Abstract
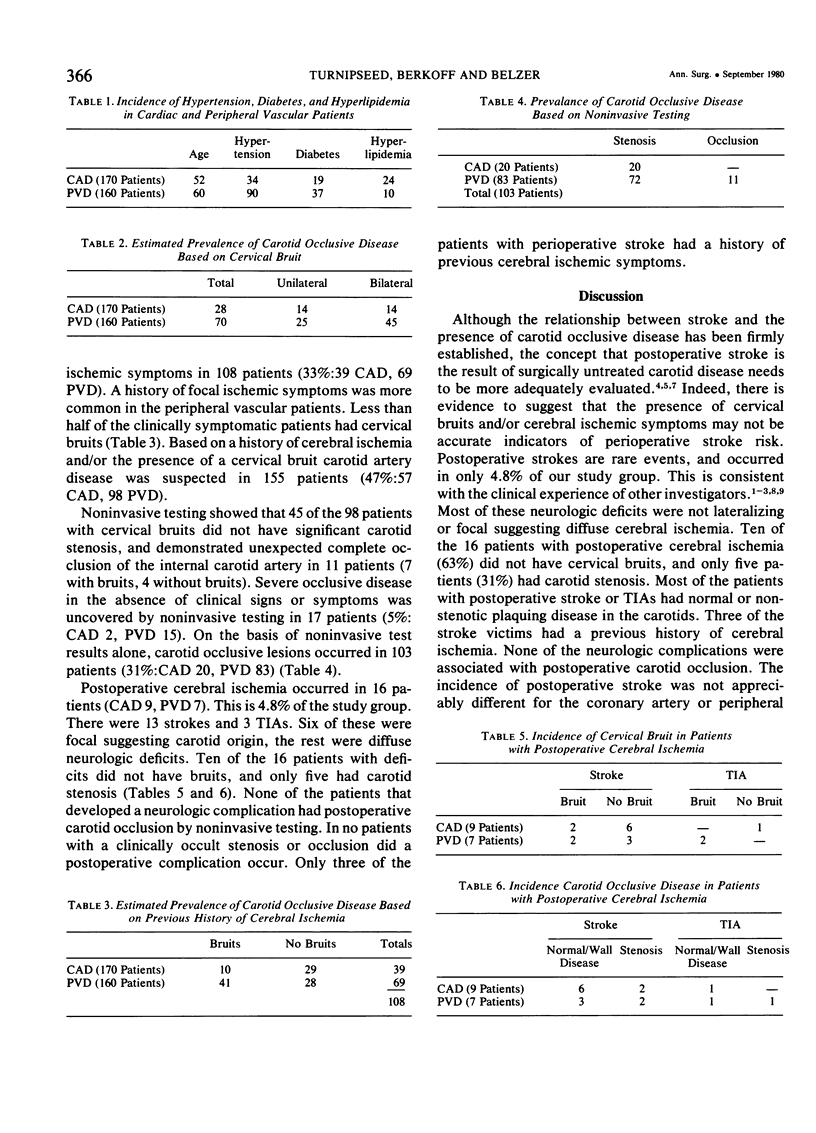
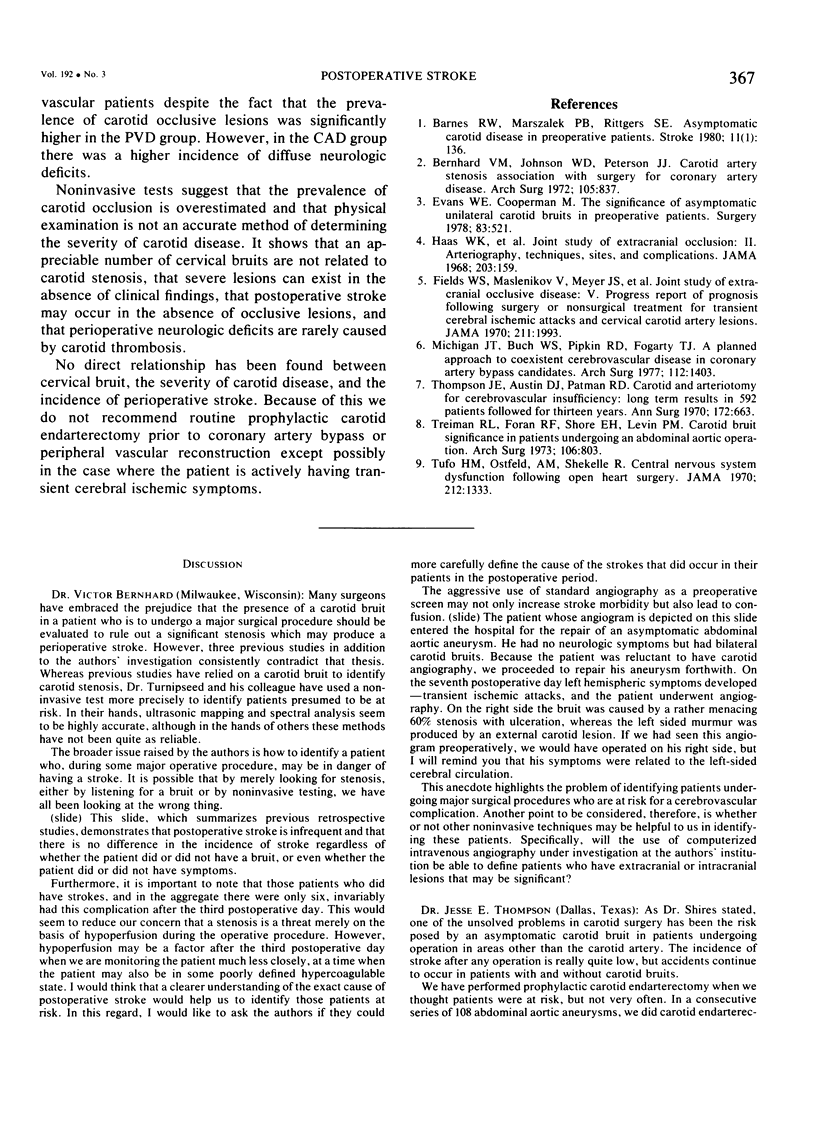
The postoperative stroke rate in 330 patients requiring coronary artery (170) or peripheral vascular (160) surgery was compared with the presence of carotid bruits and the results of noninvasive screening (Doppler imaging and spectral analysis of flow) to determine prevalence and significance of carotid lesions) and their relationship to perioperative stroke. Carotid lesions were suspected because of bruits in 70 patients with peripheral vascular disease (PVD) and in 28 patients with coronary artery disease (CAD). Noninvasive tests showed high grade stenosis or occlusion in 62 patients with PVD and in 14 with CAD. Forty-four patients with PVD and 101 patients with CAD had normal Doppler studies. The rest in both groups had plaquing without major stenosis. Noninvasive tests uncovered severe, occult lesions in only 13 patients (9 PVD, 4 CAD). Postoperative neurologic complications occurred in 16 patients (13 strokes: 5 PVD, 8 CAD and 3 TIAs: 2 PVD, 1 CAD). Thirteen neurologic complications occurred in patients having nonstenotic plaques or normal carotids without bruits. Only three of the strokes and 1 TIA occurred in patients with bruits and detectable carotid stenosis. Few of the postoperative strokes or TIAs were focal (2 PVD, 1 CAD), and the rest were nonfocal. None of the postoperative strokes or TIAs were associated with postoperative carotid occlusion. Physical examination is not an accurate method of determining severity of carotid disease. Severe carotid stenosis is more common in PVD patients than in CAD patients, but there is no significant difference in postoperative stroke rate. No direct relationship has been found between a bruit, severity of disease, and incidence of perioperative stroke.
Full text
PDF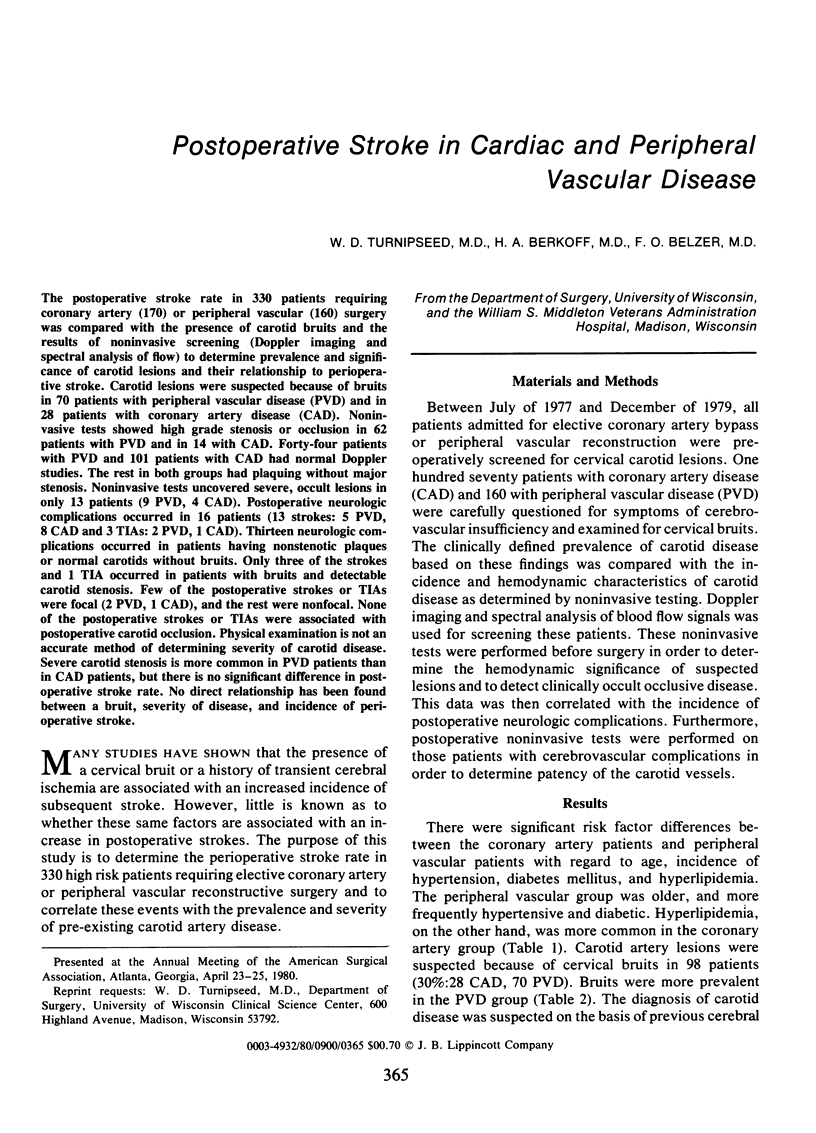
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bernhard V. M., Johnson W. D., Peterson J. J. Carotid artery stenosis. Association with surgery for coronary artery disease. Arch Surg. 1972 Dec;105(6):837–840. doi: 10.1001/archsurg.1972.04180120018005. [DOI] [PubMed] [Google Scholar]
- Fields W. S., Maslenikov V., Meyer J. S., Hass W. K., Remington R. D., Macdonald M. Joint study of extracranial arterial occlusion. V. Progress report of prognosis following surgery or nonsurgical treatment for transient cerebral ischemic attacks and cervical carotid artery lesions. JAMA. 1970 Mar 23;211(12):1993–2003. doi: 10.1001/jama.211.12.1993. [DOI] [PubMed] [Google Scholar]
- Mehigan J. T., Buch W. S., Pipkin R. D., Fogarty T. J. A planned approach to coexistent cerebrovascular disease in coronary artery bypass candidates. Arch Surg. 1977 Nov;112(11):1403–1409. doi: 10.1001/archsurg.1977.01370110137016. [DOI] [PubMed] [Google Scholar]
- Thompson J. E., Austin D. J., Patman R. D. Carotid endarterectomy for cerebrovascular insufficiency: long-term results in 592 patients followed up to thirteen years. Ann Surg. 1970 Oct;172(4):663–679. doi: 10.1097/00000658-197010000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treiman R. L., Foran R. F., Shore E. H., Levin P. M. Carotid bruit. Significance in patients undergoing an abdominal aortic operation. Arch Surg. 1973 Jun;106(6):803–805. doi: 10.1001/archsurg.1973.01350180041013. [DOI] [PubMed] [Google Scholar]
- Tufo H. M., Ostfeld A. M., Shekelle R. Central nervous system dysfunction following open-heart surgery. JAMA. 1970 May 25;212(8):1333–1340. [PubMed] [Google Scholar]


