Abstract
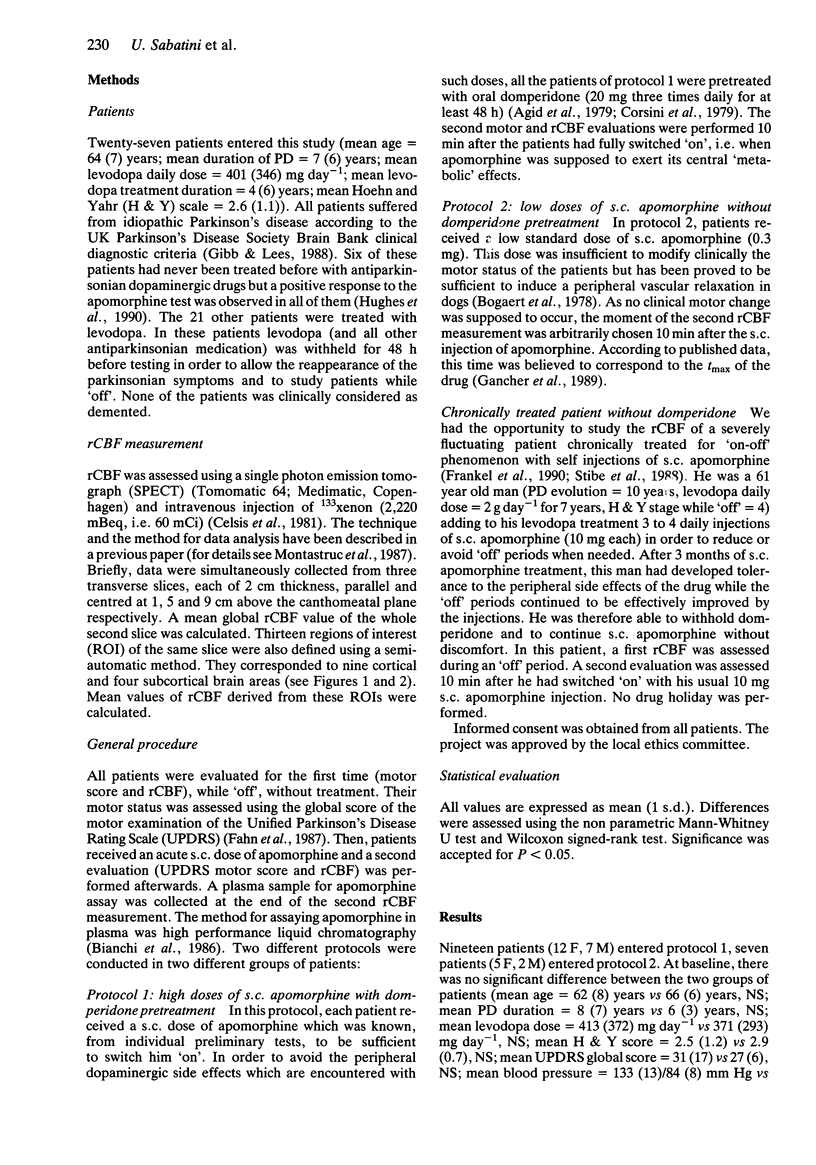
1. We have measured regional cerebral blood flow (rCBF) and motor function before and after the subcutaneous (s.c.) injection of apomorphine in parkinsonian patients deprived of their usual treatment for at least 48 h. 2. Nineteen patients, pretreated with domperidone (20 mg three times daily for 48 h), received a mean dose of 5.8 mg s.c. apomorphine. All patients switched 'on'. The mean motor score was significantly improved (-65%, P less than 0.01) but no significant change in rCBF was observed. 3. Seven other patients, not pretreated with domperidone, received a lower dose (0.3 mg) of s.c. apomorphine. No change in motor score was observed while the mean rCBF significantly increased (+12%, P less than 0.05). 4. We conclude that s.c. apomorphine increases rCBF in parkinsonian patients. This effect is independent of the central therapeutic effects of the drug. It is mediated by the stimulation of dopaminergic receptors of the cerebral vessels. These receptors are located outside the cerebral blood brain barrier and can be considered as 'peripheral' ones.
Full text
PDF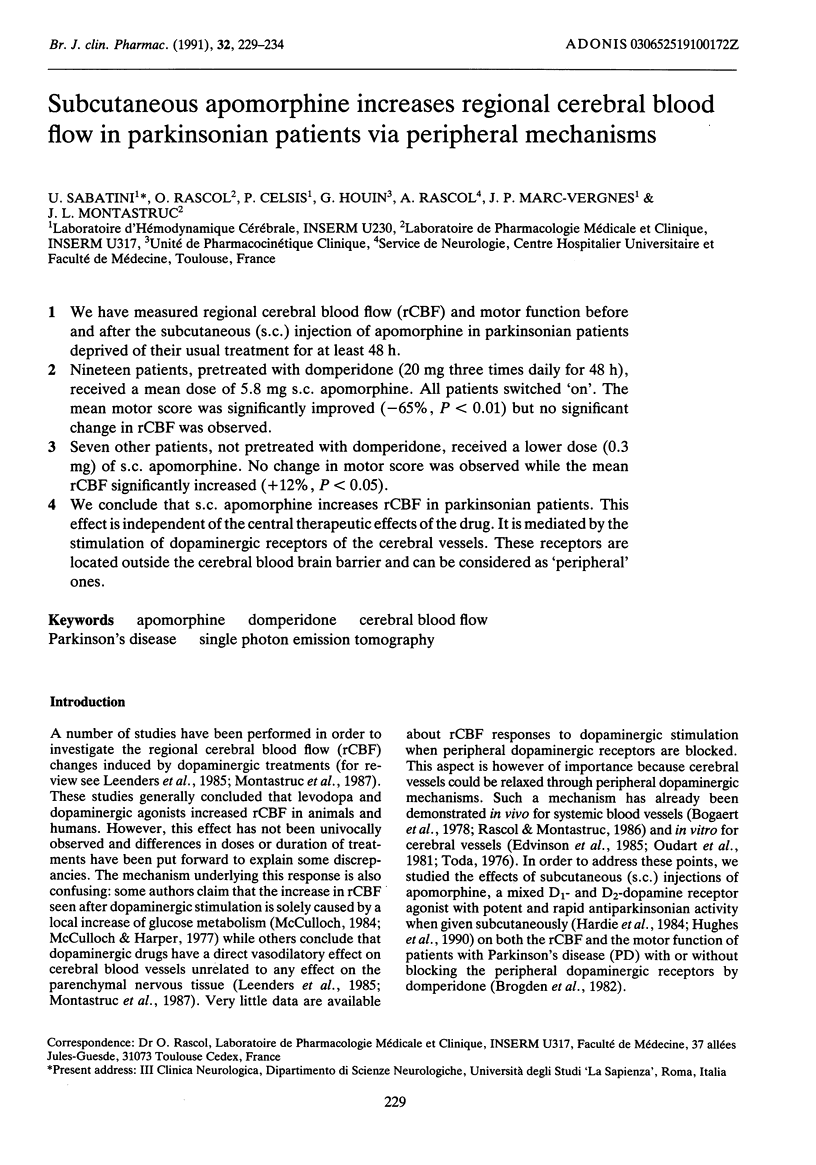
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agid Y., Pollak P., Bonnet A. M., Signoret J. L., Lhermitte F. Bromocriptine associated with a peripheral dopamine blocking agent in treatment of Parkinson's disease. Lancet. 1979 Mar 17;1(8116):570–572. doi: 10.1016/s0140-6736(79)91003-1. [DOI] [PubMed] [Google Scholar]
- Bianchi G., Landi M., Garattini S. Disposition of apomorphine in rat brain areas: relationship to stereotypy. Eur J Pharmacol. 1986 Nov 19;131(2-3):229–236. doi: 10.1016/0014-2999(86)90576-5. [DOI] [PubMed] [Google Scholar]
- Bogaert M. G., Buylaert W. A., Willems J. L. Hypotension produced by intravenous apomorphine in the anaesthetized dog is not centrally mediated. Br J Pharmacol. 1978 Jul;63(3):481–484. doi: 10.1111/j.1476-5381.1978.tb07801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brogden R. N., Carmine A. A., Heel R. C., Speight T. M., Avery G. S. Domperidone. A review of its pharmacological activity, pharmacokinetics and therapeutic efficacy in the symptomatic treatment of chronic dyspepsia and as an antiemetic. Drugs. 1982 Nov;24(5):360–400. doi: 10.2165/00003495-198224050-00002. [DOI] [PubMed] [Google Scholar]
- Celsis P., Goldman T., Henriksen L., Lassen N. A. A method for calculating regional cerebral blood flow from emission computed tomography of inert gas concentrations. J Comput Assist Tomogr. 1981 Oct;5(5):641–645. doi: 10.1097/00004728-198110000-00006. [DOI] [PubMed] [Google Scholar]
- Celsis P., Montastruc J. L., Rascol O., Senard J. M., Marc-Vergnes J. P., Rascol A. Effect of tropatepine, an anticholinergic drug, on regional cerebral blood flow in patients with Parkinson's disease. J Neurol Neurosurg Psychiatry. 1989 Jul;52(7):917–918. doi: 10.1136/jnnp.52.7.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celsis P., Rascol O., Demonet J. F., Agniel A., Montastruc J. L., Marc-Vergnes J. P., Rascol A. Effet de la bromocriptine sur le débit sanguin cérébral dans la maladie de Parkinson. Rev Neurol (Paris) 1988;144(5):367–371. [PubMed] [Google Scholar]
- Corsini G. U., Del Zompo M., Gessa G. L., Mangoni A. Therapeutic efficacy of apomorphine combined with an extracerebral inhibitor of dopamine receptors in Parkinson's disease. Lancet. 1979 May 5;1(8123):954–956. doi: 10.1016/s0140-6736(79)91725-2. [DOI] [PubMed] [Google Scholar]
- Edvinsson L., McCulloch J., Sharkey J. Vasomotor responses of cerebral arterioles in situ to putative dopamine receptor agonists. Br J Pharmacol. 1985 Jun;85(2):403–410. doi: 10.1111/j.1476-5381.1985.tb08875.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekström-Jodal B., von Essen C., Häggendal E., Roos B. E. Effects of L-dopa and L-tryptophan on the cerebral blood flow in the dog. Acta Neurol Scand. 1974;50(1):3–10. doi: 10.1111/j.1600-0404.1974.tb01342.x. [DOI] [PubMed] [Google Scholar]
- Frackowiak R. S., Lenzi G. L., Jones T., Heather J. D. Quantitative measurement of regional cerebral blood flow and oxygen metabolism in man using 15O and positron emission tomography: theory, procedure, and normal values. J Comput Assist Tomogr. 1980 Dec;4(6):727–736. doi: 10.1097/00004728-198012000-00001. [DOI] [PubMed] [Google Scholar]
- Frankel J. P., Lees A. J., Kempster P. A., Stern G. M. Subcutaneous apomorphine in the treatment of Parkinson's disease. J Neurol Neurosurg Psychiatry. 1990 Feb;53(2):96–101. doi: 10.1136/jnnp.53.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gancher S. T., Woodward W. R., Boucher B., Nutt J. G. Peripheral pharmacokinetics of apomorphine in humans. Ann Neurol. 1989 Aug;26(2):232–238. doi: 10.1002/ana.410260209. [DOI] [PubMed] [Google Scholar]
- Gibb W. R., Lees A. J. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson's disease. J Neurol Neurosurg Psychiatry. 1988 Jun;51(6):745–752. doi: 10.1136/jnnp.51.6.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandas F., Obeso J. A. Motor response following repeated apomorphine administration is reduced in Parkinson's disease. Clin Neuropharmacol. 1989 Feb;12(1):14–22. doi: 10.1097/00002826-198902000-00002. [DOI] [PubMed] [Google Scholar]
- Hardie R. J., Lees A. J., Stern G. M. On-off fluctuations in Parkinson's disease. A clinical and neuropharmacological study. Brain. 1984 Jun;107(Pt 2):487–506. doi: 10.1093/brain/107.2.487. [DOI] [PubMed] [Google Scholar]
- Henriksen L., Boas J. Regional cerebral blood flow in hemiparkinsonian patients. Emission computerized tomography of inhaled 133Xenon before and after levodopa. Acta Neurol Scand. 1985 Apr;71(4):257–266. doi: 10.1111/j.1600-0404.1985.tb03198.x. [DOI] [PubMed] [Google Scholar]
- Hughes A. J., Lees A. J., Stern G. M. Apomorphine test to predict dopaminergic responsiveness in parkinsonian syndromes. Lancet. 1990 Jul 7;336(8706):32–34. doi: 10.1016/0140-6736(90)91531-e. [DOI] [PubMed] [Google Scholar]
- Ingvar M., Lindvall O., Stenevi U. Apomorphine-induced changes in local cerebral blood flow in normal rats and after lesions of the dopaminergic nigrostriatal bundle. Brain Res. 1983 Mar 7;262(2):259–265. doi: 10.1016/0006-8993(83)91016-8. [DOI] [PubMed] [Google Scholar]
- Leenders K. L., Wolfson L., Gibbs J. M., Wise R. J., Causon R., Jones T., Legg N. J. The effects of L-DOPA on regional cerebral blood flow and oxygen metabolism in patients with Parkinson's disease. Brain. 1985 Mar;108(Pt 1):171–191. doi: 10.1093/brain/108.1.171. [DOI] [PubMed] [Google Scholar]
- Marc-Vergnes J. P., Celsis P., Montastruc J. L., Demonet J. F., Agniel A., Rascol O., Viallard G., Doyon B., Rascol A. Hémodynamique cérébrale et pharmacologie clinique dans la maladie de Parkinson. Therapie. 1988 Mar-Apr;43(2):83–88. [PubMed] [Google Scholar]
- Melamed E., Globus M., Mildworf B. Regional cerebral blood flow in patients with Parkinson's disease under chronic levodopa therapy: measurements during "on" and "off" response fluctuations. J Neurol Neurosurg Psychiatry. 1986 Nov;49(11):1301–1304. doi: 10.1136/jnnp.49.11.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montastruc J. L., Celsis P., Agniel A., Demonet J. F., Doyon B., Puel M., Marc-Vergnes J. P., Rascol A. Levodopa-induced regional cerebral blood flow changes in normal volunteers and patients with Parkinson's disease. Lack of correlation with clinical or neuropsychological improvements. Mov Disord. 1987;2(4):279–289. doi: 10.1002/mds.870020405. [DOI] [PubMed] [Google Scholar]
- Oudart N., Sercombe R., Aubineau P., Boulu R. G., Seylaz J. Relaxation by dopaminergic agonists in cerebral and peripheral arteries (in vitro). Arch Int Pharmacodyn Ther. 1981 Aug;252(2):196–209. [PubMed] [Google Scholar]
- Perlmutter J. S., Raichle M. E. Regional blood flow in hemiparkinsonism. Neurology. 1985 Aug;35(8):1127–1134. doi: 10.1212/wnl.35.8.1127. [DOI] [PubMed] [Google Scholar]
- Porrino L. J., Burns R. S., Crane A. M., Palombo E., Kopin I. J., Sokoloff L. Local cerebral metabolic effects of L-dopa therapy in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced parkinsonism in monkeys. Proc Natl Acad Sci U S A. 1987 Aug;84(16):5995–5999. doi: 10.1073/pnas.84.16.5995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rascol O. J., Montastruc J. L. Cardiovascular effects of apomorphine in humans: evidence for peripheral mechanisms. Clin Neuropharmacol. 1986;9(6):566–569. doi: 10.1097/00002826-198612000-00010. [DOI] [PubMed] [Google Scholar]
- Rougemont D., Baron J. C., Collard P., Bustany P., Comar D., Agid Y. Local cerebral glucose utilisation in treated and untreated patients with Parkinson's disease. J Neurol Neurosurg Psychiatry. 1984 Aug;47(8):824–830. doi: 10.1136/jnnp.47.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stibe C. M., Lees A. J., Kempster P. A., Stern G. M. Subcutaneous apomorphine in parkinsonian on-off oscillations. Lancet. 1988 Feb 20;1(8582):403–406. doi: 10.1016/s0140-6736(88)91193-2. [DOI] [PubMed] [Google Scholar]
- Toda N. Influence of dopamine and noradrenaline on isolated cerebral arteries of the dog. Br J Pharmacol. 1976 Sep;58(1):121–126. doi: 10.1111/j.1476-5381.1976.tb07700.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


