Abstract
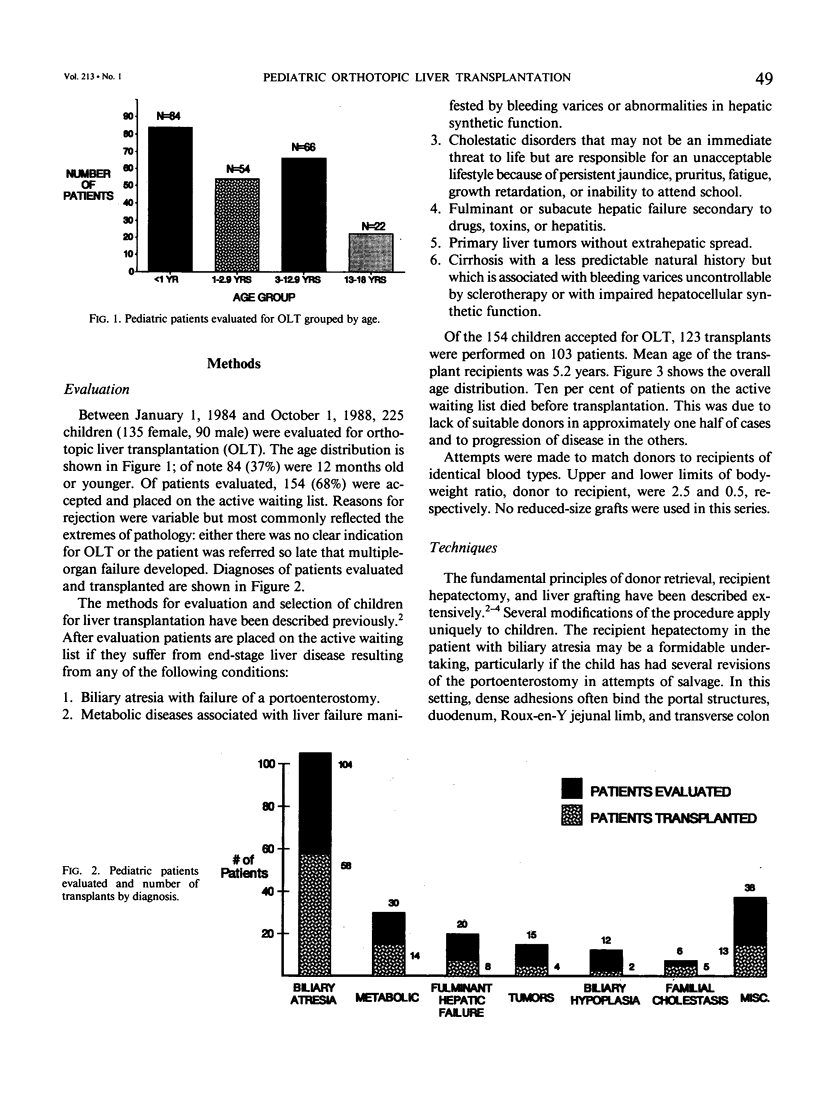
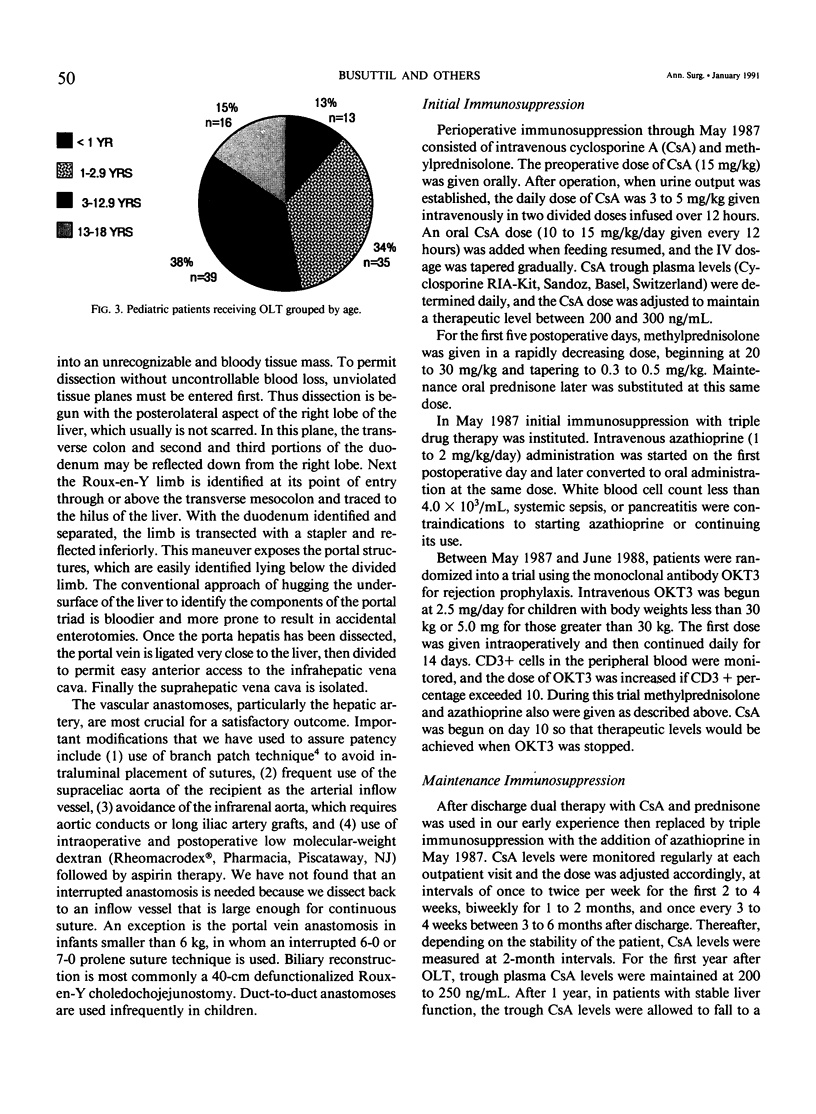
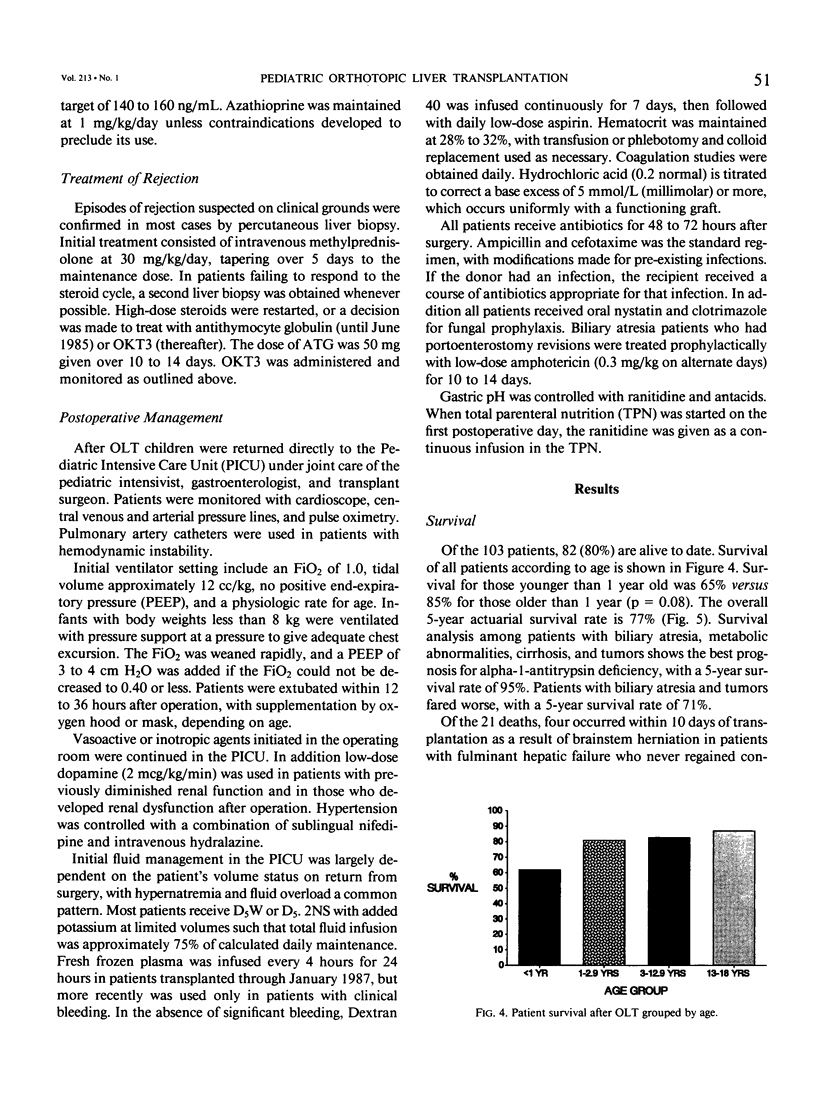
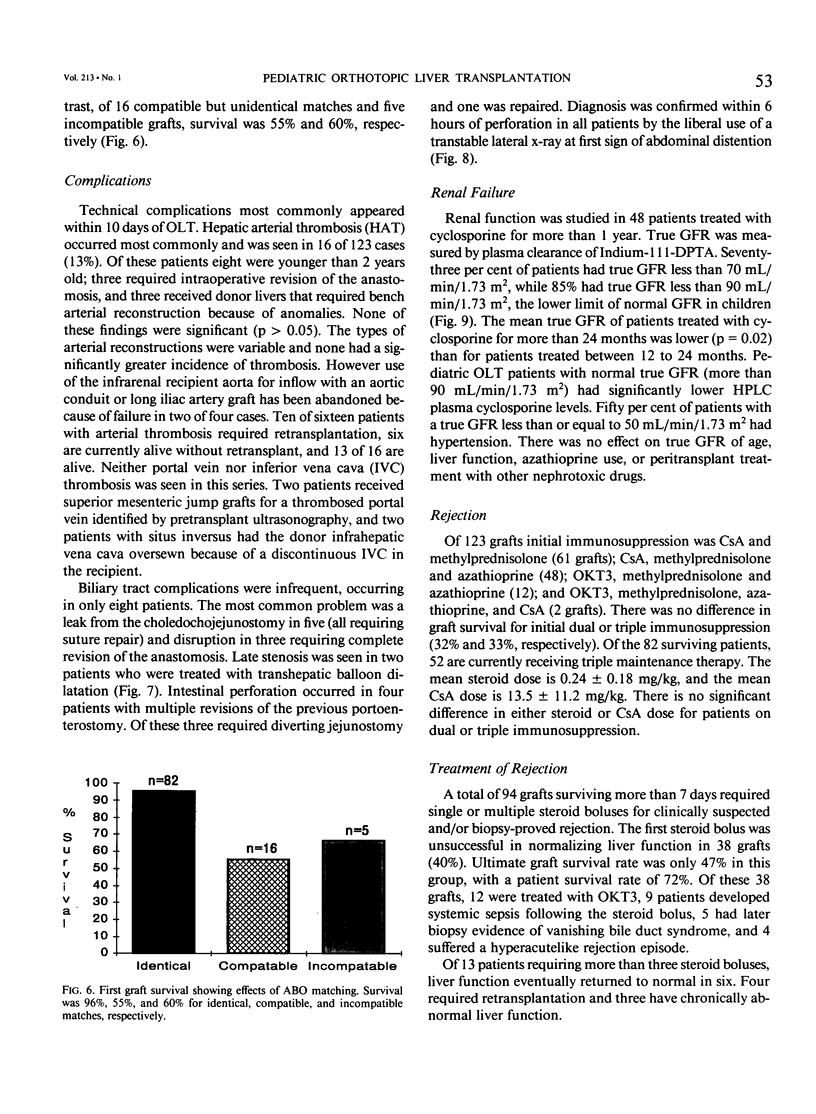
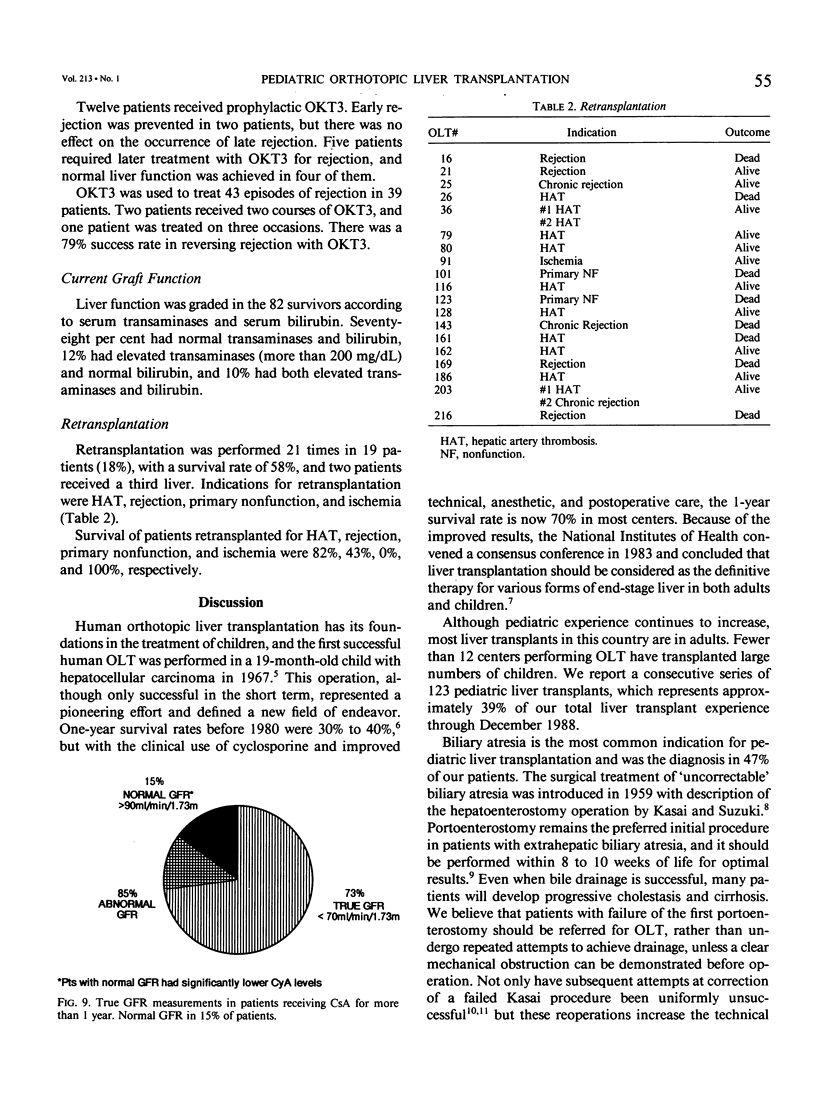
Although liver transplantation is now accepted as the ideal therapy for end-stage liver disease, relatively few centers have gained a large experience in children, and good results have been elusive. Technical difficulty and a high incidence of graft failure are among the obstacles to success. At the University of California at Los Angeles, 39% of our liver transplants are in the patients who are younger than 18 years. We have analyzed our experience with 103 patients to emphasize factors important to a favorable outcome with the procedure. One hundred twenty-three transplants were performed in 103 children (mean age, 5.2 years; 48% younger than 3 years). No reduced-size grafts were used. Scrupulous attention to technical details of the vascular reconstruction, including frequent use of the supraceliac aorta of the recipient and interrupted suture techniques, ensured construction of sound hepatic artery and portal vein anastomoses at the first operation. Preoperative exchange transfusions were used if the prothrombin time was prolonged beyond 7 seconds, resulting in an average blood loss of only 3.3 volumes. Cyclosporine dosage was maintained in the high therapeutic range for the first 4 weeks, and anti-T-cell antibody (OKT3) was used for rejection (38%). Amphotericin prophylaxis was used for biliary atresia patients with multiple previous operations. Eighty-two of one hundred three patients (80%) are alive. There were no intraoperative deaths. Actuarial survival rates at 6 months, 1 year, and 5 years are 80%, 79%, and 77%, respectively. Survival of patients who underwent transplantation at age less than 1 year is 65% versus 85% at age more than 1 year (p = 0.08). Retransplantation was performed in 19 patients (18%), with a survival rate of 58%. Hepatic artery thrombosis, the most frequent technical complication, occurred in only 16 patients (13%). Survival rates of ABO identical-match versus nonidentical-match grafts were 96% and 60%, respectively (p = 0.02). Graft survival was only 47% if more than one steroid cycle was needed, compared to 75% survival with OKT3 treatment. Despite impairment of renal function (glomerular filtration rate [GFR] less than 80 cc/kg/min) in 54% of patients and hypertension requiring therapy in 27%, 90% of the children demonstrated enhancement of growth, development, and functional status. The following conclusions were made. (1) Pediatric liver transplantation is the treatment of choice for all types of end-stage liver disease and should be considered early. (2) Factors that enhance survival include technical precision, aggressive retransplantation, antifungal chemoprophylaxis and therapy, and judicious immunosuppression with use of OKT3 for rejection.(ABSTRACT TRUNCATED AT 400 WORDS)
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Altman R. P. Results of re-operations for correction of extrahepatic biliary atresia. J Pediatr Surg. 1979 Jun;14(3):305–309. doi: 10.1016/s0022-3468(79)80488-1. [DOI] [PubMed] [Google Scholar]
- Andrews W. S., Wanek E., Fyock B., Gray S., Benser M. Pediatric liver transplantation: a 3-year experience. J Pediatr Surg. 1989 Jan;24(1):77–82. doi: 10.1016/s0022-3468(89)80306-9. [DOI] [PubMed] [Google Scholar]
- Broelsch C. E., Emond J. C., Thistlethwaite J. R., Whitington P. F., Zucker A. R., Baker A. L., Aran P. F., Rouch D. A., Lichtor J. L. Liver transplantation, including the concept of reduced-size liver transplants in children. Ann Surg. 1988 Oct;208(4):410–420. doi: 10.1097/00000658-198810000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busuttil R. W., Colonna J. O., 2nd, Hiatt J. R., Brems J. J., el Khoury G., Goldstein L. I., Quinones-Baldrich W. J., Abdul-Rasool I. H., Ramming K. P. The first 100 liver transplants at UCLA. Ann Surg. 1987 Oct;206(4):387–402. doi: 10.1097/00000658-198710000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colonna J. O., 2nd, Goldstein L. I., Brems J. J., Vargas J. H., Brill J. E., Berquist W. J., Hiatt J. R., Busuttil R. W. A prospective study on the use of monoclonal anti-T3-cell antibody (OKT3) to treat steroid-resistant liver transplant rejection. Arch Surg. 1987 Oct;122(10):1120–1123. doi: 10.1001/archsurg.1987.01400220030004. [DOI] [PubMed] [Google Scholar]
- Cosimi A. B., Cho S. I., Delmonico F. L., Kaplan M. M., Rohrer R. J., Jenkins R. L. A randomized clinical trial comparing OKT3 and steroids for treatment of hepatic allograft rejection. Transplantation. 1987 Jan;43(1):91–95. doi: 10.1097/00007890-198701000-00020. [DOI] [PubMed] [Google Scholar]
- Esquivel C. O., Fung J. J., Markus B., Iwatsuki S., Gordon R. D., Makowka L., Marsh J. W., Jr, Tzakis A. G., Todo S., Starzl T. E. OKT3 in the reversal of acute hepatic allograft rejection. Transplant Proc. 1987 Feb;19(1 Pt 3):2443–2446. [PMC free article] [PubMed] [Google Scholar]
- Goldstein G., Kremer A. B., Barnes L., Hirsch R. L. OKT3 monoclonal antibody reversal of renal and hepatic rejection in pediatric patients. J Pediatr. 1987 Dec;111(6 Pt 2):1046–1050. doi: 10.1016/s0022-3476(87)80054-9. [DOI] [PubMed] [Google Scholar]
- Gordon R. D., Tzakis A. G., Iwatsuki S., Todo S., Esquivel C. O., Marsh J. W., Stieber A., Makowka L., Starzl T. E. Experience with Orthoclone OKT3 monoclonal antibody in liver transplantation. Am J Kidney Dis. 1988 Feb;11(2):141–144. doi: 10.1016/s0272-6386(88)80199-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiatt J. R., Ament M. E., Berquist W. J., Brems J. F., Brill J. E., Colonna J. O., 2nd, el Khoury G., Quinones W. J., Ramming K. P., Vargas J. H. Pediatric liver transplantation at UCLA. Transplant Proc. 1987 Aug;19(4):3282–3288. [PubMed] [Google Scholar]
- Hoffer F. A., Teele R. L., Lillehei C. W., Vacanti J. P. Infected bilomas and hepatic artery thrombosis in infant recipients of liver transplants. Interventional radiology and medical therapy as an alternative to retransplantation. Radiology. 1988 Nov;169(2):435–438. doi: 10.1148/radiology.169.2.3051118. [DOI] [PubMed] [Google Scholar]
- Kalayoglu M., Stratta R. J., Sollinger H. W., Hoffmann R. M., D'Alessandro A. M., Pirsch J. D., Belzer F. O. Liver transplantation in infants and children. J Pediatr Surg. 1989 Jan;24(1):70–76. doi: 10.1016/s0022-3468(89)80305-7. [DOI] [PubMed] [Google Scholar]
- Mazzaferro V., Esquivel C. O., Makowka L., Belle S., Kahn D., Koneru B., Scantlebury V. P., Stieber A. C., Todo S., Tzakis A. G. Hepatic artery thrombosis after pediatric liver transplantation--a medical or surgical event? Transplantation. 1989 Jun;47(6):971–977. doi: 10.1097/00007890-198906000-00011. [DOI] [PubMed] [Google Scholar]
- Millis J. M., Brems J. J., Hiatt J. R., Klein A. S., Ashizawa T., Ramming K. P., Quinones-Baldrich W. J., Busuttil R. W. Orthotopic liver transplantation for biliary atresia. Evolution of management. Arch Surg. 1988 Oct;123(10):1237–1239. doi: 10.1001/archsurg.1988.01400340063011. [DOI] [PubMed] [Google Scholar]
- Ohi R., Hanamatsu M., Mochizuki I., Chiba T., Kasai M. Progress in the treatment of biliary atresia. World J Surg. 1985 Apr;9(2):285–293. doi: 10.1007/BF01656322. [DOI] [PubMed] [Google Scholar]
- Otte J. B., Yandza T., de Ville de Goyet J., Tan K. C., Salizzoni M., de Hemptinne B. Pediatric liver transplantation: report on 52 patients with a 2-year survival of 86%. J Pediatr Surg. 1988 Mar;23(3):250–253. doi: 10.1016/s0022-3468(88)80733-4. [DOI] [PubMed] [Google Scholar]
- Otte J. B., de Ville de Goyet J., Sokal E., Alberti D., Moulin D., de Hemptinne B., Veyckemans F., van Obbergh L., Carlier M., Clapuyt P. Size reduction of the donor liver is a safe way to alleviate the shortage of size-matched organs in pediatric liver transplantation. Ann Surg. 1990 Feb;211(2):146–157. doi: 10.1097/00000658-199002000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettitt B. J., Zitelli B. J., Rowe M. I. Analysis of patients with biliary atresia coming to liver transplantation. J Pediatr Surg. 1984 Dec;19(6):779–785. doi: 10.1016/s0022-3468(84)80368-1. [DOI] [PubMed] [Google Scholar]
- Quinones-Baldrich W. J., Memsic L., Ramming K., Hiatt J., Busuttil R. W. Branch patch for arterialization of hepatic grafts. Surg Gynecol Obstet. 1986 May;162(5):488–490. [PubMed] [Google Scholar]
- STARZL T. E., MARCHIORO T. L., VONKAULLA K. N., HERMANN G., BRITTAIN R. S., WADDELL W. R. HOMOTRANSPLANTATION OF THE LIVER IN HUMANS. Surg Gynecol Obstet. 1963 Dec;117:659–676. [PMC free article] [PubMed] [Google Scholar]
- Starzl T. E., Esquivel C., Gordon R., Todo S. Pediatric liver transplantation. Transplant Proc. 1987 Aug;19(4):3230–3235. [PMC free article] [PubMed] [Google Scholar]
- Starzl T. E., Groth C. G., Brettschneider L., Penn I., Fulginiti V. A., Moon J. B., Blanchard H., Martin A. J., Jr, Porter K. A. Orthotopic homotransplantation of the human liver. Ann Surg. 1968 Sep;168(3):392–415. doi: 10.1097/00000658-196809000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starzl T. E., Iwatsuki S., Van Thiel D. H., Gartner J. C., Zitelli B. J., Malatack J. J., Schade R. R., Shaw B. W., Jr, Hakala T. R., Rosenthal J. T. Evolution of liver transplantation. Hepatology. 1982 Sep-Oct;2(5):614–636. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratta R. J., Wood R. P., Langnas A. N., Hollins R. R., Bruder K. J., Donovan J. P., Burnett D. A., Lieberman R. P., Lund G. B., Pillen T. J. Diagnosis and treatment of biliary tract complications after orthotopic liver transplantation. Surgery. 1989 Oct;106(4):675–684. [PubMed] [Google Scholar]