Abstract
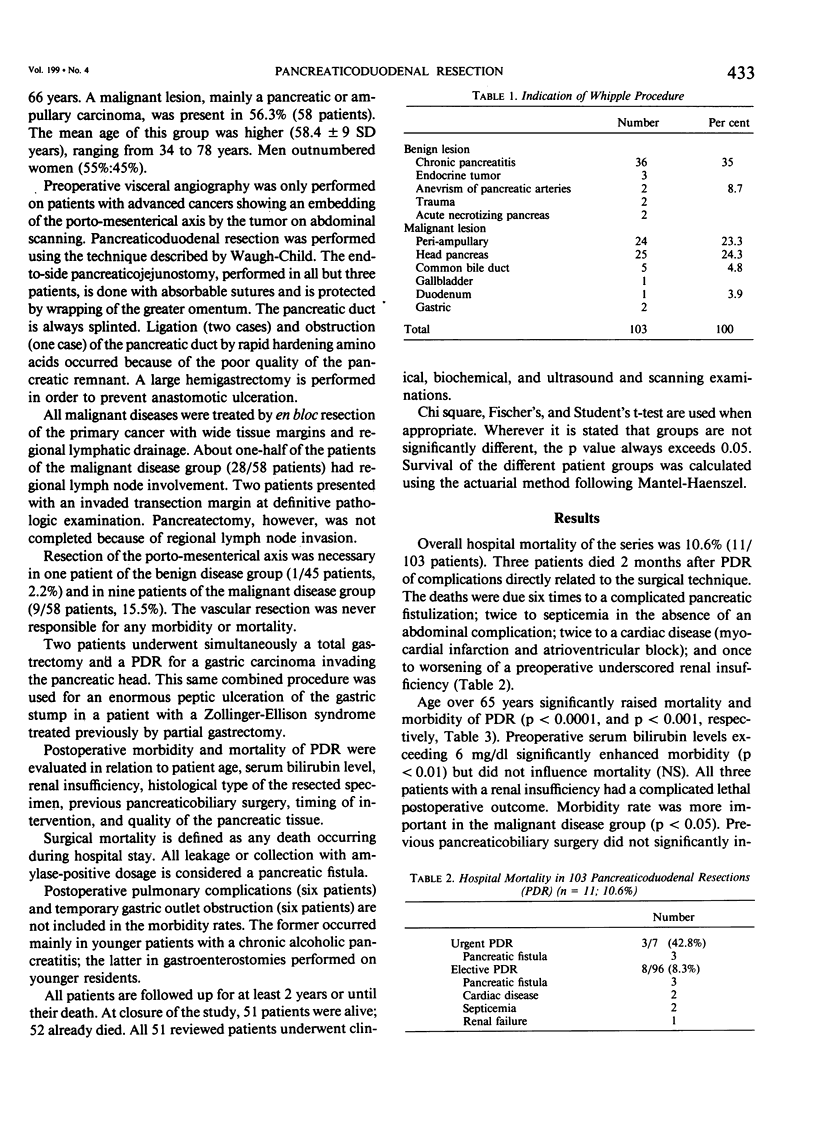
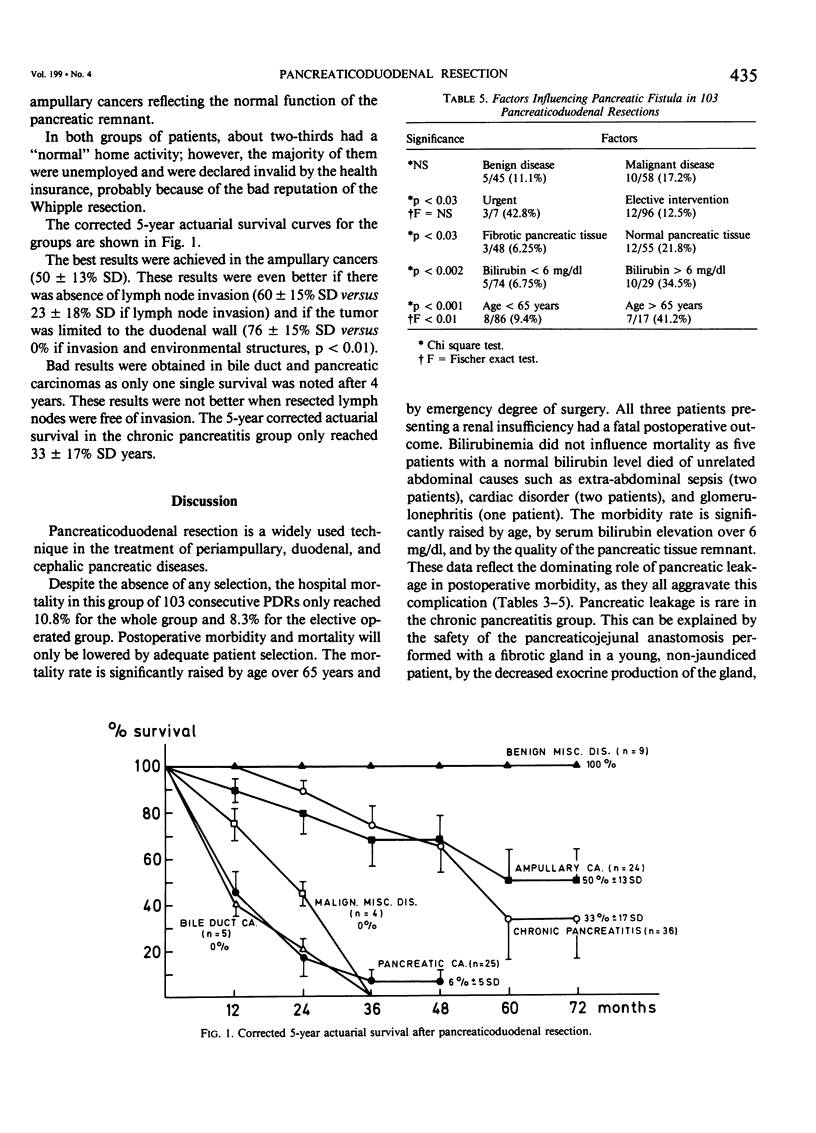
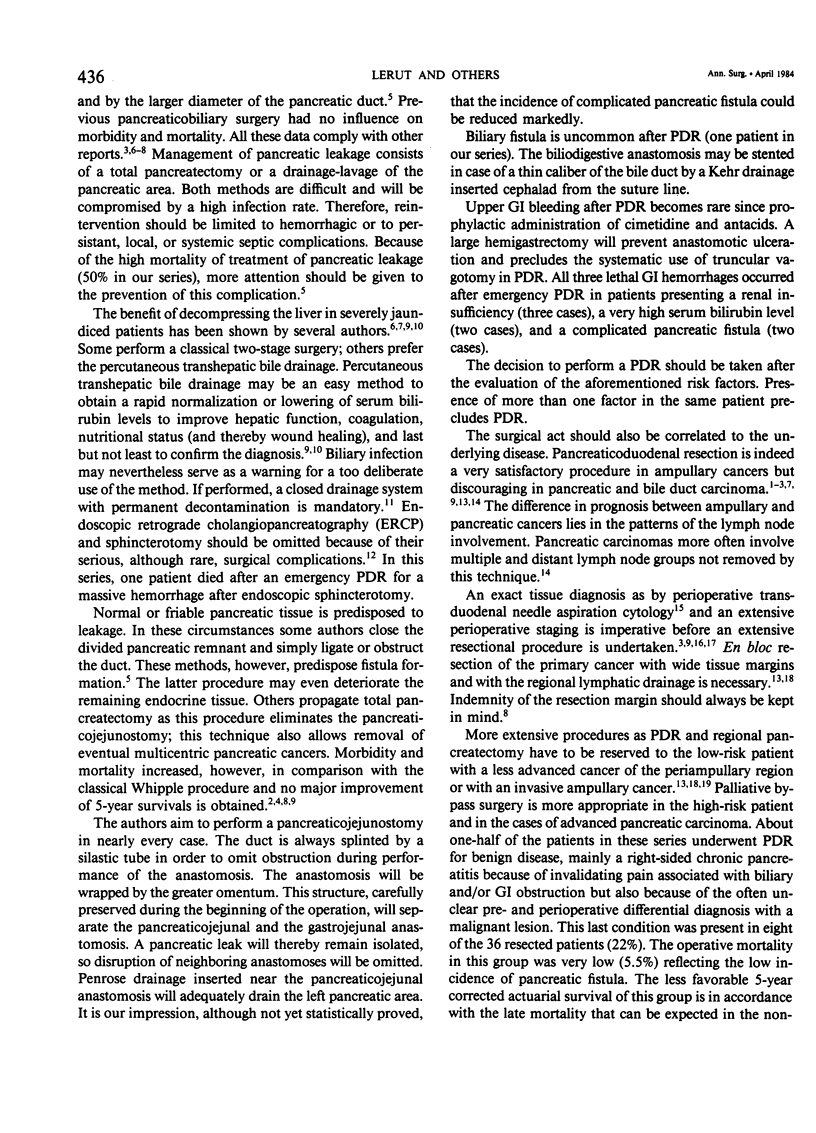
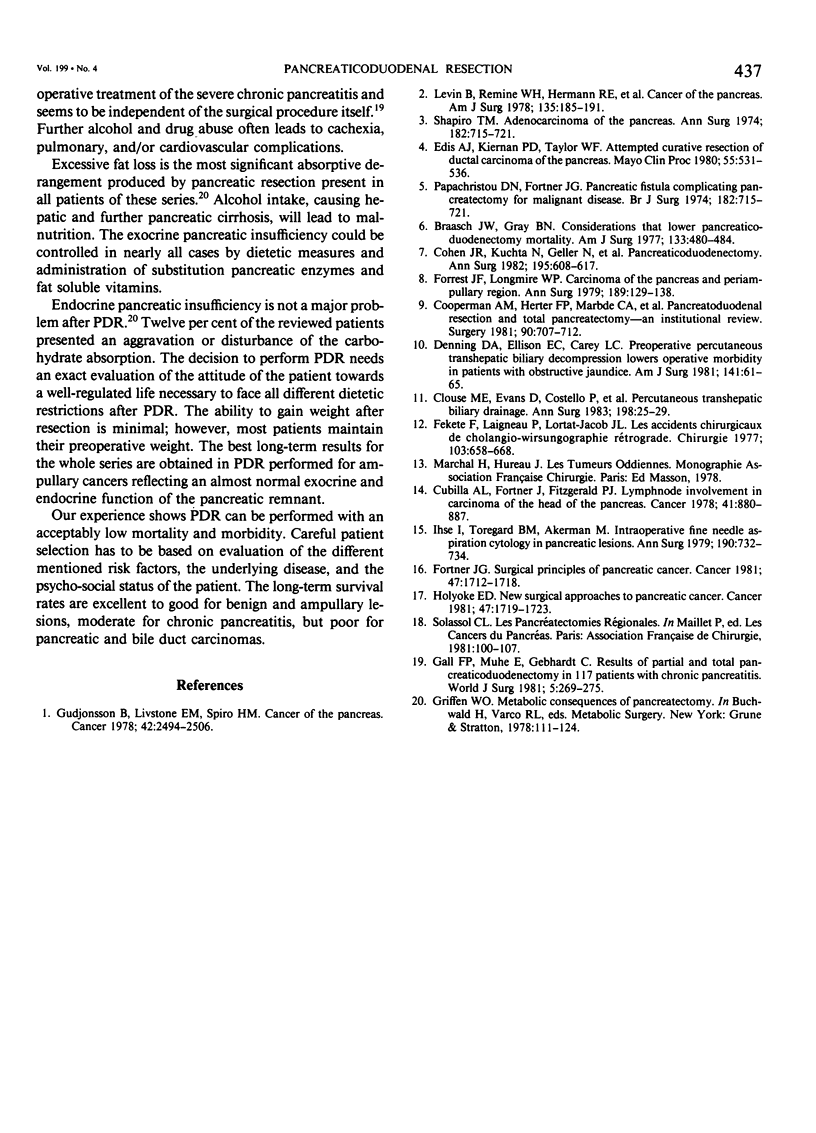
From an institutional review of 103 pancreaticoduodenal resections (PDRs) performed during the period 1968-1981, risk factors and selection criteria of this procedure were evaluated. A total of 43.7% of the patients were operated on for benign lesions, mainly right-sided chronic pancreatitis (35%); 56.3% of the interventions were performed for malignant disease, mainly carcinoma of the periampullary region. Despite the absence of any selection, the hospital mortality in 103 consecutive PDRs only reached 10.6% for the whole group (11/103 patients) and 8.3% for the elective group (8/96 patients). Mortality was significantly influenced by age barrier over 65 years (p less than 0.0001) and by urgent degree of surgery (p less than 0.03). All three patients with renal insufficiency had a fatal outcome after PDR. A total of 19.4% of the patients (20/103 patients) developed a surgical complication. The most important complication was pancreatic fistula (15/103 patients, 14.5%) responsible for all digestive-related fatal outcomes (six patients). Surgical treatment of pancreatic fistula (10 patients) is compromised by a high morbidity and a high mortality rate (50%). Postoperative morbidity as well as the incidence of the pancreatic fistula were significantly influenced by the age of the patients over 65 years (p less than 0.01 and less than 0.001, respectively), and by the serum bilirubin level over 6 mg/dl (p less than 0.002). The poor quality of the pancreatic tissue (p less than 0.03) and the urgent degree of the intervention (p less than 0.03) also raised the incidence of pancreatic leakage. Morbidity rate was more important in the malignant disease group (p less than 0.05). Corrected 5-year actuarial survival after PDR is excellent for ampullary cancer, moderate for chronic pancreatitis, and extremely poor for pancreatic and bile duct carcinoma. The decision to perform PDR should be taken after evaluation of the aforementioned risk factors: the emergency, age, serum bilirubin, quality of pancreatic tissue and renal insufficiency, underlying disease, and psycho-social status of the patient.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Braasch J. W., Gray B. N. Considerations that lower pancreatoduodenectomy mortality. Am J Surg. 1977 Apr;133(4):480–484. doi: 10.1016/0002-9610(77)90135-0. [DOI] [PubMed] [Google Scholar]
- Clouse M. E., Evans D., Costello P., Alday M., Edwards S. A., McDermott W. V., Jr Percutaneous transhepatic biliary drainage. Complications due to multiple duct obstructions. Ann Surg. 1983 Jul;198(1):25–29. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. R., Kuchta N., Geller N., Shires G. T., Dineen P. Pancreaticoduodenectomy. A 40-year experience. Ann Surg. 1982 May;195(5):608–617. doi: 10.1097/00000658-198205000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooperman A. M., Herter F. P., Marboe C. A., Helmreich Z. V., Perzin K. H. Pancreatoduodenal resection and total pnacreatectomy--an institutional review. Surgery. 1981 Oct;90(4):707–712. [PubMed] [Google Scholar]
- Cubilla A. L., Fortner J., Fitzgerald P. J. Lymph node involvement in carcinoma of the head of the pancreas area. Cancer. 1978 Mar;41(3):880–887. doi: 10.1002/1097-0142(197803)41:3<880::aid-cncr2820410315>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Denning D. A., Ellison E. C., Carey L. C. Preoperative percutaneous transhepatic biliary decompression lowers operative morbidity in patients with obstructive jaundice. Am J Surg. 1981 Jan;141(1):61–65. doi: 10.1016/0002-9610(81)90013-1. [DOI] [PubMed] [Google Scholar]
- Edis A. J., Kiernan P. D., Taylor W. F. Attempted curative resection of ductal carcinoma of the pancreas: review of Mayo Clinic experience, 1951-1975. Mayo Clin Proc. 1980 Sep;55(9):531–536. [PubMed] [Google Scholar]
- Fekete F., Laigneau P., Lortat-Jacob J. L. Les accidents chirugicaux de la cholangio-wirsungographie rétrograde (C.W.R.). A propos de 24 cas. Chirurgie. 1977 Jun;103(8):658–668. [PubMed] [Google Scholar]
- Forrest J. F., Longmire W. P., Jr Carcinoma of the pancreas and periampullary region. Ann Surg. 1979 Feb;189(2):129–138. doi: 10.1097/00000658-197902000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortner J. G. Surgical principles for pancreatic cancer: regional total and subtotal pancreatectomy. Cancer. 1981 Mar 15;47(6 Suppl):1712–1718. doi: 10.1002/1097-0142(19810315)47:6+<1712::aid-cncr2820471442>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Gall F. P., Mühe E., Gebhardt C. Results of partial and total pancreaticoduodenectomy in 117 patients with chronic pancreatitis. World J Surg. 1981 Mar;5(2):269–275. doi: 10.1007/BF01658311. [DOI] [PubMed] [Google Scholar]
- Gudjonsson B., Livstone E. M., Spiro H. M. Cancer of the pancreas: diagnostic accuracy and survival statistics. Cancer. 1978 Nov;42(5):2494–2506. doi: 10.1002/1097-0142(197811)42:5<2494::aid-cncr2820420554>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Holyoke E. D. New surgical approaches to pancreatic cancer. Cancer. 1981 Mar 15;47(6 Suppl):1719–1723. doi: 10.1002/1097-0142(19810315)47:6+<1719::aid-cncr2820471443>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Ihse I., Toregard B. M., Akerman M. Intraoperative fine needle aspiration cytology in pancreatic lesions. Ann Surg. 1979 Dec;190(6):732–734. doi: 10.1097/00000658-197912000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin B., ReMine W. H., Hermann R. E., Schein P. S., Cohn I., Jr Panel: cancer of the pancreas. Am J Surg. 1978 Feb;135(2):185–191. doi: 10.1016/0002-9610(78)90094-6. [DOI] [PubMed] [Google Scholar]
- Shapiro T. M. Adenocarcinoma of the pancreas: a statistical analysis of biliary bypass vs Whipple resection in good risk patients. Ann Surg. 1975 Dec;182(6):715–721. doi: 10.1097/00000658-197512000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]


