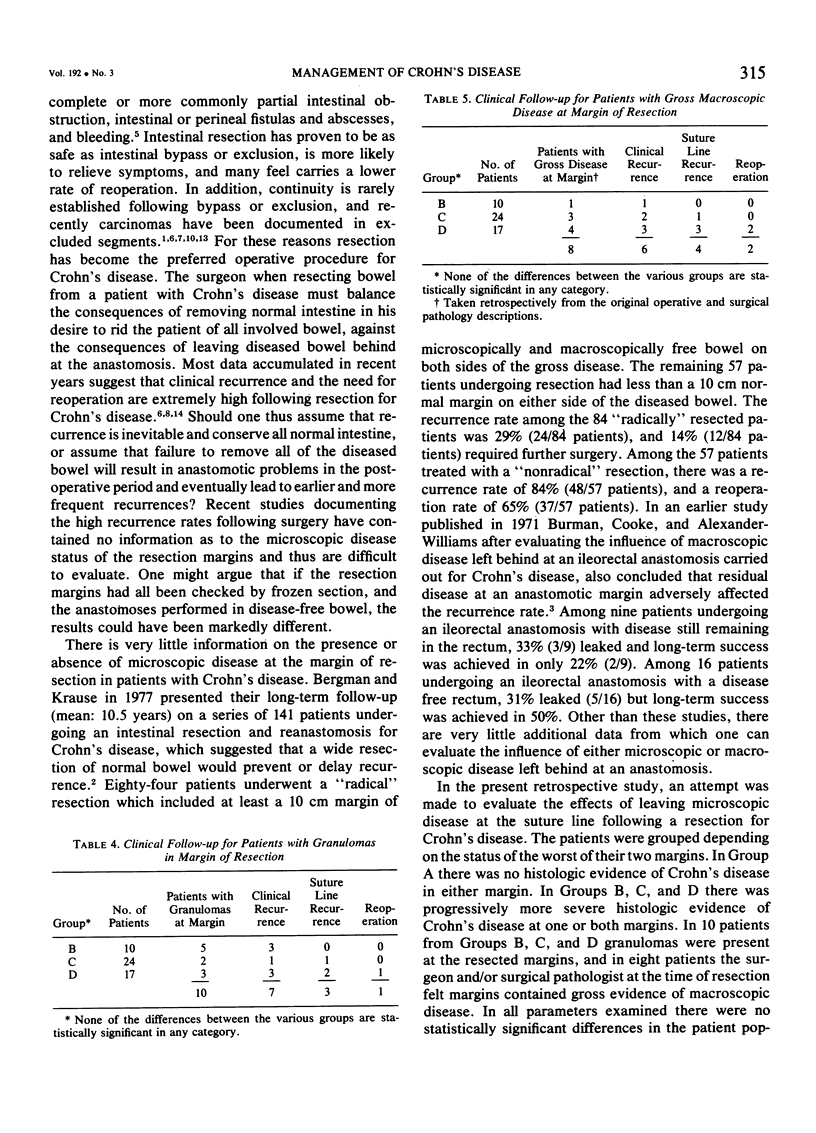
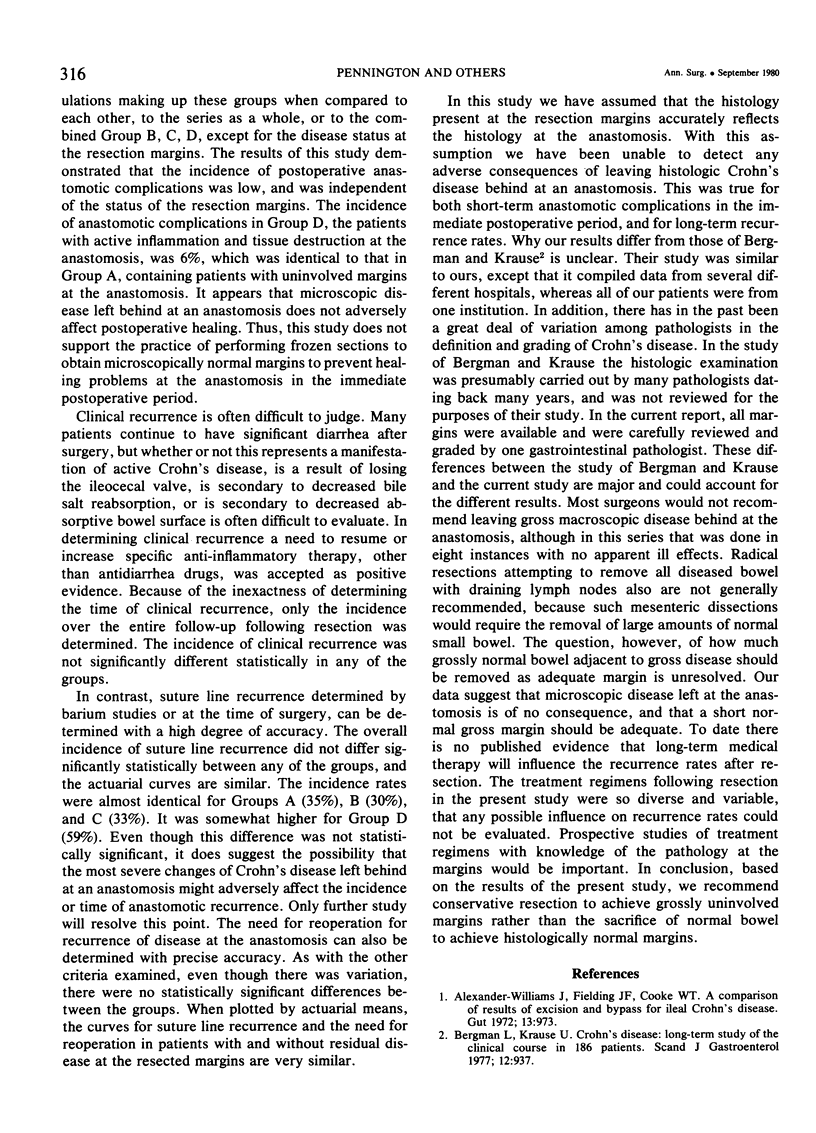
To determine the influence of microscopic disease at an anastomosis following intestinal resection for Crohn's disease, 97 patients undergoing 103 resections were reviewed. Most resections (85/103) involved both small and large bowel and were followed by an ileocolic anastomosis. All resection margins were available and were reviewed. In 52 instances there was no evidence of Crohn's disease at the margins. In 51 instances histologic evidence of Crohn's disease varying from chronic inflammation to tissue destruction was present in one or both margins. The incidence of immediate postoperative anastomotic complications (leak with fistula or abscess, or obstruction) was identical in patients with microscopically normal margins (3/52; 6%) and in patients with microscopic Crohn's disease at the margins (3/51; 6%). The patients were followed for a mean of 5.4 +/- 4.2 years. A clinical recurrence developed during the follow-up period in 50% (26/52) of those patients with normal margins, and in 61% (31/51) of those patients with involved margins. A suture line recurrence developed in 35% (18/52) and required reoperation in 17% (9/52) of those patients with microscopically normal margins. A suture line recurrence developed in 41% of the patients (21/51) and required reoperation in 24% (12/51) of those with microscopically involved margins. None of these differences are statistically significant. The presence or absence of microscopic disease at the anastomosis did not appear to influence immediate anastomotic wound healing or long-term recurrence rates. We therefore recommend conservative resections for Crohn's disease to achieve grossly uninvolved margins rather than the sacrifice of normal bowel to achieve histologically normal margins.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander-Williams J., Fielding J. F., Cooke W. T. A comparison of results of excision and bypass for ileal Crohn's disease. Gut. 1972 Dec;13(12):973–975. doi: 10.1136/gut.13.12.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman L., Krause U. Crohn's disease. A long-term study of the clinical course in 186 patients. Scand J Gastroenterol. 1977;12(8):937–944. doi: 10.3109/00365527709181353. [DOI] [PubMed] [Google Scholar]
- Burman J. H., Cooke W. T., Williams J. A. The fate of ileorectal anastomosis in Crohn's disease. Gut. 1971 Jun;12(6):432–436. doi: 10.1136/gut.12.6.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colcock B. P. Operative technique in surgery for Crohn's disease and its relationship to recurrence. Surg Clin North Am. 1973 Apr;53(2):375–380. doi: 10.1016/s0039-6109(16)39991-1. [DOI] [PubMed] [Google Scholar]
- Farmer R. G., Hawk W. A., Turnbull R. B., Jr Indications for surgery in Crohn's disease: analysis of 500 cases. Gastroenterology. 1976 Aug;71(2):245–250. [PubMed] [Google Scholar]
- Greenstein A. J., Sachar D. B., Pasternack B. S., Janowitz H. D. Reoperation and recurrence in Crohn's colitis and ileocolitis Crude and cumulative rates. N Engl J Med. 1975 Oct 2;293(14):685–690. doi: 10.1056/NEJM197510022931403. [DOI] [PubMed] [Google Scholar]
- Greenstein A. J., Sachar D., Pucillo A., Kreel I., Geller S., Janowitz H. D., Aufses A., Jr Cancer in Crohn's disease after diversionary surgery. A report of seven carcinomas occurring in excluded bowel. Am J Surg. 1978 Jan;135(1):86–90. doi: 10.1016/0002-9610(78)90015-6. [DOI] [PubMed] [Google Scholar]
- Homan W. P., Dineen P. Comparison of the results of resection, bypass, and bypass with exclusion for ileocecal Crohn's disease. Ann Surg. 1978 May;187(5):530–535. doi: 10.1097/00000658-197805000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koudahl G., Kristensen M., Lenz K. Bypass compared with resection for ileal Crohn's disease. Scand J Gastroenterol. 1974;9(2):203–206. [PubMed] [Google Scholar]
- Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep. 1966 Mar;50(3):163–170. [PubMed] [Google Scholar]
- Mekhjian H. S., Switz D. M., Watts H. D., Deren J. J., Katon R. M., Beman F. M. National Cooperative Crohn's Disease Study: factors determining recurrence of Crohn's disease after surgery. Gastroenterology. 1979 Oct;77(4 Pt 2):907–913. [PubMed] [Google Scholar]
- Nesbit R. R., Jr, Elbadawi N. A., Morton J. H., Cooper R. A., Jr Carcinoma of the small bowel. A complication of regional enteritis. Cancer. 1976 Jun;37(6):2948–2959. doi: 10.1002/1097-0142(197606)37:6<2948::aid-cncr2820370652>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Stone W., Veidenheimer M. C., Corman M. L., Coller J. A. The dilemma of Crohn's disease: long-term follow-up of Crohn's disease of the small intestine. Dis Colon Rectum. 1977 Jul-Aug;20(5):372–376. doi: 10.1007/BF02587362. [DOI] [PubMed] [Google Scholar]



