Abstract
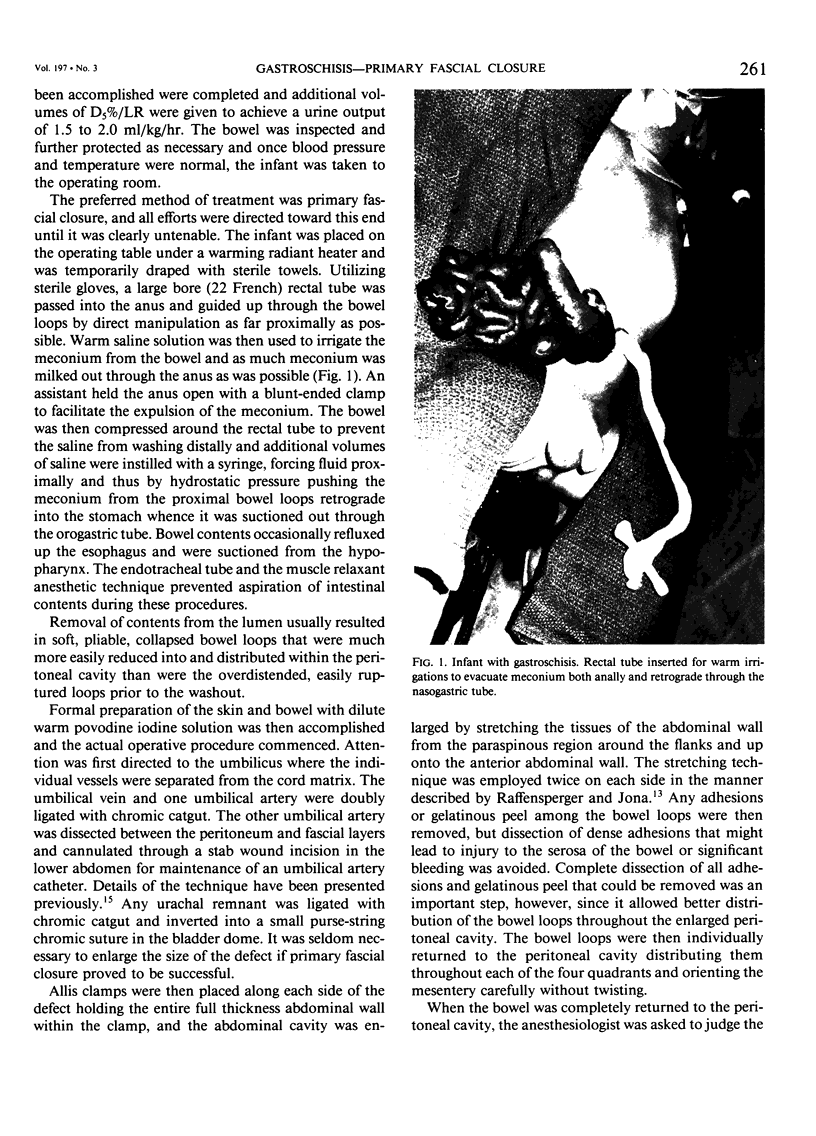
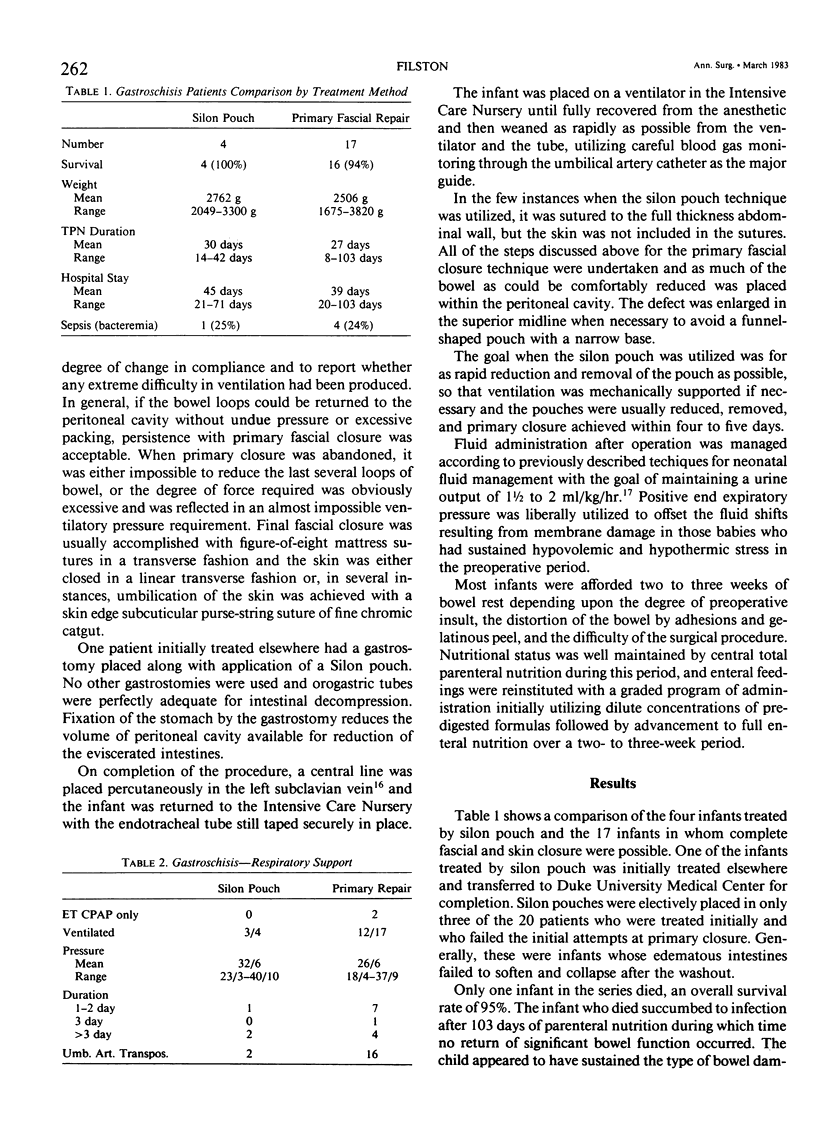
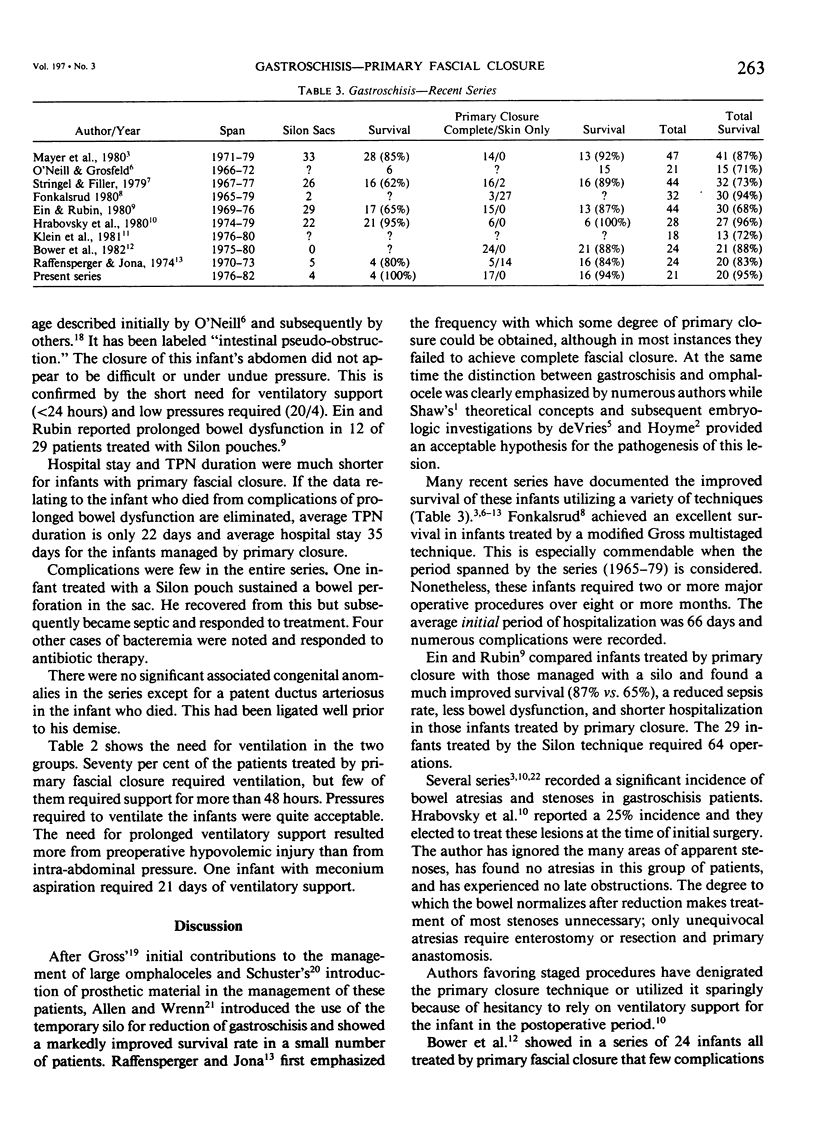
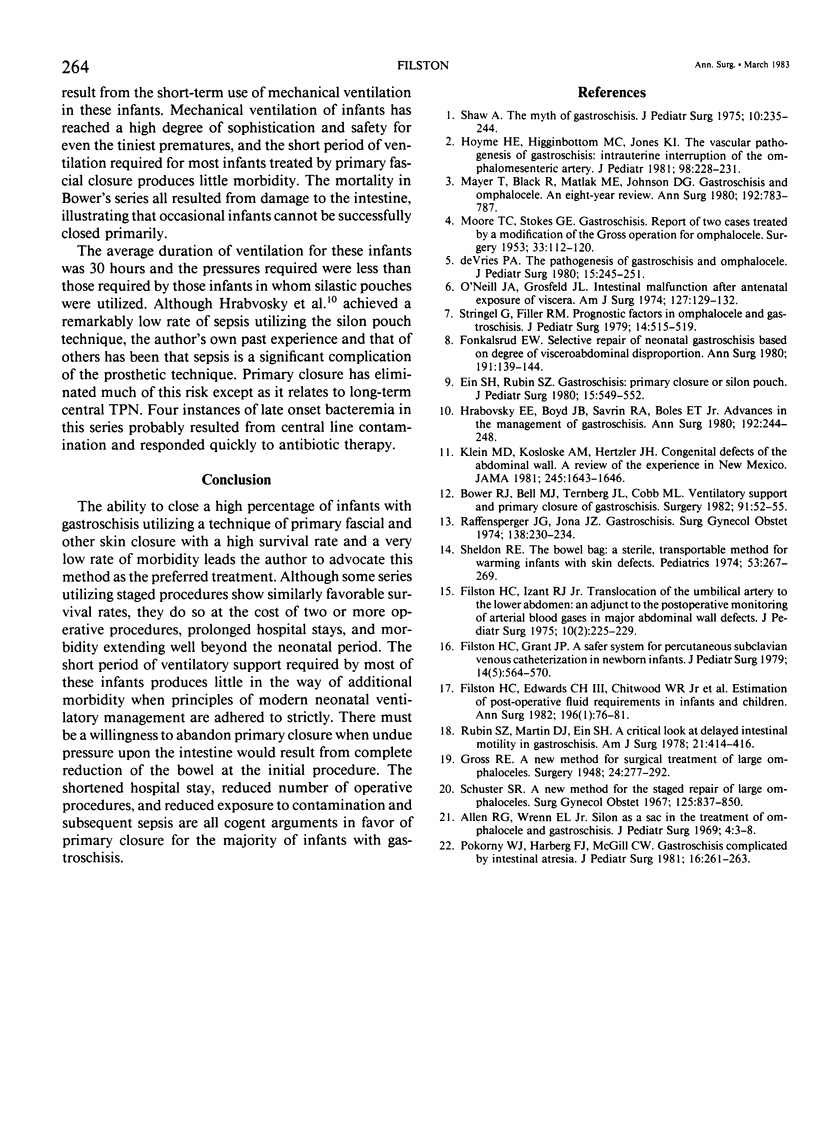
Since Raffensperger and Jona reported an 80% success rate with primary skin closure including a 16% rate of complete fascial closure in 24 patients with gastroschisis in 1974, primary fascial closure has been the author's preferred method. It has been possible to achieve complete fascial and skin closure in 17 of the last 21 patients (81%). Four infants in this series, one of whom was initially managed by another surgeon, were treated with brief application of a silon prosthesis with subsequent reduction and closure. The two keys to success of this method are thorough wash out of the meconium from the entire intestine and vigorous stretching of the abdominal wall. Assisted ventilation may be needed for 24 to 48 hours after operation and has been well tolerated. Transposition of an umbilical artery for cannulation and blood gas monitoring has been an important adjunct. The one death (5% mortality) resulted from prolonged bowel dysfunction and liver failure three months after operation. Other complications have been few and mild. Since some recent reports have indicated that primary closure is not being widely used in the treatment of gastroschisis, this series is presented to emphasize that this method can be used in most infants and with a very low complication rate.
Full text
PDF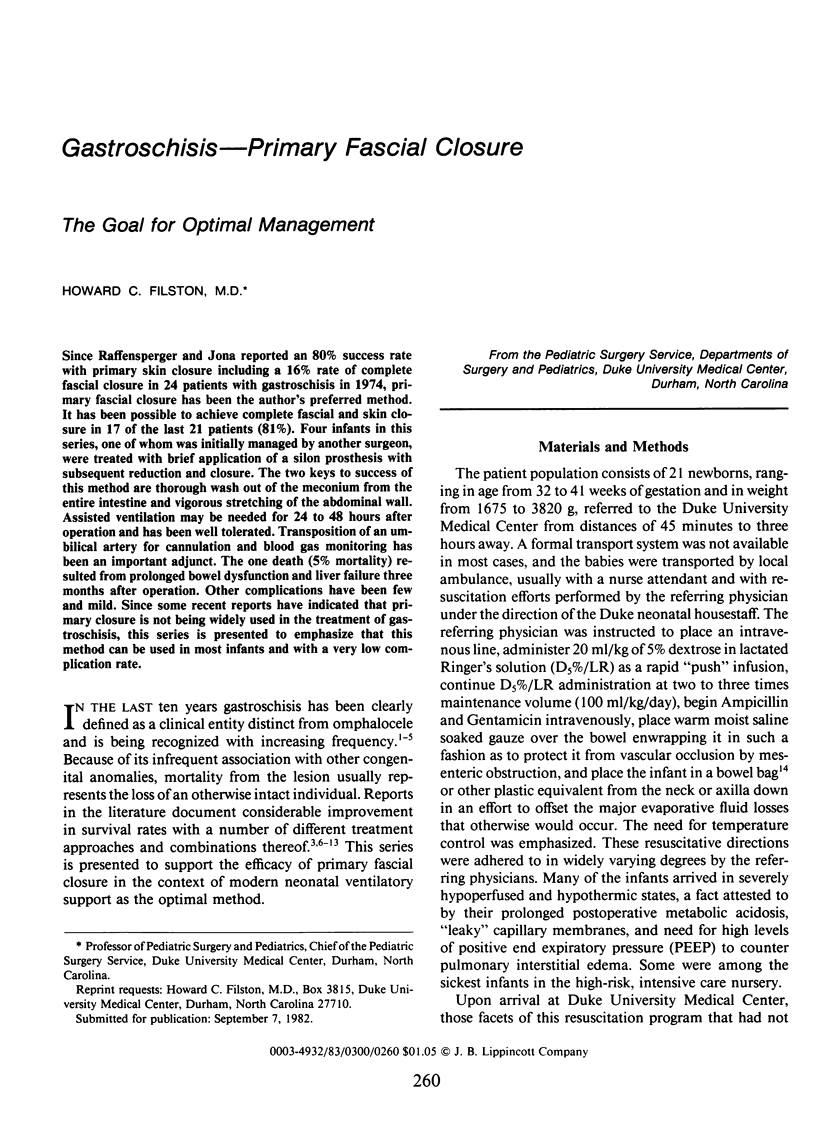
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allen R. G., Wrenn E. L., Jr Silon as a sac in the treatment of omphalocele and gastroschisis. J Pediatr Surg. 1969 Feb;4(1):3–8. doi: 10.1016/0022-3468(69)90177-8. [DOI] [PubMed] [Google Scholar]
- Bower R. J., Bell M. J., Ternberg J. L., Cobb M. L. Ventilatory support and primary closure of gastroschisis. Surgery. 1982 Jan;91(1):52–55. [PubMed] [Google Scholar]
- Ein S. H., Rubin S. Z. Gastroschisis: primary closure or Silon pouch. J Pediatr Surg. 1980 Aug;15(4):549–552. doi: 10.1016/s0022-3468(80)80771-8. [DOI] [PubMed] [Google Scholar]
- Filston H. C., Edwards C. H., 3rd, Chitwood W. R., Jr, Larson R. M., Marsicano T. H., Hill R. C. Estimation of postoperative fluid requirements in infants and children. Ann Surg. 1982 Jul;196(1):76–81. doi: 10.1097/00000658-198207000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filston H. C., Grant J. P. A safer system for percutaneous subclavian venous catheterization in newborn infants. J Pediatr Surg. 1979 Oct;14(5):564–570. doi: 10.1016/s0022-3468(79)80141-4. [DOI] [PubMed] [Google Scholar]
- Filston H. C., Izant R. J. Translocation of the umbilical artery to the lower abdomen: an adjunct to the postoperative monitoring of arterial blood gases in major abdominal wall defects. J Pediatr Surg. 1975 Apr;10(2):225–229. doi: 10.1016/0022-3468(75)90283-3. [DOI] [PubMed] [Google Scholar]
- Fonkalsrud E. W. Selective repair of neonatal gastroschisis based on degree of visceroabdominal disproportion. Ann Surg. 1980 Feb;191(2):139–144. doi: 10.1097/00000658-198002000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyme H. E., Higginbottom M. C., Jones K. L. The vascular pathogenesis of gastroschisis: intrauterine interruption of the omphalomesenteric artery. J Pediatr. 1981 Feb;98(2):228–231. doi: 10.1016/s0022-3476(81)80640-3. [DOI] [PubMed] [Google Scholar]
- Hrabovsky E. E., Boyd J. B., Savrin R. A., Boles E. T., Jr Advances in the management of gastroschisis. Ann Surg. 1980 Aug;192(2):244–248. doi: 10.1097/00000658-198008000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein M. D., Kosloske A. M., Hertzler J. H. Congenital defects of the abdominal wall. A review of the experience in New Mexico. JAMA. 1981 Apr 24;245(16):1643–1646. [PubMed] [Google Scholar]
- MOORE T. C., STOKES G. E. Gastroschisis; report of two cases treated by a modification of the gross operation for omphalocele. Surgery. 1953 Jan;33(1):112–120. [PubMed] [Google Scholar]
- Mayer T., Black R., Matlak M. E., Johnson D. G. Gastroschisis and omphalocele. An eight-year review. Ann Surg. 1980 Dec;192(6):783–787. doi: 10.1097/00000658-198012000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Niell J. A., Jr, Grosfeld J. L. Intestinal malfunction after antenatal exposure of viscera. Am J Surg. 1974 Feb;127(2):129–132. doi: 10.1016/0002-9610(74)90147-0. [DOI] [PubMed] [Google Scholar]
- Pokorny W. J., Harberg F. J., McGill C. W. Gastroschisis complicated by intestinal atresia. J Pediatr Surg. 1981 Jun;16(3):261–263. doi: 10.1016/s0022-3468(81)80676-8. [DOI] [PubMed] [Google Scholar]
- Raffensperger J. G., Jona J. Z. Gastroschisis. Surg Gynecol Obstet. 1974 Feb;138(2):230–234. [PubMed] [Google Scholar]
- Rubin S. Z., Martin D. J., Ein S. H. A critical look at delayed intestinal motility in gastroschisis. Can J Surg. 1978 Sep;21(5):414–416. [PubMed] [Google Scholar]
- Schuster S. R. A new method for the staged repair of large omphaloceles. Surg Gynecol Obstet. 1967 Oct;125(4):837–850. [PubMed] [Google Scholar]
- Shaw A. The myth of gastroschisis. J Pediatr Surg. 1975 Apr;10(2):235–244. doi: 10.1016/0022-3468(75)90285-7. [DOI] [PubMed] [Google Scholar]
- Sheldon R. E. The bowel bag: a sterile, transportable method for warming infants with skin defects. Pediatrics. 1974 Feb;53(2):267–269. [PubMed] [Google Scholar]
- Stringel G., Filler R. M. Prognostic factors in omphalocele and gastroschisis. J Pediatr Surg. 1979 Oct;14(5):515–519. doi: 10.1016/s0022-3468(79)80128-1. [DOI] [PubMed] [Google Scholar]
- deVries P. A. The pathogenesis of gastroschisis and omphalocele. J Pediatr Surg. 1980 Jun;15(3):245–251. doi: 10.1016/s0022-3468(80)80130-8. [DOI] [PubMed] [Google Scholar]