Abstract
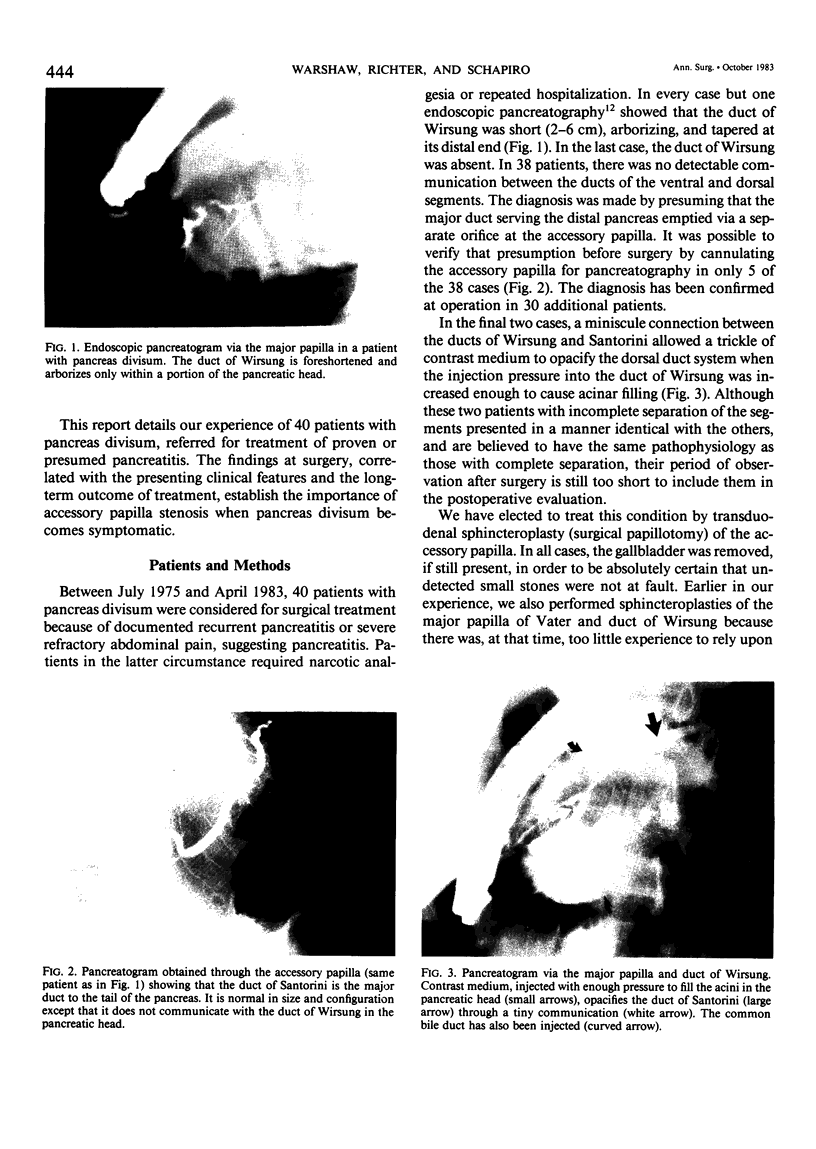
Recurrent pancreatitis is more prevalent in the 4% of people with pancreas divisum (nonfused dorsal and ventral ducts), and it has been proposed that the pancreatitis is caused by stenosis at the orifice of the dorsal duct. We have treated 40 patients with pancreas divisum and proven or probable pancreatitis. The diagnoses were made by endoscopic pancreatography showing a foreshortened (less than 6 cm) ventral duct (Wirsung) and confirmed by postoperative pancreatograms showing the separate main duct (Santorini) emptying via the accessory papilla. Of these, 32 patients (25 men, 7 women, median age 30) had recurrent acute pancreatitis (22) or persistent pain (10) without chronic inflammation or fibrosis. Twenty-nine have been treated by transduodenal sphincteroplasty of the accessory papilla; 22 were stenotic (0.75 mm or less) and 7 nonstenotic. Among 25 patients observed for longer than 6 months after surgery, the relief of pain and pancreatitis has been good in 17, fair in 1, and poor in 7. There was no difference between accessory papillotomy alone (10-0-3) v papillotomies of both accessory and major papillae (7-1-4). Patients with stenosis (16-1-1) fared better (p less than 0.001) than those without stenosis (1-0-6). Those presenting with discrete attacks (12-1-2) also fared better (p less than 0.05) than those presenting with chronic pain (5-0-5). The other eight patients (two women, six men, median age 28) had chronic pancreatitis proven by pancreatography and surgical biopsy. In this group, treatment by sphincteroplasty of the accessory papilla failed, and seven patients eventually required a pancreaticojejunostomy (3), distal pancreatectomy (2), or total pancreatectomy (2). In pancreas divisum, pancreatitis is caused by stenosis at the accessory papilla of Santorini. There may be progression from recurrent acute pancreatitis to irreversible fibrosis in some cases. Sphincteroplasty is effective for recurrent acute pancreatitis, but ductal drainage or resection becomes necessary once chronic pancreatitis is established. A preoperative test for stenosis of the accessory papilla is needed to identify patients whose symptoms are genuinely caused by their pancreas divisum.
Full text
PDF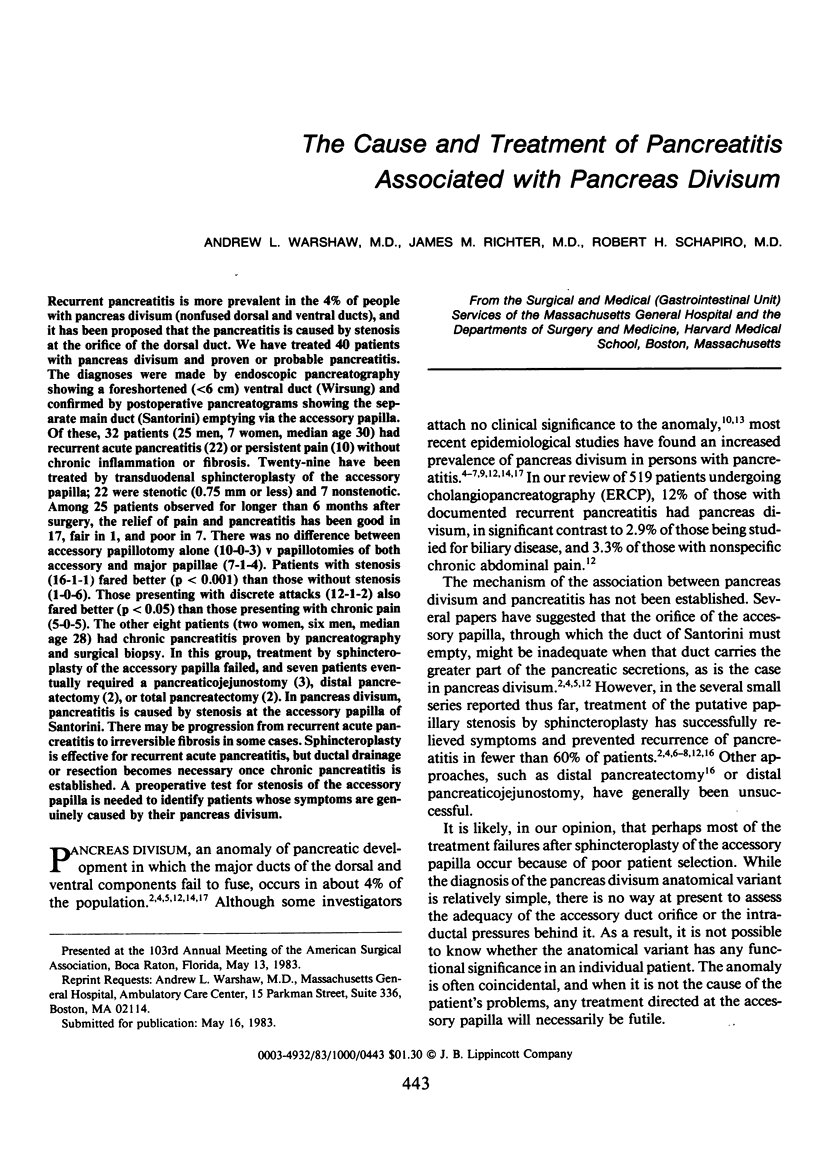


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cooperman M., Ferrara J. J., Fromkes J. J., Carey L. C. Surgical management of pancreas divisum. Am J Surg. 1982 Jan;143(1):107–112. doi: 10.1016/0002-9610(82)90138-6. [DOI] [PubMed] [Google Scholar]
- Cotton P. B. Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut. 1980 Feb;21(2):105–114. doi: 10.1136/gut.21.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregg J. A., Monaco A. P., McDermott W. V. Pancreas divisum. Results of surgical intervention. Am J Surg. 1983 Apr;145(4):488–492. doi: 10.1016/0002-9610(83)90045-4. [DOI] [PubMed] [Google Scholar]
- Gregg J. A. Pancreas divisum: its association with pancreatitis. Am J Surg. 1977 Nov;134(5):539–543. doi: 10.1016/0002-9610(77)90429-9. [DOI] [PubMed] [Google Scholar]
- Heiss F. W., Shea J. A. Association of pancreatitis and variant ductal anatomy: dominant drainage of the duct of Santorini. Am J Gastroenterol. 1978 Aug;70(2):158–162. [PubMed] [Google Scholar]
- Keith R. G., Shapero T. F., Saibil F. G. Treatment of pancreatitis associated with pancreas divisum by dorsal duct sphincterotomy alone. Can J Surg. 1982 Nov;25(6):622–626. [PubMed] [Google Scholar]
- Mitchell C. J., Lintott D. J., Ruddell W. S., Losowsky M. S., Axon A. T. Clinical relevance of an unfused pancreatic duct system. Gut. 1979 Dec;20(12):1066–1071. doi: 10.1136/gut.20.12.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter J. M., Schapiro R. H., Mulley A. G., Warshaw A. L. Association of pancreas divisum and pancreatitis, and its treatment by sphincteroplasty of the accessory ampulla. Gastroenterology. 1981 Dec;81(6):1104–1110. [PubMed] [Google Scholar]
- Rösch W., Koch H., Schaffner O., Demling L. The clinical significance of the pancreas divisum. Gastrointest Endosc. 1976 May;22(4):206–207. doi: 10.1016/s0016-5107(76)73755-6. [DOI] [PubMed] [Google Scholar]
- Sahel J., Cros R. C., Bourry J., Sarles H. Clinico-pathological conditions associated with pancreas divisum. Digestion. 1982;23(1):1–8. doi: 10.1159/000198689. [DOI] [PubMed] [Google Scholar]
- Shapero T. F., Keith R. G. Pancreatitis and pancreas divisum. Gastroenterology. 1982 Jul;83(1 Pt 1):158–158. [PubMed] [Google Scholar]
- Tulassay Z., Papp J. New clinical aspects of pancreas divisum. Gastrointest Endosc. 1980 Nov;26(4):143–146. doi: 10.1016/s0016-5107(80)73305-9. [DOI] [PubMed] [Google Scholar]
- Warshaw A. L., Popp J. W., Jr, Schapiro R. H. Long-term patency, pancreatic function, and pain relief after lateral pancreaticojejunostomy for chronic pancreatitis. Gastroenterology. 1980 Aug;79(2):289–293. [PubMed] [Google Scholar]