Abstract
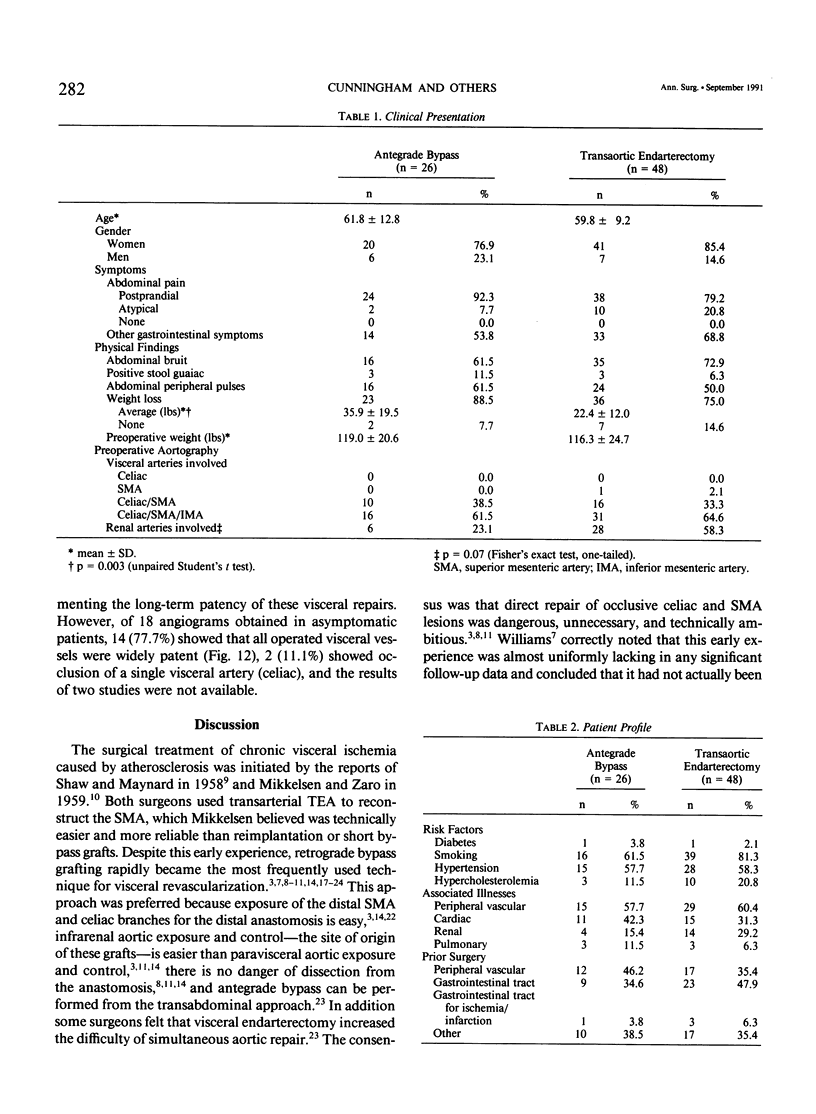
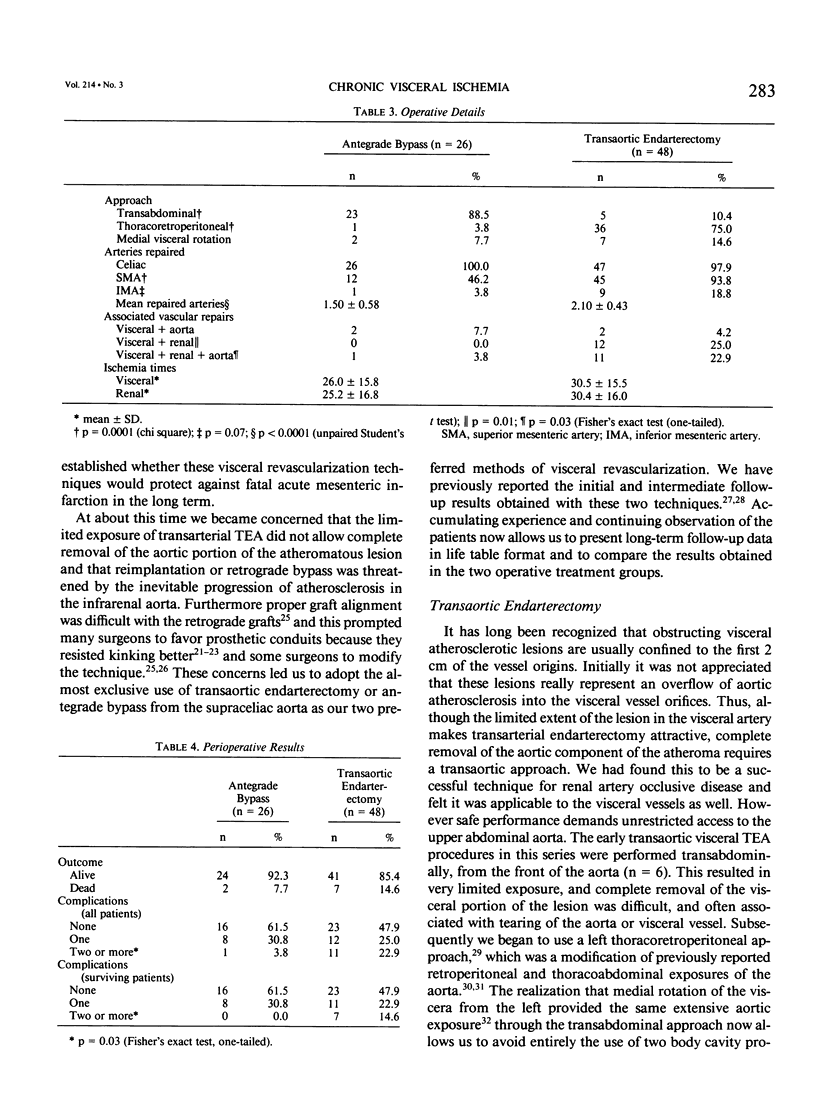
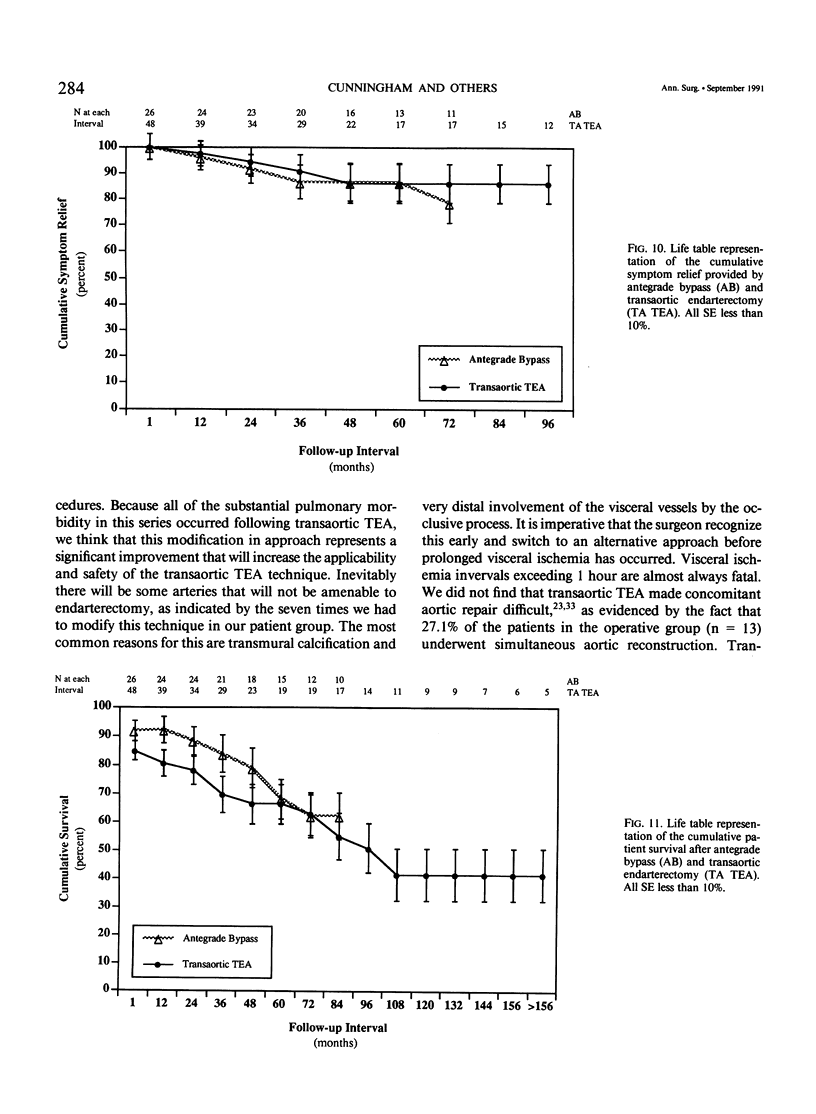
Symptomatic visceral atherosclerosis is a major surgical challenge because of its life-threatening course and the complexity of its definitive operative treatment. Evolution in the operative approach to the visceral aorta and progress in the intraoperative management of patients undergoing complex vascular reconstructions prompted a review of the authors' cumulative experience in the surgical management of chronic visceral ischemia. Among all patients undergoing visceral revascularization at the University of California, San Francisco during the past three decades, 74 patients were identified whose primary reconstruction used transaortic endarterectomy (TA TEA) (n = 48) or antegrade bypass (AB) (n = 26), the authors' preferred revascularization techniques. The two treatment groups were comparable in gender distribution, age, presenting symptoms, and physical findings, although the amount of preoperative weight loss was greater in the AB group (35.8 +/- 19.5 versus 22.4 +/- 12.0, p = 0.003). The groups were also comparable in the prevalence of atherosclerosis risk factors, symptomatic vascular disease at other sites, and previous vascular operations. However associated renal artery atherosclerosis was slightly greater in the TA TEA group (58.3% versus 23.1%, p = 0.07) when compared to the AB group. Antegrade bypass was usually performed transabdominally (88.5%), while TA TEA was approached thoracoretroperitoneally (75.0%). Celiac revascularization was almost universal in both treatment groups, but the TA TEA group underwent significantly more frequent superior mesenteric artery (SMA) revascularization (93.8% versus 46.2%, p = 0.0001) and slightly more frequent inferior mesenteric repair (18.8% versus 3.8%, p = 0.07) than the AB group. In addition the frequency of combined renal and visceral repair (25.0% versus 0.0%, p = 0.01) as well as combined aortic, renal, and visceral repair (22.9% versus 3.8%, p = 0.03) was significantly greater in the TA TEA group. The obligatory interval of renal and visceral ischemia did not differ between the two approaches. The perioperative mortality rate was 12.2% and was the same for TA TEA (14.6%) and AB (7.7%). Overall the incidence of complications was the same with either operative approach, although patients in the TA TEA group tended to have multiple complications (17.1% versus 0.0, p = 0.03) and all significant pulmonary complications occurred in this group. Two patients were lost to follow-up. The cumulative percentage of patients who remained asymptomatic following AB or TA TEA was (respectively) 95.8% and 97.3% at 1 year and 86.5% and 86.1% at 5 years. Both of these operative approaches provide durable symptom relief with acceptable operative morbidity and mortality rates.(ABSTRACT TRUNCATED AT 400 WORDS)
Full text
PDF
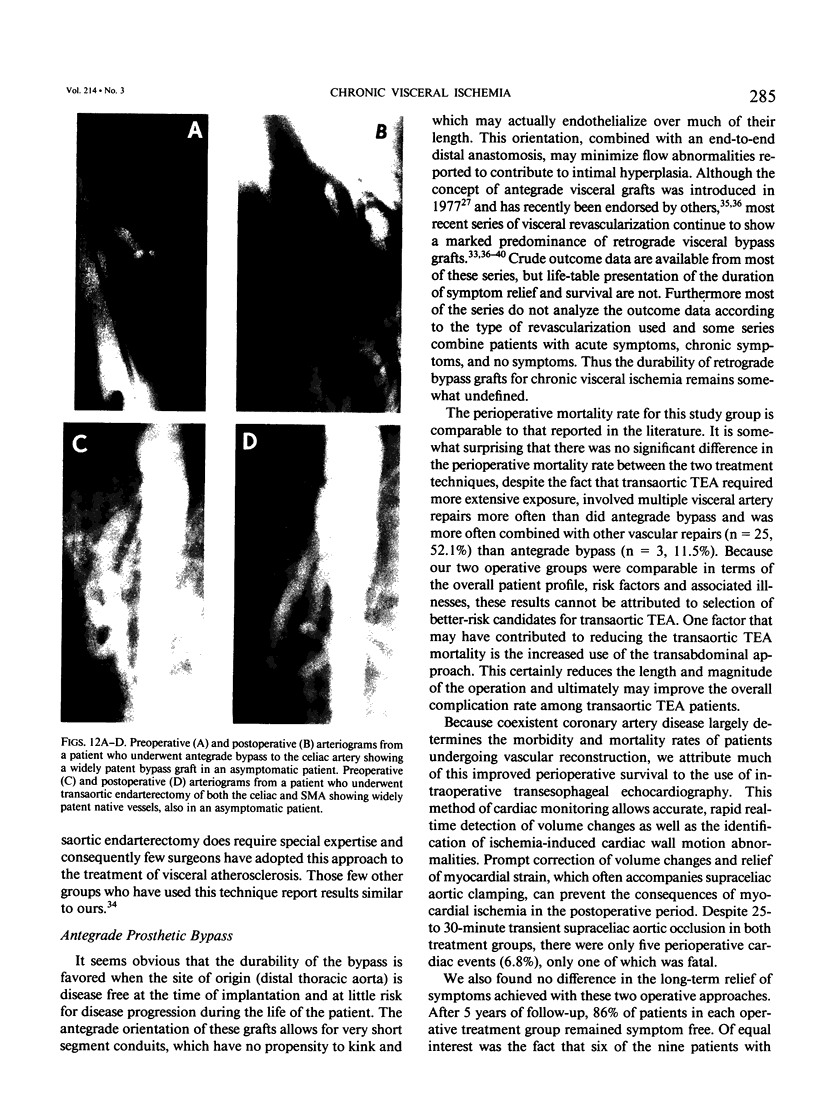
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adashek K., Wittenstein G. Mesenteric revascularization: an operative approach. Am J Surg. 1979 Jun;137(6):821–823. doi: 10.1016/0002-9610(79)90104-1. [DOI] [PubMed] [Google Scholar]
- Baur G. M., Millay D. J., Taylor L. M., Jr, Porter J. M. Treatment of chronic visceral ischemia. Am J Surg. 1984 Jul;148(1):138–144. doi: 10.1016/0002-9610(84)90301-5. [DOI] [PubMed] [Google Scholar]
- Beebe H. G., MacFarlane S., Raker E. J. Supraceliac aortomesenteric bypass for intestinal ischemia. J Vasc Surg. 1987 May;5(5):749–754. doi: 10.1067/mva.1987.avs0050749. [DOI] [PubMed] [Google Scholar]
- Bergan J. J., Dry L., Conn J., Jr, Trippel O. H. Intestinal ischemic syndromes. Ann Surg. 1969 Jan;169(1):120–126. doi: 10.1097/00000658-196901000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CONNOLLY J. E., ABRAMS H. L., KIERALDO J. H. OBSERVATIONS ON THE DIAGNOSIS AND TREATMENT OF OBLITERATIVE DISEASE OF THE VISCERAL BRANCHES OF THE ABDOMINAL AORTA. Arch Surg. 1965 Apr;90:596–606. doi: 10.1001/archsurg.1965.01320100140021. [DOI] [PubMed] [Google Scholar]
- Crawford E. S., Morris G. C., Jr, Myhre H. O., Roehm J. O., Jr Celiac axis, superior mesenteric artery, and inferior mesenteric artery occlusion: surgical considerations. Surgery. 1977 Dec;82(6):856–866. [PubMed] [Google Scholar]
- Crawford E. S., Morris G. C., Jr, Myhre H. O., Roehm J. O., Jr Celiac axis, superior mesenteric artery, and inferior mesenteric artery occlusion: surgical considerations. Surgery. 1977 Dec;82(6):856–866. [PubMed] [Google Scholar]
- DEBAKEY M. E., CREECH O., Jr, MORRIS G. C., Jr Aneurysm of thoracoabdominal aorta involving the celiac, superior mesenteric, and renal arteries; report of four cases treated by resection and homograft replacement. Ann Surg. 1956 Oct;144(4):549–573. doi: 10.1097/00000658-195610000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DERRICK J. R., POLLARD H. S., MOORE R. M. The pattern of arteriosclerotic narrowing of the celiac and superior mesenteric arteries. Ann Surg. 1959 May;149(5):684–689. doi: 10.1097/00000658-195905000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUBOST C., ALLARY M., OECONOMOS N. Resection of an aneurysm of the abdominal aorta: reestablishment of the continuity by a preserved human arterial graft, with result after five months. AMA Arch Surg. 1952 Mar;64(3):405–408. [PubMed] [Google Scholar]
- Daily P. O., Fogarty T. J. Simplified revascularization of the celiac and superior mesenteric arteries. Am J Surg. 1976 Jun;131(6):762–765. doi: 10.1016/0002-9610(76)90197-5. [DOI] [PubMed] [Google Scholar]
- Elkins R., DeMeester T. R., Brawley R. K. Surgical exposure of the upper abdominal aorta and its branches. Surgery. 1971 Oct;70(4):622–627. [PubMed] [Google Scholar]
- FRY W. J., KRAFT R. O. VISCERAL ANGINA. Surg Gynecol Obstet. 1963 Oct;117:417–424. [PubMed] [Google Scholar]
- Hertzer N. R., Beven E. G., Humphries A. W. Chronic intestinal ischemia. Surg Gynecol Obstet. 1977 Sep;145(3):321–328. [PubMed] [Google Scholar]
- Hollier L. H., Bernatz P. E., Pairolero P. C., Payne W. S., Osmundson P. J. Surgical management of chronic intestinal ischemia: a reappraisal. Surgery. 1981 Dec;90(6):940–946. [PubMed] [Google Scholar]
- Jaffe M. S. Status of abdominal visceral circulation via superior mesenteric prosthesis. Am J Surg. 1971 Jun;121(6):736–738. doi: 10.1016/0002-9610(71)90059-6. [DOI] [PubMed] [Google Scholar]
- MIKKELSEN W. P. Intestinal angina: its surgical significance. Am J Surg. 1957 Aug;94(2):262-7; discussion, 267-9. doi: 10.1016/0002-9610(57)90654-2. [DOI] [PubMed] [Google Scholar]
- MIKKELSEN W. P., ZARO J. A., Jr Intestinal angina; report of a case with preoperative diagnosis and surgical relief. N Engl J Med. 1959 Apr 30;260(18):912–914. doi: 10.1056/NEJM195904302601804. [DOI] [PubMed] [Google Scholar]
- Marston A. Patterns of Intestinal Ischaemia: Arris and Gale Lecture delivered at the Royal College of Surgeons of England on 6th February 1964. Ann R Coll Surg Engl. 1964 Sep;35(3):151–181. [PMC free article] [PubMed] [Google Scholar]
- McCollum C. H., Graham J. M., DeBakey M. E. Chronic mesenteric arterial insufficiency: results of revascularization in 33 cases. South Med J. 1976 Oct;69(10):1266–1268. doi: 10.1097/00007611-197610000-00006. [DOI] [PubMed] [Google Scholar]
- Morris G. C., Jr, De Bakey M. E., Bernhard V. Abdominal angina. Surg Clin North Am. 1966 Aug;46(4):919–930. doi: 10.1016/s0039-6109(16)37936-1. [DOI] [PubMed] [Google Scholar]
- Nunn D. B. Chronic intestinal angina: a report of two patients treated successfully by operation. Ann Surg. 1972 Apr;175(4):523–527. doi: 10.1097/00000658-197204000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuhn S. P., Reilly L. M., Bennett J. B., Hughes L., 3rd, Goldstone J., Ehrenfeld W. K., Stoney R. J. Intraoperative assessment of renal and visceral artery reconstruction: the role of duplex scanning and spectral analysis. J Vasc Surg. 1987 Jan;5(1):137–147. [PubMed] [Google Scholar]
- Pokrovsky A. V., Kasantchjan P. O. Surgical treatment of chronic occlusive disease of the enteric visceral branches of the abdominal aorta. Experience with 119 operations. Ann Surg. 1980 Jan;191(1):51–56. doi: 10.1097/00000658-198001000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- REINER L., JIMENEZ F. A., RODRIGUEZ F. L. ATHEROSCLEROSIS IN THE MESENTERIC CIRCULATION. OBSERVATIONS AND CORRELATIONS WITH AORTIC AND CORONARY ATHEROSCLEROSIS. Am Heart J. 1963 Aug;66:200–209. doi: 10.1016/0002-8703(63)90035-8. [DOI] [PubMed] [Google Scholar]
- Rapp J. H., Reilly L. M., Qvarfordt P. G., Goldstone J., Ehrenfeld W. K., Stoney R. J. Durability of endarterectomy and antegrade grafts in the treatment of chronic visceral ischemia. J Vasc Surg. 1986 May;3(5):799–806. doi: 10.1067/mva.1986.avs0030799. [DOI] [PubMed] [Google Scholar]
- Reul G. J., Jr, Wukash D. C., Sandiford F. M., Chiarillo L., Hallman G. L., Cooley D. A. Surgical treatment of abdominal angina: review of 25 patients. Surgery. 1974 May;75(5):682–689. [PubMed] [Google Scholar]
- Rheudasil J. M., Stewart M. T., Schellack J. V., Smith R. B., 3rd, Salam A. A., Perdue G. D. Surgical treatment of chronic mesenteric arterial insufficiency. J Vasc Surg. 1988 Oct;8(4):495–500. [PubMed] [Google Scholar]
- Rob C. Surgical diseases of the celiac and mesenteric arteries. Arch Surg. 1966 Jul;93(1):21–32. doi: 10.1001/archsurg.1966.01330010023004. [DOI] [PubMed] [Google Scholar]
- Rogers D. M., Thompson J. E., Garrett W. V., Talkington C. M., Patman R. D. Mesenteric vascular problems. A 26-year experience. Ann Surg. 1982 May;195(5):554–565. doi: 10.1097/00000658-198205000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers D. M., Thompson J. E., Garrett W. V., Talkington C. M., Patman R. D. Mesenteric vascular problems. A 26-year experience. Ann Surg. 1982 May;195(5):554–565. doi: 10.1097/00000658-198205000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roizen M. F., Beaupre P. N., Alpert R. A., Kremer P., Cahalan M. K., Shiller N., Sohn Y. J., Cronnelly R., Lurz F. W., Ehrenfeld W. K. Monitoring with two-dimensional transesophageal echocardiography. Comparison of myocardial function in patients undergoing supraceliac, suprarenal-infraceliac, or infrarenal aortic occlusion. J Vasc Surg. 1984 Mar;1(2):300–305. [PubMed] [Google Scholar]
- SHAW R. S., MAYNARD E. P., 3rd Acute and chronic thrombosis of the mesenteric arteries associated with malabsorption; a report of two cases successfully treated by thromboendarterectomy. N Engl J Med. 1958 May 1;258(18):874–878. doi: 10.1056/NEJM195805012581803. [DOI] [PubMed] [Google Scholar]
- Stanton P. E., Jr, Hollier P. A., Seidel T. W., Rosenthal D., Clark M., Lamis P. A. Chronic intestinal ischemia: diagnosis and therapy. J Vasc Surg. 1986 Oct;4(4):338–344. [PubMed] [Google Scholar]
- Stoney R. J., Ehrenfeld W. K., Wylie E. J. Revascularization methods in chronic visceral ischemia caused by atherosclerosis. Ann Surg. 1977 Oct;186(4):468–476. doi: 10.1097/00000658-197710000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoney R. J., Wylie E. J. Recognition and surgical management of visceral ischemic syndromes. Ann Surg. 1966 Oct;164(4):714–722. doi: 10.1097/00000658-196610000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoney R. J., Wylie E. J. Surgical management of arterial lesions of the thoracoabdominal aorta. Am J Surg. 1973 Aug;126(2):157–164. doi: 10.1016/s0002-9610(73)80147-3. [DOI] [PubMed] [Google Scholar]
- Zelenock G. B., Graham L. M., Whitehouse W. M., Jr, Erlandson E. E., Kraft R. O., Lindenauer S. M., Stanley J. C. Splanchnic arteriosclerotic disease and intestinal angina. Arch Surg. 1980 Apr;115(4):497–501. doi: 10.1001/archsurg.1980.01380040119021. [DOI] [PubMed] [Google Scholar]