Abstract
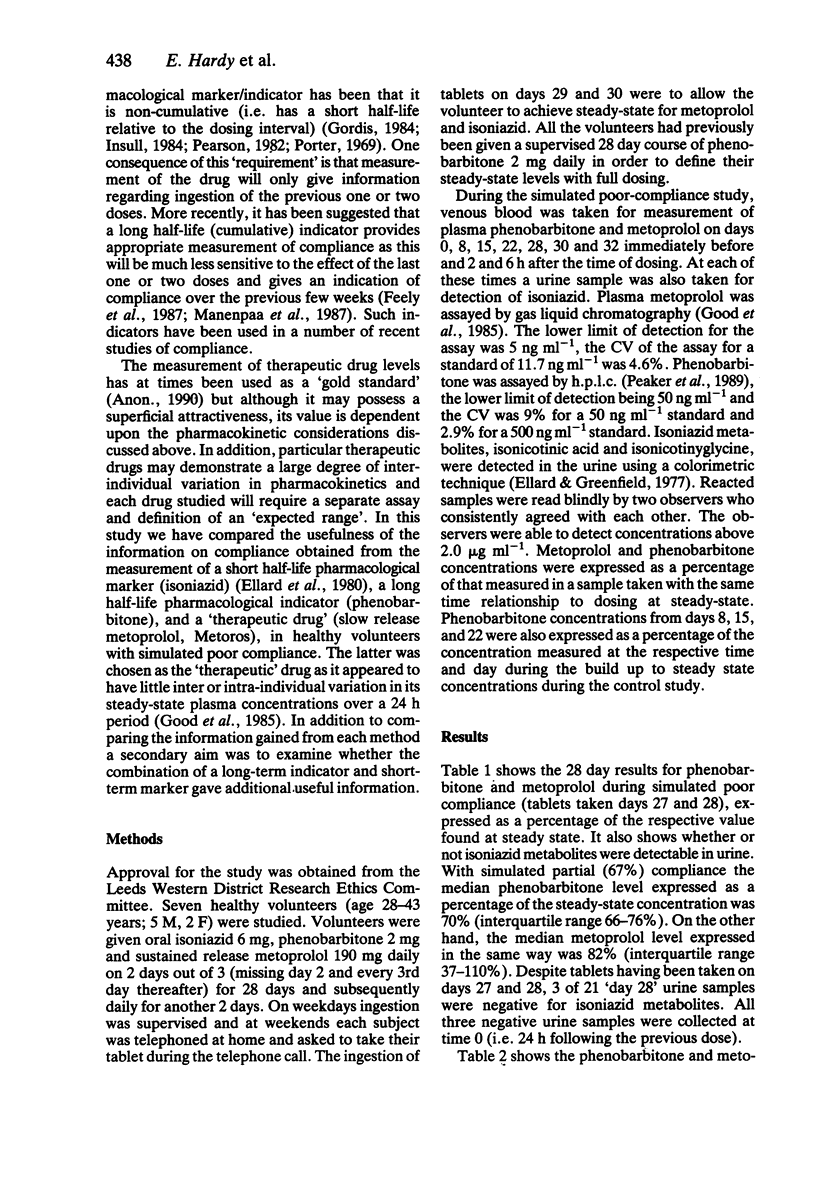
1. Although, long half-life compounds appear to be more appropriate pharmacological indicators of compliance with treatment, short half-life markers or measurements of short half-life therapeutic drugs are frequently used. 2. We have compared the usefulness of low-dose phenobarbitone (a long half-life indicator), low dose isoniazid (a short half-life marker) and controlled release metoprolol (Metros) (a controlled release formulation of a short half-life 'therapeutic' drug) in seven volunteers with simulated partial (two thirds) compliance. 3. Detection of isoniazid metabolites in urine had an 83% sensitivity and 94% specificity for detecting ingestion within the previous 24 h and 100% sensitivity and 82% specificity for detecting ingestion within the past 6 h but gave no indication of the longer term pattern of compliance. 4. At 28 days (a time when steady-state would be obtained for all three drugs) phenobarbitone plasma levels were 70% (66-76%)--median and interquartile range--of the expected steady-state level if compliance had been complete. Corresponding figures for metoprolol were 82% (37-100%). 5. Measurement of phenobarbitone was much superior to isoniazid or metoprolol measurements in reflecting partial compliance over the previous 1 to 4 weeks.
Full text
PDF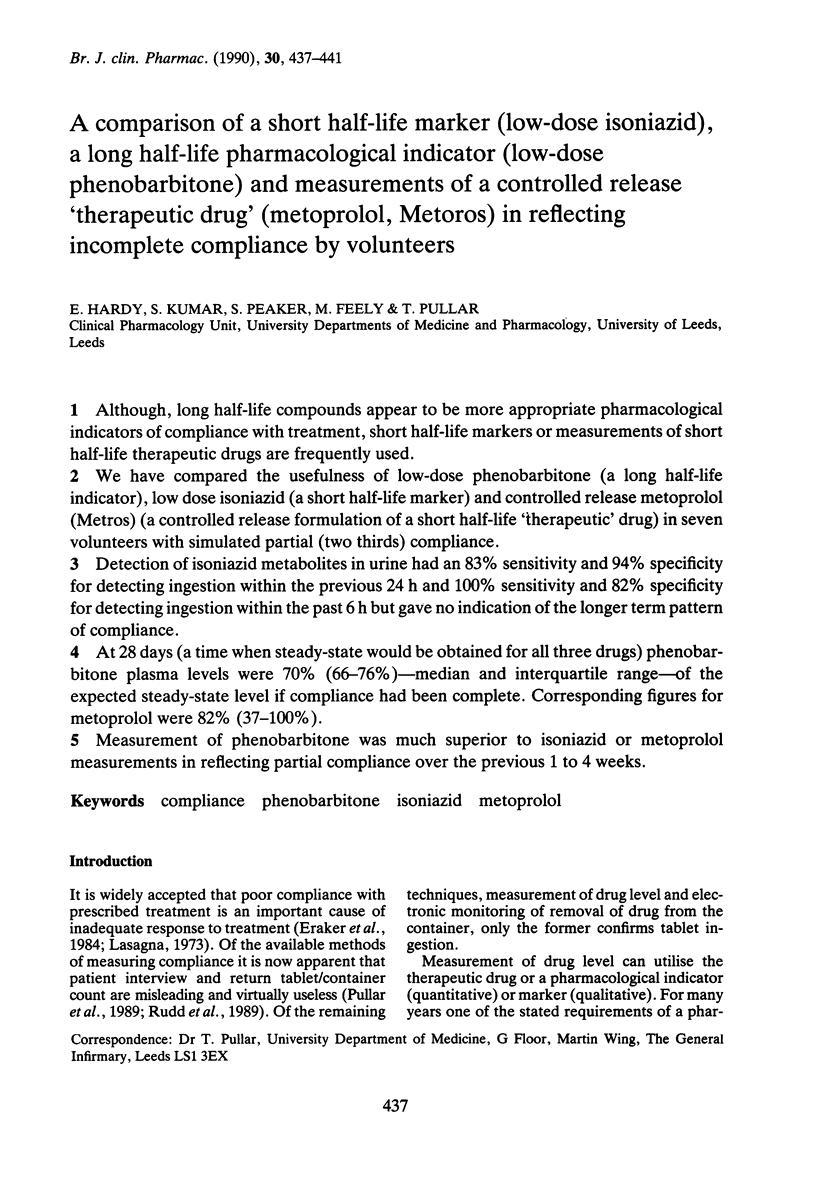
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cramer J. A., Mattson R. H., Prevey M. L., Scheyer R. D., Ouellette V. L. How often is medication taken as prescribed? A novel assessment technique. JAMA. 1989 Jun 9;261(22):3273–3277. [PubMed] [Google Scholar]
- Ellard G. A., Greenfield A sensitive urine-test method for monitoring the ingestion of isoniazid. J Clin Pathol. 1977 Jan;30(1):84–87. doi: 10.1136/jcp.30.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard G. A., Jenner P. J., Downs P. A. An evaluation of the potential use of isoniazid, acetylisoniazid and isonicotinic acid for monitoring the self-administration of drugs. Br J Clin Pharmacol. 1980 Oct;10(4):369–381. doi: 10.1111/j.1365-2125.1980.tb01773.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eraker S. A., Kirscht J. P., Becker M. H. Understanding and improving patient compliance. Ann Intern Med. 1984 Feb;100(2):258–268. doi: 10.7326/0003-4819-100-2-258. [DOI] [PubMed] [Google Scholar]
- Feely M., Cooke J., Price D., Singleton S., Mehta A., Bradford L., Calvert R. Low-dose phenobarbitone as an indicator of compliance with drug therapy. Br J Clin Pharmacol. 1987 Jul;24(1):77–83. doi: 10.1111/j.1365-2125.1987.tb03139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good W., Leeson L. J., Zak S. L., Wagner W. E., Meeker J. B., Arnold J. D. Oros controlled-release formulations of metoprolol: an approach to the development of a system for once daily administration. Br J Clin Pharmacol. 1985;19 (Suppl 2):231S–238S. doi: 10.1111/j.1365-2125.1985.tb02768.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordis L. General concepts for use of markers in clinical trials. Control Clin Trials. 1984 Dec;5(4 Suppl):481–487. doi: 10.1016/0197-2456(84)90008-4. [DOI] [PubMed] [Google Scholar]
- Insull W., Jr Statement of the problem and pharmacological and clinical requirements for the ideal marker. Control Clin Trials. 1984 Dec;5(4 Suppl):459–462. doi: 10.1016/0197-2456(84)90003-5. [DOI] [PubMed] [Google Scholar]
- Lasagna L. Fault and default. N Engl J Med. 1973 Aug 2;289(5):267–268. doi: 10.1056/NEJM197308022890511. [DOI] [PubMed] [Google Scholar]
- Mäenpä H., Javela K., Pikkarainen J., Mälkönen M., Heinonen O. P., Manninen V. Minimal doses of digoxin: a new marker for compliance to medication. Eur Heart J. 1987 Oct;8 (Suppl 1):31–37. doi: 10.1093/eurheartj/8.suppl_i.31. [DOI] [PubMed] [Google Scholar]
- Peaker S., Mehta A. C., Kumar S., Feely M. Measurement of low (sub-therapeutic) phenobarbitone levels in plasma by high-performance liquid chromatography: application to patient compliance studies. J Chromatogr. 1989 Dec 29;497:308–312. doi: 10.1016/0378-4347(89)80034-9. [DOI] [PubMed] [Google Scholar]
- Pearson R. M. Who is taking their tablets? Br Med J (Clin Res Ed) 1982 Sep 18;285(6344):757–758. doi: 10.1136/bmj.285.6344.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter A. M. Drug defaulting in a general practice. Br Med J. 1969 Jan 25;1(5638):218–222. doi: 10.1136/bmj.1.5638.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price D. E., Mehta A., Park B. K., Hay A., Feely M. P. The effect of low-dose phenobarbitone on three indices of hepatic microsomal enzyme induction. Br J Clin Pharmacol. 1986 Dec;22(6):744–747. doi: 10.1111/j.1365-2125.1986.tb02970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullar T., Birtwell A. J., Wiles P. G., Hay A., Feely M. P. Use of a pharmacologic indicator to compare compliance with tablets prescribed to be taken once, twice, or three times daily. Clin Pharmacol Ther. 1988 Nov;44(5):540–545. doi: 10.1038/clpt.1988.191. [DOI] [PubMed] [Google Scholar]
- Pullar T., Kumar S., Tindall H., Feely M. Time to stop counting the tablets? Clin Pharmacol Ther. 1989 Aug;46(2):163–168. doi: 10.1038/clpt.1989.121. [DOI] [PubMed] [Google Scholar]
- Pullar T., Peaker S., Martin M. F., Bird H. A., Feely M. P. The use of a pharmacological indicator to investigate compliance in patients with a poor response to antirheumatic therapy. Br J Rheumatol. 1988 Oct;27(5):381–384. doi: 10.1093/rheumatology/27.5.381. [DOI] [PubMed] [Google Scholar]
- Rudd P., Byyny R. L., Zachary V., LoVerde M. E., Titus C., Mitchell W. D., Marshall G. The natural history of medication compliance in a drug trial: limitations of pill counts. Clin Pharmacol Ther. 1989 Aug;46(2):169–176. doi: 10.1038/clpt.1989.122. [DOI] [PubMed] [Google Scholar]


