Abstract
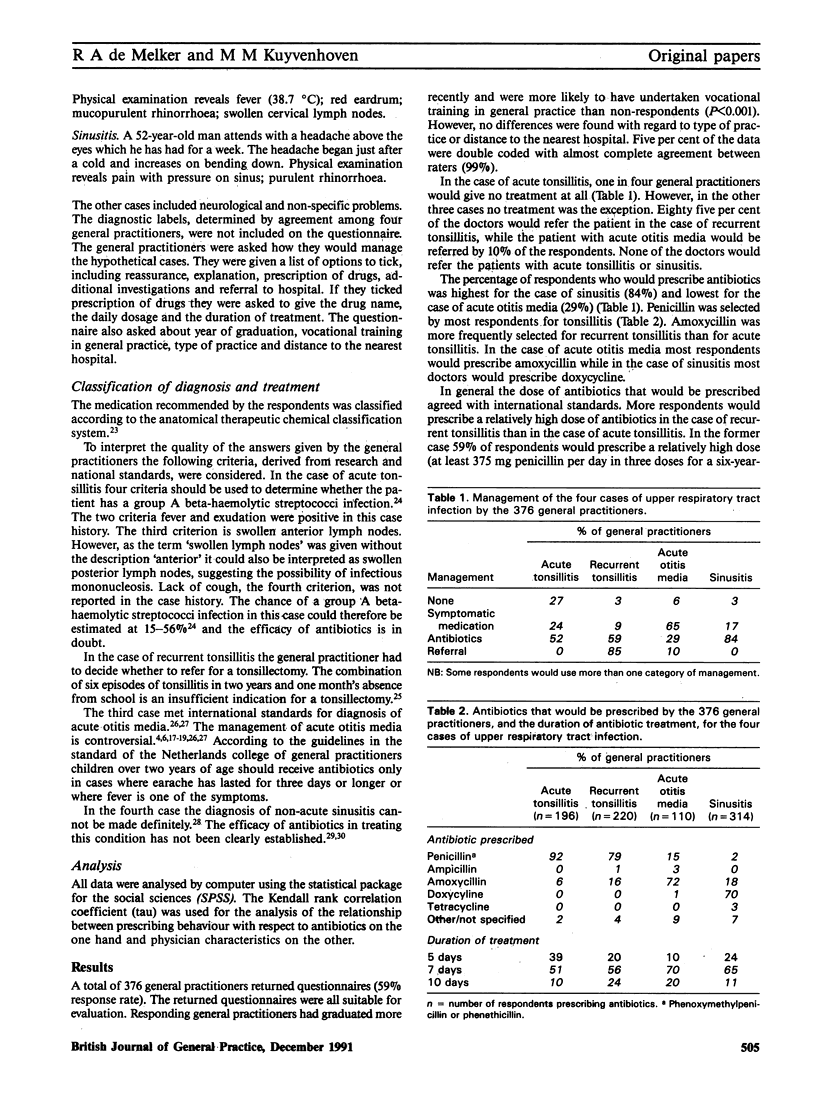
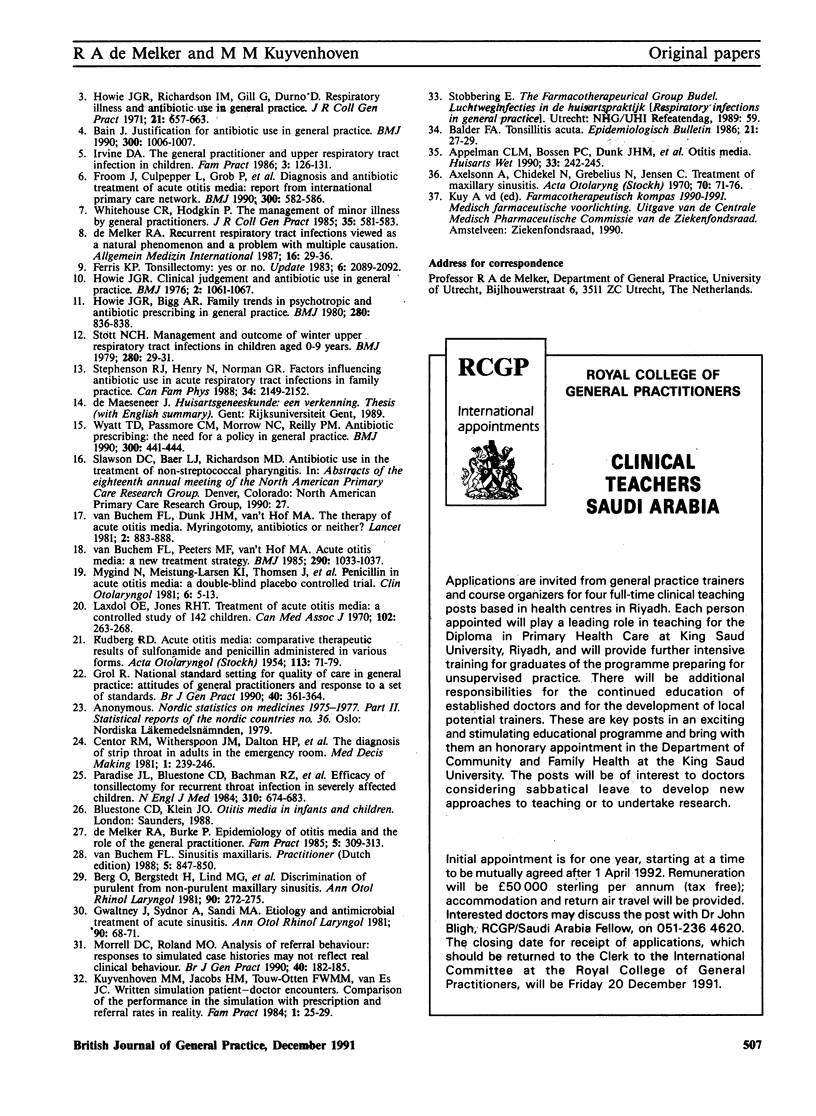
A questionnaire, sent to a 10% random sample of Dutch general practitioners (n = 635) included descriptions of four cases of upper respiratory tract infections (acute tonsillitis, recurrent tonsillitis, acute otitis media and sinusitis). This was used to study the general practitioners' management of upper respiratory tract infections. A total of 376 doctors responded (59%). The majority of general practitioners would prescribe antibiotics for sinusitis (80% of respondents) but only 29% would prescribe antibiotics for acute otitis media. For acute tonsillitis and recurrent tonsillitis the proportions were 52% and 59%, respectively. The low prescription rate for acute otitis media was in accordance with national standards, such as the standard of the Netherlands college of general practitioners. A penicillin (phenoxymethylpenicillin or phenethicillin) was most likely to be selected for the two types of tonsillitis, amoxycillin for acute otitis media and doxycycline for sinusitis. Other antibiotics such as erythromycin, other tetracyclines and ampicillin, were seldom selected. Most respondents would prescribe antibiotics for seven days, but there was considerable variation. The influence of the characteristics of the general practitioners and their practices on their antibiotic prescribing was small. Only type of practice correlated with antibiotic treatment, in that general practitioners in single-handed practices would prescribe antibiotics more often than their colleagues in health centres. Among those who would prescribe symptomatic treatment nearly all would prescribe nosedrops for acute otitis media and sinusitis. Eighty five per cent of the respondents would refer the patient with recurrent tonsillitis, while 10% would refer the patient with acute otitis media. The results suggest that some aspects of the prescribing behaviour of Dutch general practitioners might be improved.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Albers H. E., Pollock J., Simmons W. H., Ferris C. F. A V1-like receptor mediates vasopressin-induced flank marking behavior in hamster hypothalamus. J Neurosci. 1986 Jul;6(7):2085–2089. doi: 10.1523/JNEUROSCI.06-07-02085.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson A., Chidekel N., Grebelius N., Jensen C. Treatment of acute maxillary sinusitis. A comparison of four different methods. Acta Otolaryngol. 1970 Jul;70(1):71–76. doi: 10.3109/00016487009181861. [DOI] [PubMed] [Google Scholar]
- Bain J. Childhood otalgia: acute otitis media. 2. Justification for antibiotic use in general practice. BMJ. 1990 Apr 14;300(6730):1006–1007. doi: 10.1136/bmj.300.6730.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg O., Bergstedt H., Carenfelt C., Lind M. G., Perols O. Discrimination of purulent from nonpurulent maxillary sinusitis. Clinical and radiographic diagnosis. Ann Otol Rhinol Laryngol. 1981 May-Jun;90(3 Pt 1):272–275. doi: 10.1177/000348948109000316. [DOI] [PubMed] [Google Scholar]
- Centor R. M., Witherspoon J. M., Dalton H. P., Brody C. E., Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making. 1981;1(3):239–246. doi: 10.1177/0272989X8100100304. [DOI] [PubMed] [Google Scholar]
- De Melker R. A., Burke P. D. Epidemiology of otitis media and the role of the general practitioner in management. Fam Pract. 1988 Dec;5(4):307–313. doi: 10.1093/fampra/5.4.307. [DOI] [PubMed] [Google Scholar]
- Froom J., Culpepper L., Grob P., Bartelds A., Bowers P., Bridges-Webb C., Grava-Gubins I., Green L., Lion J., Somaini B. Diagnosis and antibiotic treatment of acute otitis media: report from International Primary Care Network. BMJ. 1990 Mar 3;300(6724):582–586. doi: 10.1136/bmj.300.6724.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol R. National standard setting for quality of care in general practice: attitudes of general practitioners and response to a set of standards. Br J Gen Pract. 1990 Sep;40(338):361–364. [PMC free article] [PubMed] [Google Scholar]
- Gwaltney J. M., Jr, Sydnor A., Jr, Sande M. A. Etiology and antimicrobial treatment of acute sinusitis. Ann Otol Rhinol Laryngol Suppl. 1981 May-Jun;90(3 Pt 3):68–71. doi: 10.1177/00034894810903s216. [DOI] [PubMed] [Google Scholar]
- Howie J. G., Bigg A. R. Family trends in psychotropic and antibiotic prescribing in general practice. Br Med J. 1980 Mar 22;280(6217):836–838. doi: 10.1136/bmj.280.6217.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howie J. G. Clinical judgement and antibiotic use in general practice. Br Med J. 1976 Oct 30;2(6043):1061–1064. doi: 10.1136/bmj.2.6043.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howie J. G., Richardson I. M., Gill G., Durno D. Respiratory illness and antibiotic use in general practice. J R Coll Gen Pract. 1971 Nov;21(112):657–663. [PMC free article] [PubMed] [Google Scholar]
- Irvine D. A. The general practitioner and upper respiratory tract infection in childhood. Fam Pract. 1986 Jun;3(2):126–131. doi: 10.1093/fampra/3.2.126. [DOI] [PubMed] [Google Scholar]
- Kuyvenhoven M. M., Jacobs H. M., Touw-Otten F. W., van Es J. C. Written simulation of patient-doctor encounters. 3. Comparison of the performance in the simulation with prescription and referral data in reality. Fam Pract. 1984 Mar;1(1):25–29. doi: 10.1093/fampra/1.1.25. [DOI] [PubMed] [Google Scholar]
- Laxdal O. E., Merida J., Jones R. H. Treatment of acute otitis media: a controlled study of 142 children. Can Med Assoc J. 1970 Feb 14;102(3):263–268. [PMC free article] [PubMed] [Google Scholar]
- Morrell D. C., Roland M. O. Analysis of referral behaviour: responses to simulated case histories may not reflect real clinical behaviour. Br J Gen Pract. 1990 May;40(334):182–185. [PMC free article] [PubMed] [Google Scholar]
- Mygind N., Meistrup-Larsen K. I., Thomsen J., Thomsen V. F., Josefsson K., Sørensen H. Penicillin in acute otitis media: a double-blind placebo-controlled trial. Clin Otolaryngol Allied Sci. 1981 Feb;6(1):5–13. doi: 10.1111/j.1365-2273.1981.tb01781.x. [DOI] [PubMed] [Google Scholar]
- Paradise J. L., Bluestone C. D., Bachman R. Z., Colborn D. K., Bernard B. S., Taylor F. H., Rogers K. D., Schwarzbach R. H., Stool S. E., Friday G. A. Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials. N Engl J Med. 1984 Mar 15;310(11):674–683. doi: 10.1056/NEJM198403153101102. [DOI] [PubMed] [Google Scholar]
- RUDBERG R. D. Acute otitis media; comparative therapeutic results of sulphonamide and penicillin administered in various forms. Acta Otolaryngol Suppl. 1954;113:1–79. [PubMed] [Google Scholar]
- Whitehouse C. R., Hodgkin P. The management of minor illness by general practitioners. J R Coll Gen Pract. 1985 Dec;35(281):581–583. [PMC free article] [PubMed] [Google Scholar]
- Wyatt T. D., Passmore C. M., Morrow N. C., Reilly P. M. Antibiotic prescribing: the need for a policy in general practice. BMJ. 1990 Feb 17;300(6722):441–444. doi: 10.1136/bmj.300.6722.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buchem F. L., Dunk J. H., van't Hof M. A. Therapy of acute otitis media: myringotomy, antibiotics, or neither? A double-blind study in children. Lancet. 1981 Oct 24;2(8252):883–887. doi: 10.1016/s0140-6736(81)91388-x. [DOI] [PubMed] [Google Scholar]
- van Buchem F. L., Peeters M. F., van 't Hof M. A. Acute otitis media: a new treatment strategy. Br Med J (Clin Res Ed) 1985 Apr 6;290(6474):1033–1037. doi: 10.1136/bmj.290.6474.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]


