Abstract
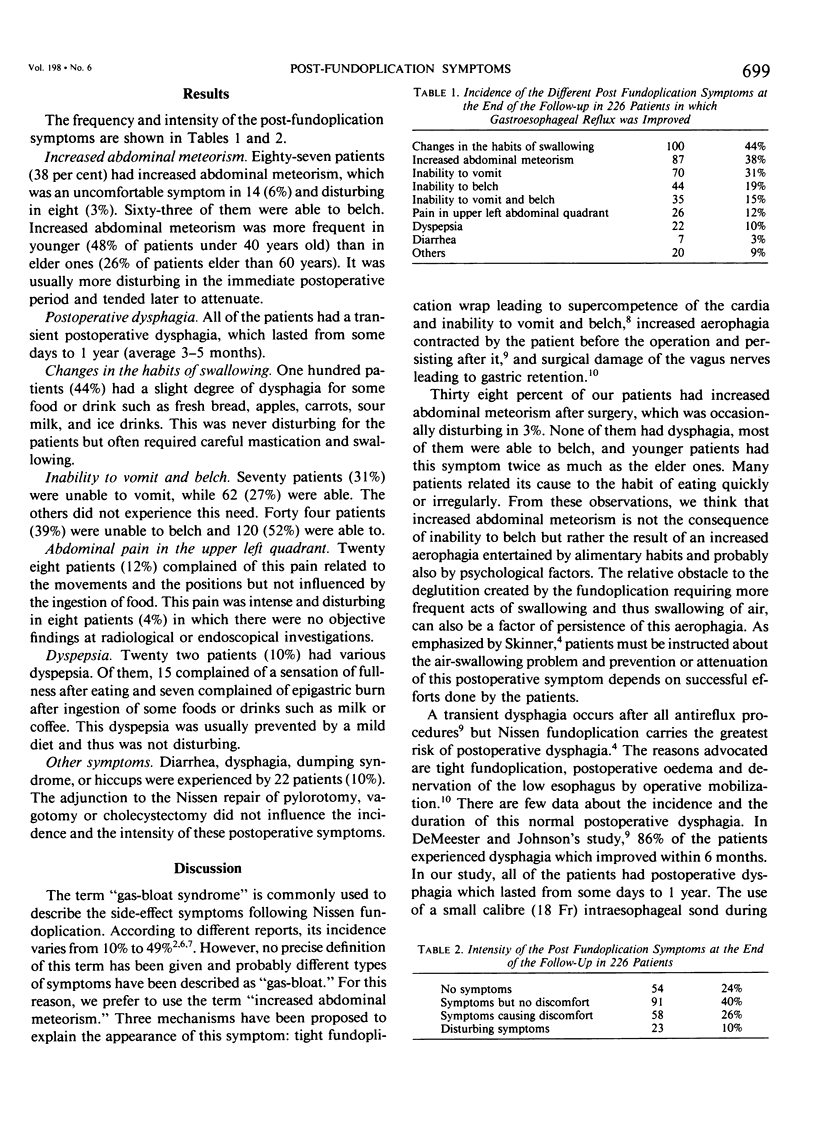
The post-fundoplication symptoms were assessed in 226 patients who had symptomatical improvement of gastroesophageal reflux after Nissen fundoplication. Follow-up range was from 3 to 12 years (average 5,6 years). Of these patients, 24% were totally asymptomatic. All had transient postoperative dysphagia which improved within an average of 3-5 months. Forty four per cent had changes in habits of swallowing; 38% had increased abdominal meteorism; 31% were unable to vomit and 19% unable to belch; 12% had pain in the upper left abdominal quadrant; and 10% had dyspepsia. These symptoms were uncomfortable in 26% and disturbing in 10%. Diverse causes can be responsible for these symptoms; mechanical (narrowing of the cardia, postoperative adherences), functional (motor troubles, denervation), and depending of the patients (alimentary habits). The high frequency of post-fundoplication symptoms restrict clearly the success of Nissen fundoplication.
Full text
PDF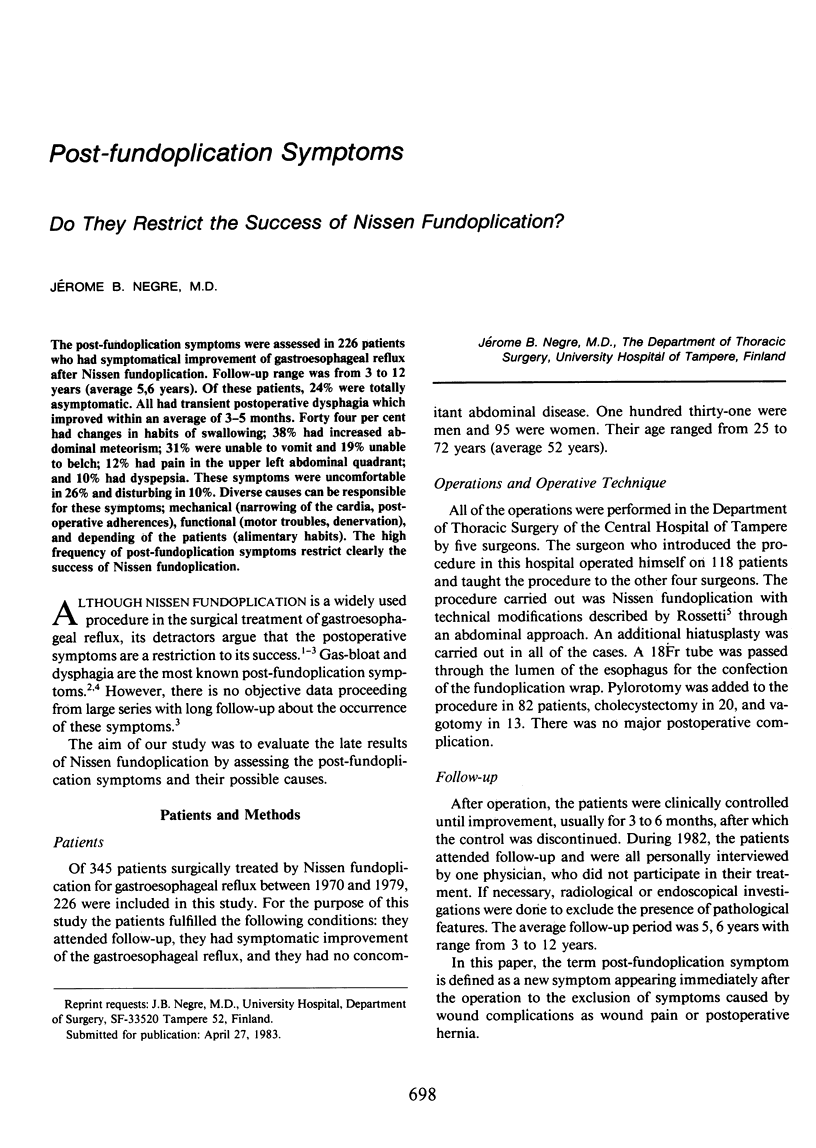
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belsey R. H. Gastroesophageal reflux. Am J Surg. 1980 Jun;139(6):775–781. doi: 10.1016/0002-9610(80)90382-7. [DOI] [PubMed] [Google Scholar]
- Bushkin F. L., Neustein C. L., Parker T. H., Woodward E. R. Nissen fundoplication for reflux peptic esophagitis. Ann Surg. 1977 Jun;185(6):672–677. doi: 10.1097/00000658-197706000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demeester T. R., Johnson L. F., Kent A. H. Evaluation of current operations for the prevention of gastroesophageal reflux. Ann Surg. 1974 Oct;180(4):511–525. doi: 10.1097/00000658-197410000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill L. D. Progress in the surgical management of hiatal hernia. World J Surg. 1977 Jul;1(4):425–436. doi: 10.1007/BF01565905. [DOI] [PubMed] [Google Scholar]
- Rossetti M., Hell K. Fundoplication for the treatment of gastroesophageal reflux in hiatal hernia. World J Surg. 1977 Jul;1(4):439–443. doi: 10.1007/BF01565907. [DOI] [PubMed] [Google Scholar]
- Siewert J. R., Blum A. L. The oesophagus. Part I: Surgery at the upper oesophageal sphincter, tubular oesophagus and lower oesophageal sphincter. Clin Gastroenterol. 1979 May;8(2):271–291. [PubMed] [Google Scholar]
- Skinner D. B. Complications of surgery for gastroesophageal reflux. World J Surg. 1977 Jul;1(4):485–490. doi: 10.1007/BF01565918. [DOI] [PubMed] [Google Scholar]
- Vansant J. H., Baker J. W., Jr Complications of vagotomy in the treatment of hiatal hernia. Ann Surg. 1976 Jun;183(6):629–635. doi: 10.1097/00000658-197606000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward E. R. Surgical treatment of gastroesophageal reflux and its complications. World J Surg. 1977 Jul;1(4):453–460. doi: 10.1007/BF01565911. [DOI] [PubMed] [Google Scholar]
- Woodward E. R., Thomas H. F., McAlhany J. C. Comparison of crural repair and Nissen fundoplication in the treatment of esophageal hiatus hernia with peptic esophagitis. Ann Surg. 1971 May;173(5):782–792. doi: 10.1097/00000658-197105000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]


