Abstract
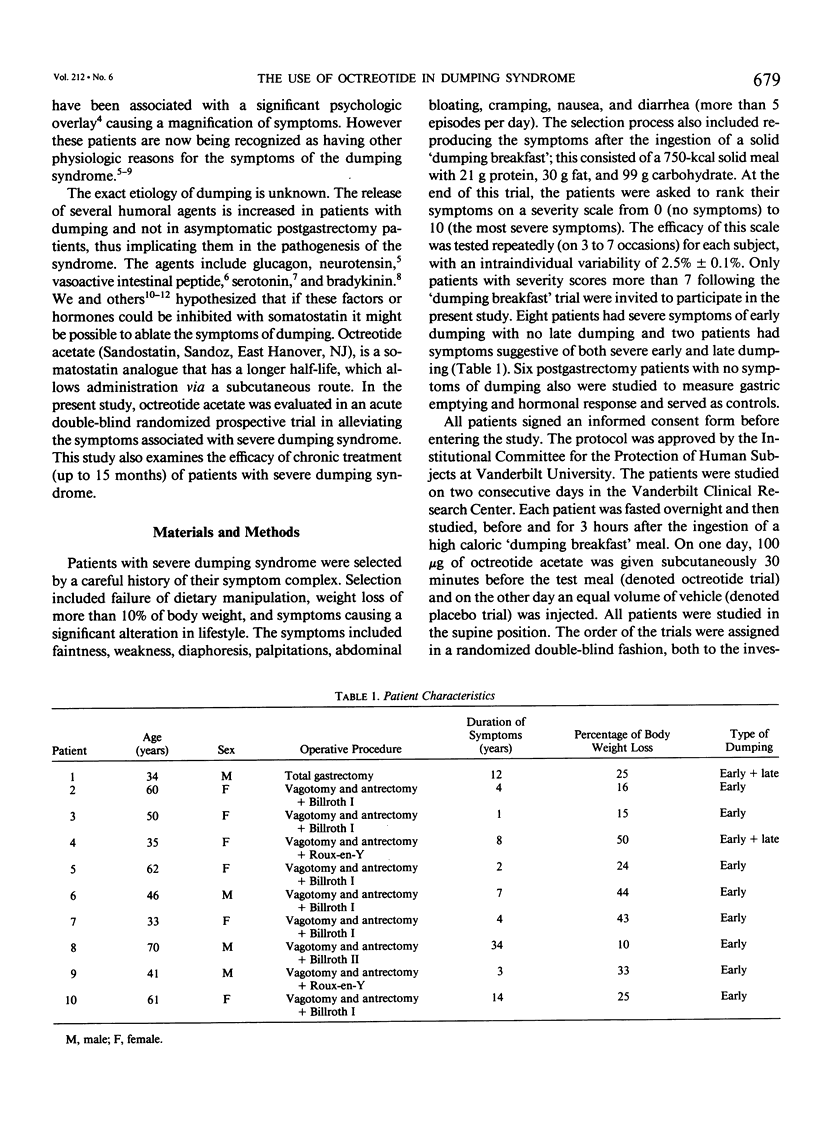
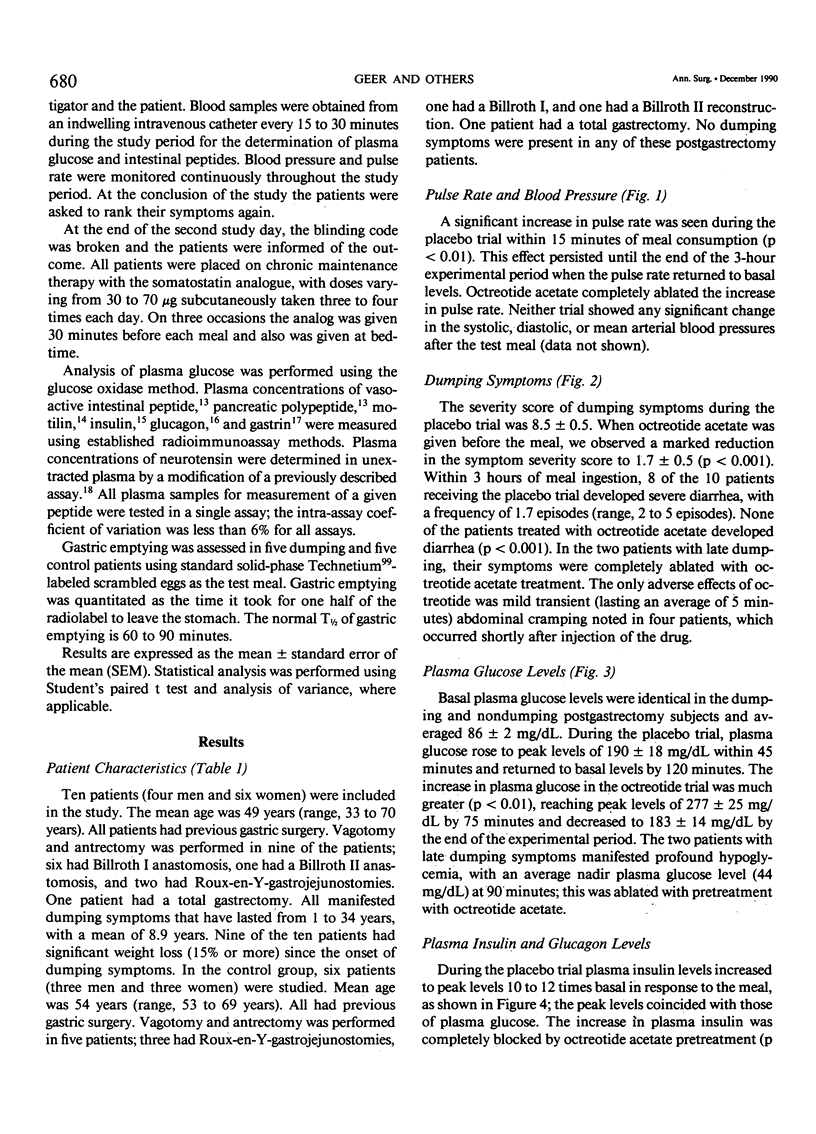
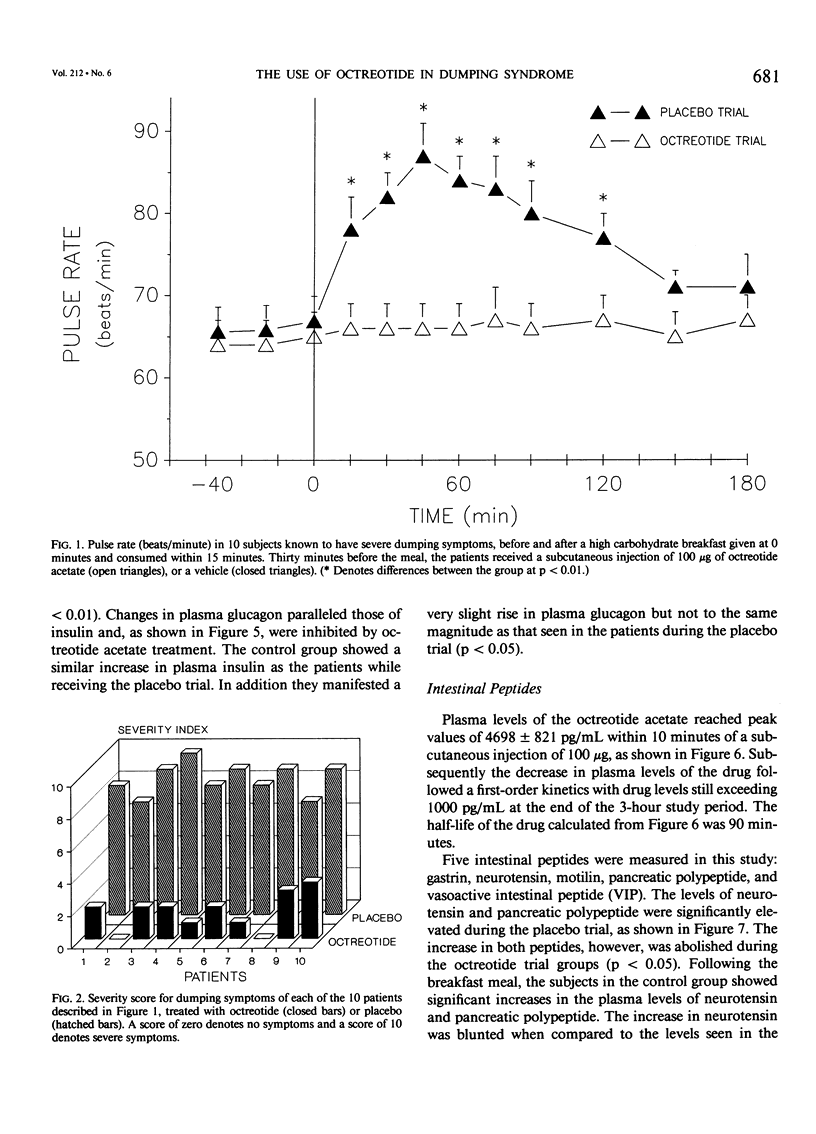
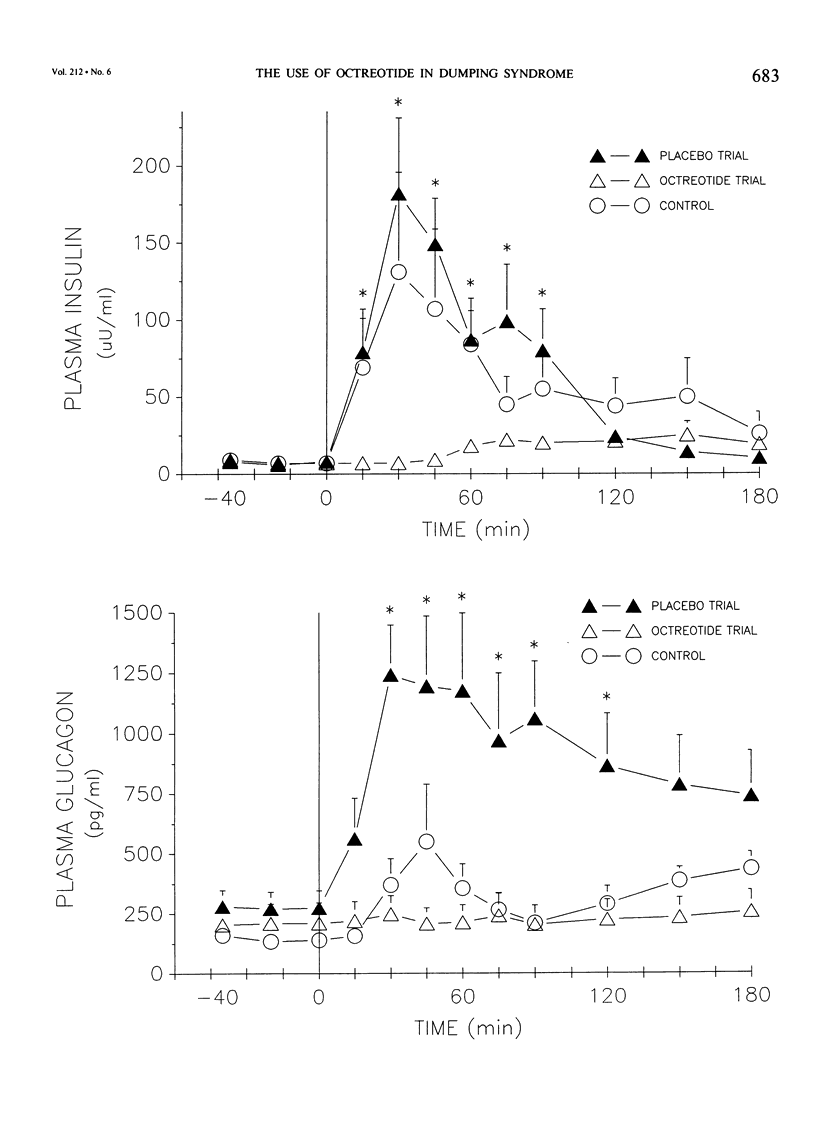
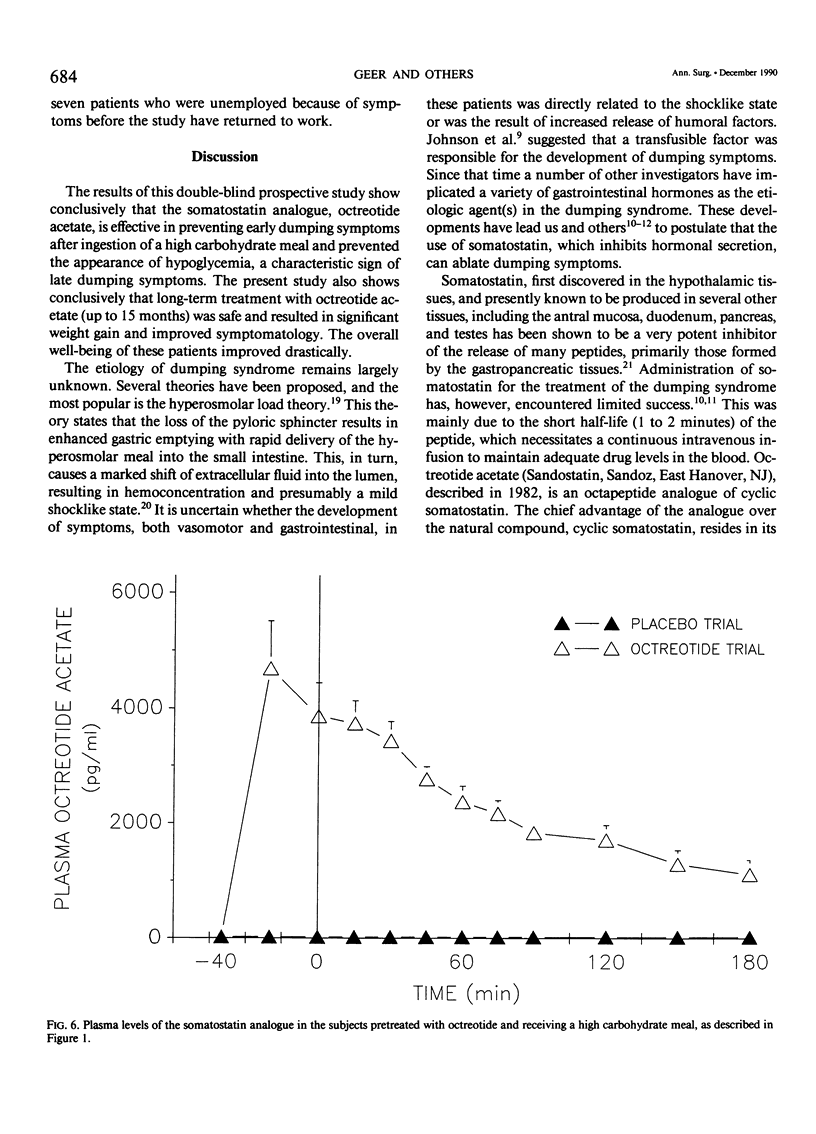
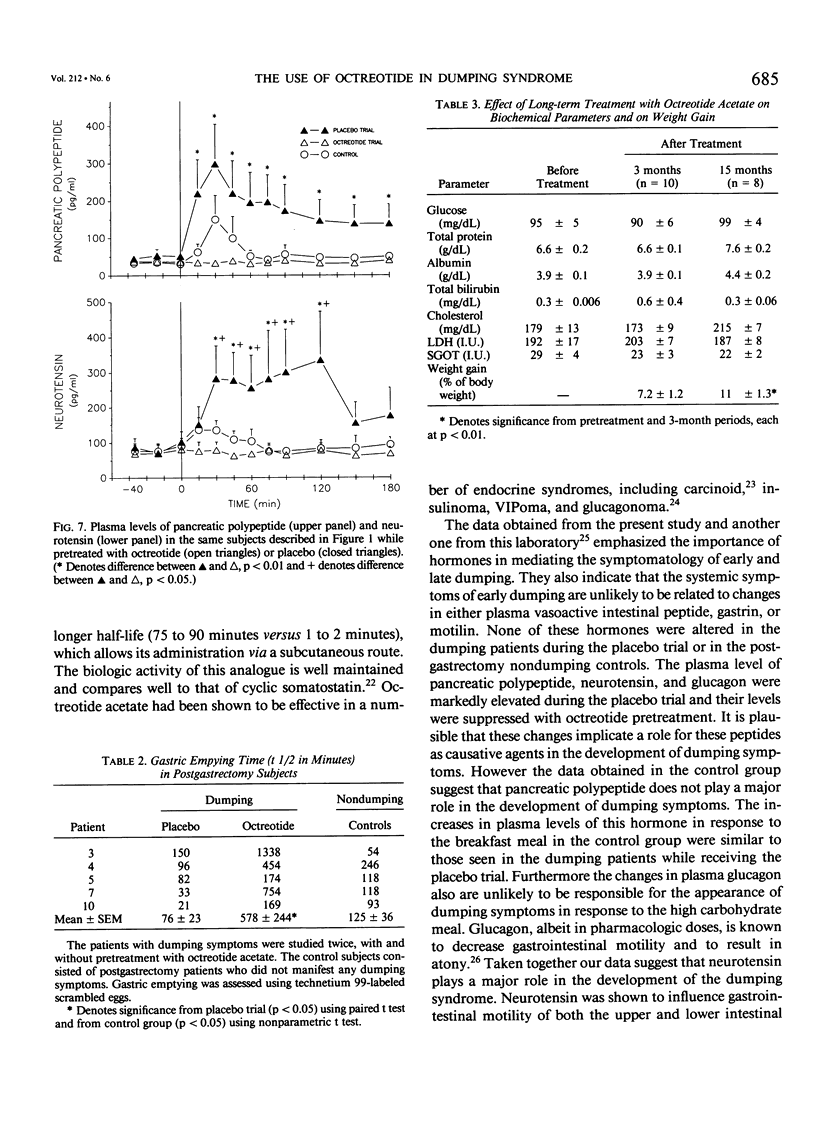
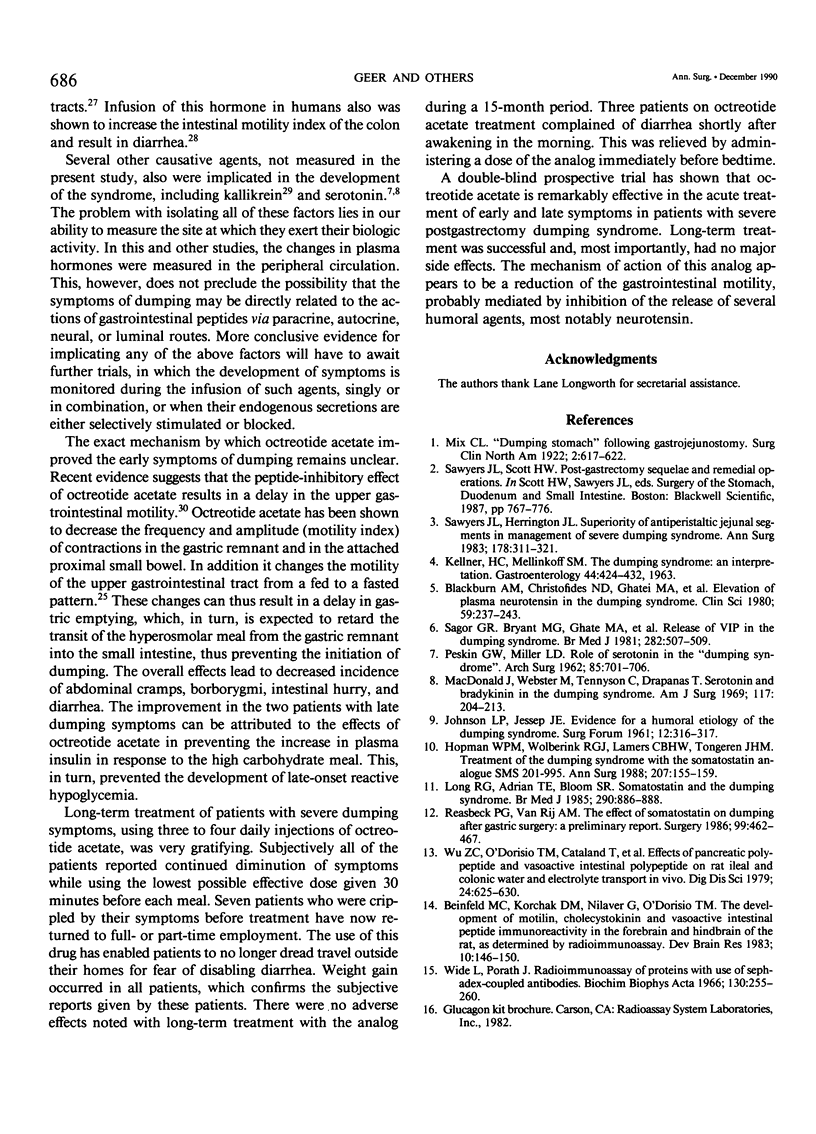
The present study evaluates the acute and chronic use of a long-acting somatostatin analog, octreotide acetate, in the treatment of patients with severe postgastrectomy dumping syndrome. In the acute phase, 10 patients with severe dumping were studied over 2 consecutive days before and for 3 hours after the ingestion of a 'dumping breakfast' in a randomized double-blind fashion. On one day octreotide (100 micrograms) was given subcutaneously 30 minutes before the test meal and on the other day an equal volume of vehicle was injected. An additional group of six postgastrectomy patients without dumping were studied in a similar fashion and these acted as controls. During placebo treatment the test meal resulted in an immediate increase (p less than 0.01) in the pulse rate and in plasma levels of glucose, glucagon, pancreatic polypeptide, neurotensin, and insulin. Similar changes were seen in the control group with respect to placebo; however glucagon and neurotensin (p less than 0.05) did not show the same magnitude of increase as seen with placebo. Treatment with octreotide acetate prevented the development of both vasomotor and gastrointestinal symptoms and completely ablated all of the above responses in plasma peptides. These changes were associated with complete ablation of diarrhea (p less than 0.001). Pretreatment with octreotide acetate completely suppressed the rise in plasma insulin response to the meal and this ablated the late hypoglycemia of dumping. Treatment with octreotide acetate resulted in delayed gastric emptying and transit time (578 +/- 244 minutes) versus 76 +/- 23 minutes with placebo and 125 +/- 36 minutes in controls (p less than 0.05). Chronic daily treatment with octreotide acetate resulted in minimal side effects. These patients demonstrated a stable fasting plasma glucose, normal liver function tests, and an average weight gain of 11% during a 12-month period. In addition most patients were able to resume employment. The long-acting somatostatin analog, octreotide acetate, is highly effective in preventing the development of symptoms of severe dumping syndrome, both vasomotor and gastrointestinal.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson J. V., Bloom S. R. Neuroendocrine tumours of the gut: long-term therapy with the somatostatin analogue SMS 201-995. Scand J Gastroenterol Suppl. 1986;119:115–128. doi: 10.3109/00365528609087439. [DOI] [PubMed] [Google Scholar]
- Bauer W., Briner U., Doepfner W., Haller R., Huguenin R., Marbach P., Petcher T. J., Pless SMS 201-995: a very potent and selective octapeptide analogue of somatostatin with prolonged action. Life Sci. 1982 Sep 13;31(11):1133–1140. doi: 10.1016/0024-3205(82)90087-x. [DOI] [PubMed] [Google Scholar]
- Beinfeld M. C., Korchak D. M., Nilaver G., O'Dorisio T. M. The development of motilin, cholecystokinin and vasoactive intestinal peptide immunoreactivity in the forebrain and hindbrain of the rat, as determined by radioimmunoassay. Brain Res. 1983 Oct;312(1):146–150. doi: 10.1016/0165-3806(83)90130-x. [DOI] [PubMed] [Google Scholar]
- Blackburn A. M., Christofides N. D., Ghatei M. A., Sarson D. L., Ebeid F. H., Ralphs D. N., Bloom S. R. Elevation of plasma neurotensin in the dumping syndrome. Clin Sci (Lond) 1980 Oct;59(4):237–243. doi: 10.1042/cs0590237. [DOI] [PubMed] [Google Scholar]
- Fuessl H. S., Carolan G., Williams G., Bloom S. R. Effect of a long-acting somatostatin analogue (SMS 201-995) on postprandial gastric emptying of 99mTc-tin colloid and mouth-to-caecum transit time in man. Digestion. 1987;36(2):101–107. doi: 10.1159/000199407. [DOI] [PubMed] [Google Scholar]
- Hopman W. P., Wolberink R. G., Lamers C. B., Van Tongeren J. H. Treatment of the dumping syndrome with the somatostatin analogue SMS 201-995. Ann Surg. 1988 Feb;207(2):155–159. doi: 10.1097/00000658-198802000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JOHNSON L. P., JESSEPH J. E. Evidence for a humoral etiology of the dumping syndrome. Surg Forum. 1961;12:316–317. [PubMed] [Google Scholar]
- Jackson B. M., Reeder D. D., Thompson J. C. Dynamic characteristics of gastrin release. Am J Surg. 1972 Feb;123(2):137–142. doi: 10.1016/0002-9610(72)90323-6. [DOI] [PubMed] [Google Scholar]
- Long R. G., Adrian T. E., Bloom S. R. Somatostatin and the dumping syndrome. Br Med J (Clin Res Ed) 1985 Mar 23;290(6472):886–888. doi: 10.1136/bmj.290.6472.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald J. M., Webster M. M., Jr, Tennyson C. H., Drapanas T. Serotonin and bradykinin in the dumping syndrome. Am J Surg. 1969 Feb;117(2):204–213. doi: 10.1016/0002-9610(69)90305-5. [DOI] [PubMed] [Google Scholar]
- Machella T. E. The Mechanism of the Post-gastrectomy "Dumping" Syndrome. Ann Surg. 1949 Aug;130(2):145–159. [PMC free article] [PubMed] [Google Scholar]
- Ouyang A., Cohen S. Effects of hormones on gastrointestinal motility. Med Clin North Am. 1981 Nov;65(6):1111–1127. doi: 10.1016/s0025-7125(16)31465-1. [DOI] [PubMed] [Google Scholar]
- PESKIN G. W., MILLER L. D. The role of serotonin in the "dumping syndrome". Arch Surg. 1962 Nov;85:701–704. doi: 10.1001/archsurg.1962.01310050003001. [DOI] [PubMed] [Google Scholar]
- Reasbeck P. G., Van Rij A. M. The effect of somatostatin on dumping after gastric surgery: a preliminary report. Surgery. 1986 Apr;99(4):462–468. [PubMed] [Google Scholar]
- Sagor G. R., Bryant M. G., Ghatei M. A., Kirk R. M., Bloom S. R. Release of vasoactive intestinal peptide in the dumping syndrome. Br Med J (Clin Res Ed) 1981 Feb 14;282(6263):507–510. doi: 10.1136/bmj.282.6263.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyers J. L., Herrington J. L., Jr Superiority of antiperistaltic jejunal segments in management of severe dumping syndrome. Ann Surg. 1973 Sep;178(3):311–321. doi: 10.1097/00000658-197309000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thor K., Rosell S. Neurotensin increases colonic motility. Gastroenterology. 1986 Jan;90(1):27–31. doi: 10.1016/0016-5085(86)90070-3. [DOI] [PubMed] [Google Scholar]
- Thor K., Rosell S., Rökaeus A., Kager L. (Gln4)-neurotensin changes the motility pattern of the duodenum and proximal jejunum from a fasting-type to a fed-type. Gastroenterology. 1982 Sep;83(3):569–574. [PubMed] [Google Scholar]
- Wong P. Y., Talamo R. C., Babior B. M., Raymond G. G., Colman R. W. Kallikrein-kinin system in postgastrectomy dumping syndrome. Ann Intern Med. 1974 May;80(5):577–581. doi: 10.7326/0003-4819-80-5-577. [DOI] [PubMed] [Google Scholar]
- Wu Z. C., O'Dorisio T. M., Cataland S., Mekhjian H. S., Gaginella T. S. Effects of pancreatic polypeptide and vasoactive intestinal polypeptide on rat ileal and colonic water and electrolyte transport in vivo. Dig Dis Sci. 1979 Aug;24(8):625–630. doi: 10.1007/BF01333707. [DOI] [PubMed] [Google Scholar]


