Dupuytren's disease is a common and disabling fibroproliferative condition of the hand. It tends to strike patients in advancing age, causing progressive digital flexion contracture. Through its many associations, Dupuytren's disease crosses all borders of medicine and is often encountered by surgeon, physician, and general practitioner alike. To the medical student, it is dependable examination fodder—a name on many lists and a sign of many systems.
The early history of Dupuytren's disease lies in folklore—it has been fabled somewhat contentiously for being a disease disseminated by the Vikings, an explanation for the curling of the papal “hand of benediction,” and a curse on the bagpipe craftsmanship of the MacCrimmon clan.1 The eminent surgeon Henry Cline introduced the condition into the medical literature and carried out the first surgical corrective procedures. The French surgeon Baron Dupuytren further developed Cline's observations and cemented his reputation by providing the eponym for the condition. We have reviewed the literature with the aim of highlighting important considerations in the management of patients with Dupuytren's disease, including a succinct overview of treatment options and referral guidelines.
Sources and selection criteria
We used PubMed and Medline search engines to identify seminal reviews, studies, and trials to clarify current knowledge of Dupuytren's disease. We used broad search terms to ensure that we identified all relevant papers. We cast the net further by scouring all reference lists to ensure that we omitted no important articles.
Presentation
Pitting and thickening of the palmar skin are the earliest manifestations of Dupuytren's disease. However, the key to early diagnosis is recognition of the nodule, a firm painless mass fixed to skin and deeper fascia. Classically, a nodule precedes development of a cord. Over time, which may be months or several years, the cord gradually contracts, reeling in the metacarpophalangeal joint and the proximal interphalangeal joint and leading to progressive digital flexion deformity (fig 1). Contracture is a common presenting complaint, although fear of malignancy or embarrassment of a handshake may precipitate the initial consultation. The condition most commonly affects the ring and little fingers, although any digit can be involved.2 The main consequence is impaired function. Contractures can affect activities at the workplace (manual labour, wearing gloves) and home (washing, dressing), posing a threat to independence.
Fig 1.


Dupuytren's cord, causing metacarpophalangeal and proximal interphalangeal contracture of the little finger
Summary points
Dupuytren's disease is a disabling condition common in elderly men
Treatment is often unnecessary, but regular follow-up is needed to detect early joint contracture
An appropriately timed referral to a surgical specialist before irreversible contracture develops can prevent a permanent loss of function
Injection with collagenase has shown early clinical promise for mild disease limited to the metacarpophalangeal joint
Surgery readily corrects contracture, but recurrence remains an unsolved problem
The condition is commonly bilateral and often associated with involvement of other areas of the body, so called ectopic disease—Garrod's knuckle pads (44-54%), plantar fibromatosis (Ledderhose disease, 6-31%), and penile fibromatosis (Peyronie's disease, 2-8%).3 A diathesis is recognised in Dupuytren's disease and describes disease affecting young white men with a strong family history, bilateral involvement, severe disease, and ectopic manifestations. Recognition of this clinical type is essential, as it carries a more serious prognosis and warrants aggressive follow-up and treatment.
Epidemiology
Dupuytren's disease typically affects elderly men of northern European descent. Prevalence varies widely according to the selected population, ranging from 2% to 42%.4 In the United Kingdom, more than 2 million people are thought to have the condition. A strong familial component is recognised, and the pattern of inheritance has been suggested to be autosomal dominant with variable penetrance. Men typically present earlier (mean age 55 years) than women (10 years later) and have more severe disease.5
Associations
As illustrated in the box, Dupuytren's disease has many recognised associations. Smoking and excessive alcohol intake are independent risk factors for disease development, and in both cases the relation is dose dependent (odds ratio 1.5-2 for smoking and 1.35-4.2 for alcohol).6 Chronic liver disease is not a risk factor independent of alcohol consumption.7 The condition is more prevalent among people with diabetes, especially those dependent on insulin.6 Diabetic patients tend to have a milder form of the disease. Patients with Dupuytren's disease have also been noted to have raised serum lipids compared with controls.w1 Controversy exists as to the significance of either anticonvulsant drugs or epilepsy.8
Dupuytren suggested a possible association between development of the condition and holding the reigns of horses. Nearly 200 years later, as many studies have established a relation between Dupuytren's disease and manual labour as have refuted it.9 Most experts would concede, however, that a one-off hand injury can rarely trigger Dupuytren's disease and that a history of manual labour indicates a worse prognosis.
Factors associated with Dupuytren's disease
Smoking
Alcohol
Diabetes mellitus
Anticonvulsants
Epilepsy
Hypercholesterolaemia
Manual labour
Hand trauma
Pathophysiology
Although the cause of Dupuytren's disease remains unknown, much has been uncovered about the associated cellular and connective tissue changes. It is classified as a fibroproliferative disorder in a group that includes keloid scars. Fibroblast proliferation is a key feature of early Dupuytren's disease and manifests clinically as the nodule.10 In these early stages, Dupuytren's disease shares certain properties with malignant tumours and histologically often resembles fibrosarcoma.11 As the disease progresses, proliferation fizzles out and connective tissue assembles, manifesting clinically as the cord.
Parallels have been drawn between Dupuytren's disease and wound healing.12 As well as cellular proliferation, both conditions are marked by collagen type III deposition.13 Similarly, the myofibroblast, a contractile cell derived from fibroblast differentiation, is prominent in both granulation tissue, where it assists wound closure, and Dupuytren's tissue, where it may be the engine behind contracture.14 The healing wound is an environment rich in biologically active molecules that coordinate repair. Up-regulation of various growth factors and their receptors has also been shown in Dupuytren's tissue, including transforming growth factor β and basic fibroblast growth factor.15 What injurious events might precipitate a “wound healing” response in Dupuytren's disease is unknown, although hypoxia induced free radicals and microtrauma of collagen fibres have been suggested as possible triggers.w2 w3
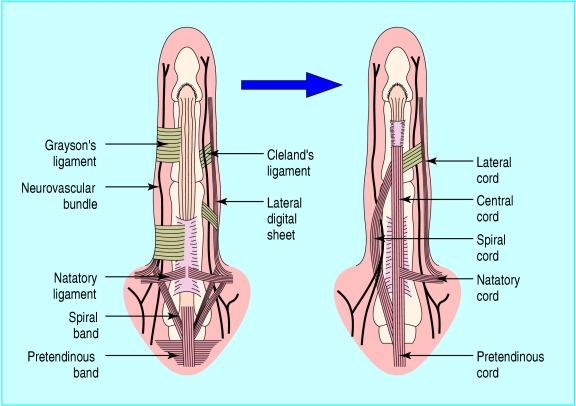
Anatomy
An appreciation of the normal anatomy is the key to understanding the deformities of Dupuytren's disease and the surgical basis of their correction. Dupuytren's disease affects the palmar fascial complex, a tough aponeurotic sheet that lies deep to the dermis and superficial to the flexor tendons and small muscles of the hand. It fans outwards from the wrist across the palm, proceeding distally first as the palmo-digital fascia and finally the digital fascia. Within each digit, the fibres of fascia continue longitudinally as the pretendinous band, the spiral band, and the lateral digital sheet (fig 2). As well as protecting deeper structures, notably the neurovascular bundle, the palmar fascia allows conformation of the palmar skin to assist in grasping objects.
Fig 2.
Normal elements of the digital fascia (left) and the diseased fascia of Dupuytren's disease (right)
The clinical presentation of Dupuytren's disease can be explained in terms of a distortion of the normal palmar fascia. Skin pitting is a result of involvement of small vertical fibres (Grapow fibres) that connect the dermis to the palmar fascia. Nodules develop from the superficial fibres of the palmo-digital fascia, adhere to the overlying skin, and usually precede cords.3 The affected bands of the digital fascia are referred to as cords (table).10 Contraction of cords results in predictable deformity as they cross joints—the pretendinous cord causes flexion contracture at the metacarpophalangeal joint; the lateral digital sheet becomes the lateral cord and causes flexion of the proximal interphalangeal joint through its attachment to Grayson's ligament. The spiral cord is responsible for both proximal interphalangeal joint contracture and superficial displacement of the neurovascular bundle, making it more susceptible to accidental division at surgery.
Table 1.
Joint deformities associated with diseased cords
| Normal structure | Pathological cord | Action |
|---|---|---|
| Pretendinous band | Pretendinous cord | MCPJ deformity |
| Natatory ligament | Natatory cord | Limits digital abduction |
| Central fibrofatty tissue | Central cord | PIPJ deformity |
| Spiral band | Spiral cord | Displaces neurovascular bundle superficially |
| Lateral digital sheet | Lateral cord | PIPJ/DIPJ contracture |
DIPJ=distal interphalangeal joint; MCPJ=metacarpophalangeal joint;
PIPJ=proximal interphalangeal joint.
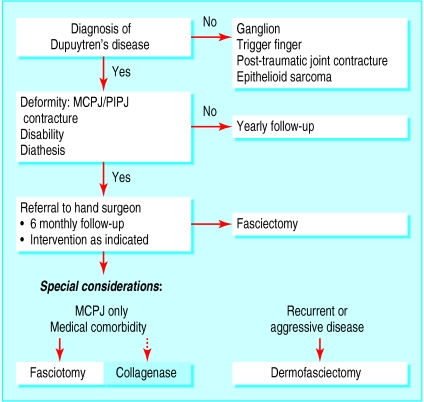
Treatment
Most patients with Dupuytren's disease do not need treatment and can be managed expectantly. Intervention is almost exclusively surgical and should be considered when function is impeded or deformity is disabling. All patients must be assessed on an individual basis and the nature of the disability characterised, especially noting use of hands at work and home. Referral to a specialist is advisable when contracture develops. The longer the deformity prevails, the greater the chance of joint contracture becoming irreversible as ligaments remodel in the contracted position. This is especially true of proximal interphalangeal joint contracture, and the first sign of such contracture should precipitate referral to a hand surgeon. Figure 3 illustrates a proposed management algorithm.
Fig 3.
Management algorithm for Dupuytren's disease. MCPJ=metacarpophalangeal joint; PIPJ=proximal interphalangeal joint
Non-operative treatment
Despite much unravelling of the biochemical and cellular processes underlying Dupuytren's disease, this has not so far been translated into medical treatment. Several non-operative treatments, including radiotherapy, splinting, steroids, and topical vitamin A, have been tried and tested,w4 w5 but none has gained popularity. Preliminary observations suggest that intralesional interferon gamma may reduce the size of Dupuytren's cords, although further validation from controlled studies is awaited.16 The enzyme collagenase, derived from Clostridium histolyticum, has shown early clinical promise. It can be injected under ultrasound guidance directly into the cord, breaking the lesion down by enzymic fasciotomy. A randomised placebo controlled double blind trial concluded that it was a safe and effective means of correcting contracture, although results of phase III trials and long term recurrence rates are awaited before firm conclusions can be made.17
Surgical correction
The aim of surgery is to restore function and correct deformity with minimal complications. Accepted indications for surgical intervention include metacarpophalangeal joint contracture of 30° and any degree of proximal interphalangeal joint contracture.18 Broadly speaking, surgical options involve either fasciotomy, in which the cord is simply divided, or fasciectomy, in which the diseased fascia is excised. Fasciotomy is indicated for isolated metacarpophalangeal joint contracture and can be done as an open procedure or percutaneously (needle fasciotomy) in the outpatient setting.19 Early recurrence is a common complication after simple fasciotomy, making it most suitable for patients in whom major surgery is contraindicated.20
Fasciectomy can be done under regional anaesthetic (axillary block) or general anaesthetic as a day surgery procedure or an inpatient overnight stay. Zigzag incisions along natural palmar and digital creases prevent volar contractures and allow adequate exposure. Fasciectomy can be either limited, where all macroscopically diseased tissue is excised, or radical, where all palmar fascia is excised. Digital amputation is sometimes indicated in cases of severe, irreversible joint contracture. Closure of the wound can be problematic; often, inadequate skin is available for direct closure. Z-plasties enable partial lengthening of the contracted palmar skin. Some surgeons advocate leaving the wound open (open palm technique) as postoperative pain is reduced and early mobilisation is possible.21 Other surgeons close palmar wounds with full thickness skin grafts.
Postoperatively, the hand is splinted initially in the position of function (45-70° metacarpophalangeal joint flexion, interphalangeal joint extension). Hand physiotherapy is started immediately to prevent stiffness, retain the new range of motion, and restore strength and function. An extension splint enabling serial metacarpophalangeal joint extension over time is worn at night for three months. Intraoperative complications are rare (1-2%) and include digital nerve or vessel injury and buttonholing of skin flaps.22 In the early postoperative period, haematoma, infection, and flap necrosis occur relatively frequently (19%).w6 Such wound complications may be reduced by segmental aponeurectomy, which involves a more minimal dissection than fasciectomy.23 Recurrence is common after surgery (up to 60%), especially in patients with aggressive disease (fig 4).24 Little progress has been made in reducing recurrence, although dermofasciectomy, in which diseased fascia and overlying skin are simultaneously removed, may delay return of disease.25 Extension of disease into previously untreated areas is also a common feature of Dupuytren's disease.
Fig 4.

Recurrent contracture
Prognosis
Many patients with Dupuytren's disease will not develop contracture and can be managed expectantly. Where indicated, surgery readily corrects deformity and can prevent irreversible contracture at an acceptable risk. Although restoration of premorbid function is unlikely, most patients can expect a significant improvement in hand function and can return to work. However, patients should be made aware that surgery does not cure the disease and that, over time, extension and recurrence are likely. Patients with a recognised diathesis carry the worst prognosis and are likely to be troubled by aggressive and recurrent disease.
Patient's story
Mr P is a 70 year old, right handed man who was returning to hospital for his eighth Dupuytren's operation when I spoke to him. He had presented to his general practitioner 10 years earlier on recognising the telltale finger contracture of Dupuytren's disease, just as his father had had previously. As managing director of a flag manufacturing business, the illness had not interfered with his work. It was, however, proving an unrelenting burden on daily activities, making it difficult to retrieve his wallet from his pocket, applaud at the theatre, and strike a golf ball. When he washed his face, the contracted little finger poked him in the eye. He had surgery to correct contracture of both right and left little fingers. Despite diligent adherence to hand therapy, including regular ultrasound to reduce scarring and wearing a night splint for three months, the disease returned. When I saw him, he had had multiple operations on both hands and had recently had his left little finger amputated as a result of irreversible scarring and joint adhesions. He was upbeat about the proposed new surgery, however, noting the extra facility that every operation had granted him in the past and the absence of any effective alternative.
Additional educational resources
eMedicine (www.emedicine.com)—detailed overview from a leading American based e-learning website
National Institute for Health and Clinical Excellence (www.nice.org.uk)—evidence based guidelines for needle fasciotomy
Information for patients
American Society for Surgery of the Hand (www.assh.org)—detailed yet simple to follow explanation of Dupuytren's disease for patients
Patient UK (www.patient.co.uk)—patient oriented advice about Dupuytren's disease, with links to support groups
E-hand (www.e-hand.com)—contains a well illustrated section on Dupuytren's disease
Supplementary Material
 References w1-w6 are on bmj.com
References w1-w6 are on bmj.com
Contributors: RB and NS wrote the sections on presentation, associations, anatomy, and surgical management. AOG edited the final version.
Competing interests: None declared.
References
- 1.Elliot D. The early history of Dupuytren's disease. Hand Clin 1999;15: 1-19, v. [PubMed] [Google Scholar]
- 2.Mikkelsen OA. Dupuytren's disease—a study of the pattern of distribution and stage of contracture in the hand. Hand 1976;8: 265-71. [DOI] [PubMed] [Google Scholar]
- 3.Rayan GM. Clinical presentation and types of Dupuytren's disease. Hand Clin 1999;15: 87-96, vii. [PubMed] [Google Scholar]
- 4.Ross DC. Epidemiology of Dupuytren's disease. Hand Clin 1999;15: 53-62, vi. [PubMed] [Google Scholar]
- 5.Gudmundsson KG, Arngrimsson R, Sigfusson N, Bjornsson A, Jonsson T. Epidemiology of Dupuytren's disease: clinical, serological, and social assessment. The Reykjavik study. J Clin Epidemiol 2000;53: 291-6. [DOI] [PubMed] [Google Scholar]
- 6.Godtfredsen NS, Lucht H, Prescott E, Sorensen TI, Gronbaek M. A prospective study linked both alcohol and tobacco to Dupuytren's disease. J Clin Epidemiol 2004;57: 858-63. [DOI] [PubMed] [Google Scholar]
- 7.Attali P, Ink O, Pelletier G, Vernier C, Jean F, Moulton L, et al. Dupuytren's contracture, alcohol consumption, and chronic liver disease. Arch Intern Med 1987;147: 1065-7. [PubMed] [Google Scholar]
- 8.Geoghegan JM, Forbes J, Clark DI, Smith C, Hubbard R. Dupuytren's disease risk factors. J Hand Surg [Br] 2004;29: 423-6. [DOI] [PubMed] [Google Scholar]
- 9.McFarlane RM. Dupuytren's disease: relation to work and injury. J Hand Surg [Am] 1991;16: 775-9. [DOI] [PubMed] [Google Scholar]
- 10.Luck JV. Dupuytren's contracture; a new concept of the pathogenesis correlated with surgical management. J Bone Joint Surg Am 1959;41-A(4): 635-64. [PubMed] [Google Scholar]
- 11.Jemec B, Grobbelaar AO, Wilson GD, Smith PJ, Sanders R, McGrouther DA. Is Dupuytren's disease caused by an imbalance between proliferation and cell death? J Hand Surg [Br] 1999;24: 511-4. [DOI] [PubMed] [Google Scholar]
- 12.Fitzgerald AM, Kirkpatrick JJ, Naylor IL. Dupuytren's disease: the way forward? J Hand Surg [Br] 1999;24: 395-9. [DOI] [PubMed] [Google Scholar]
- 13.Brickley-Parsons D, Glimcher MJ, Smith RJ, Albin R, Adams JP. Biochemical changes in the collagen of the palmar fascia in patients with Dupuytren's disease. J Bone Joint Surg Am 1981;63: 787-97. [PubMed] [Google Scholar]
- 14.Bisson MA, McGrouther DA, Mudera V, Grobbelaar AO. The different characteristics of Dupuytren's disease fibroblasts derived from either nodule or cord: expression of alpha-smooth muscle actin and the response to stimulation by TGF-beta1. J Hand Surg [Br] 2003;28: 351-6. [DOI] [PubMed] [Google Scholar]
- 15.Baird KS, Crossan JF, Ralston SH. Abnormal growth factor and cytokine expression in Dupuytren's contracture. J Clin Pathol 1993;46: 425-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pittet B, Rubbia-Brandt L, Desmouliere A, Sappino AP, Roggero P, Guerret S, et al. Effect of gamma-interferon on the clinical and biologic evolution of hypertrophic scars and Dupuytren's disease: an open pilot study. Plast Reconstr Surg 1994;93: 1224-35. [DOI] [PubMed] [Google Scholar]
- 17.Badalamente MA, Hurst LC, Hentz VR. Collagen as a clinical target: nonoperative treatment of Dupuytren's disease. J Hand Surg [Am] 2002;27: 788-98. [DOI] [PubMed] [Google Scholar]
- 18.Smith AC. Diagnosis and indications for surgical treatment. Hand Clin 1991;7: 635-42, discussion 643. [PubMed] [Google Scholar]
- 19.Bryan AS, Ghorbal MS. The long-term results of closed palmar fasciotomy in the management of Dupuytren's contracture. J Hand Surg [Br] 1988;13: 254-6. [DOI] [PubMed] [Google Scholar]
- 20.Foucher G, Medina J, Navarro R. Percutaneous needle aponeurotomy: complications and results. J Hand Surg [Br] 2003;28: 427-31. [DOI] [PubMed] [Google Scholar]
- 21.McCash CR. The open palm technique in Dupuytren's contracture. Br J Plast Surg 1964;17: 271-80. [DOI] [PubMed] [Google Scholar]
- 22.Bulstrode NW, Jemec B, Smith PJ. The complications of Dupuytren's contracture surgery. J Hand Surg [Am] 2005;30: 1021-5. [DOI] [PubMed] [Google Scholar]
- 23.Moermans JP. Long-term results after segmental aponeurectomy for Dupuytren's disease. J Hand Surg [Br] 1996;21: 797-800. [DOI] [PubMed] [Google Scholar]
- 24.Rodrigo JJ, Niebauer JJ, Brown RL, Doyle JR. Treatment of Dupuytren's contracture: long-term results after fasciotomy and fascial excision. J Bone Joint Surg Am 1976;58: 380-7. [PubMed] [Google Scholar]
- 25.Hall PN, Fitzgerald A, Sterne GD, Logan AM. Skin replacement in Dupuytren's disease. J Hand Surg [Br] 1997;22: 193-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.