Abstract
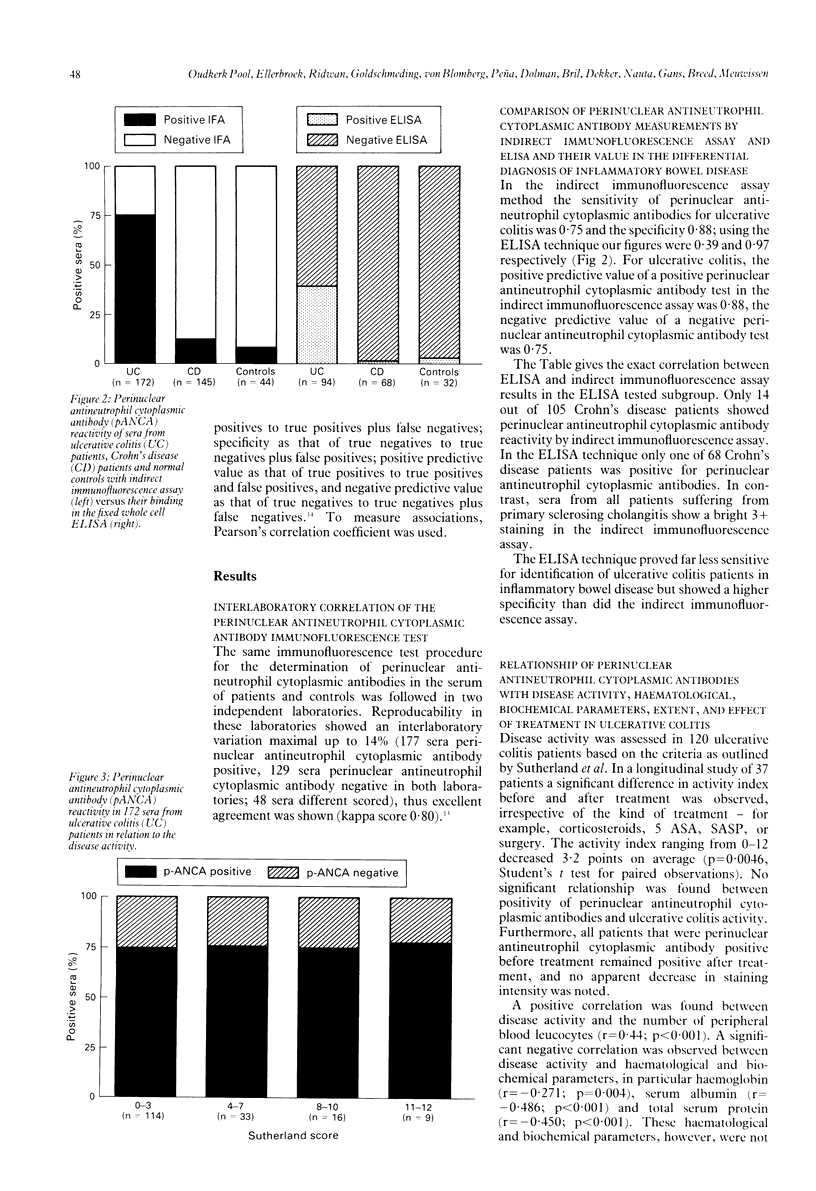
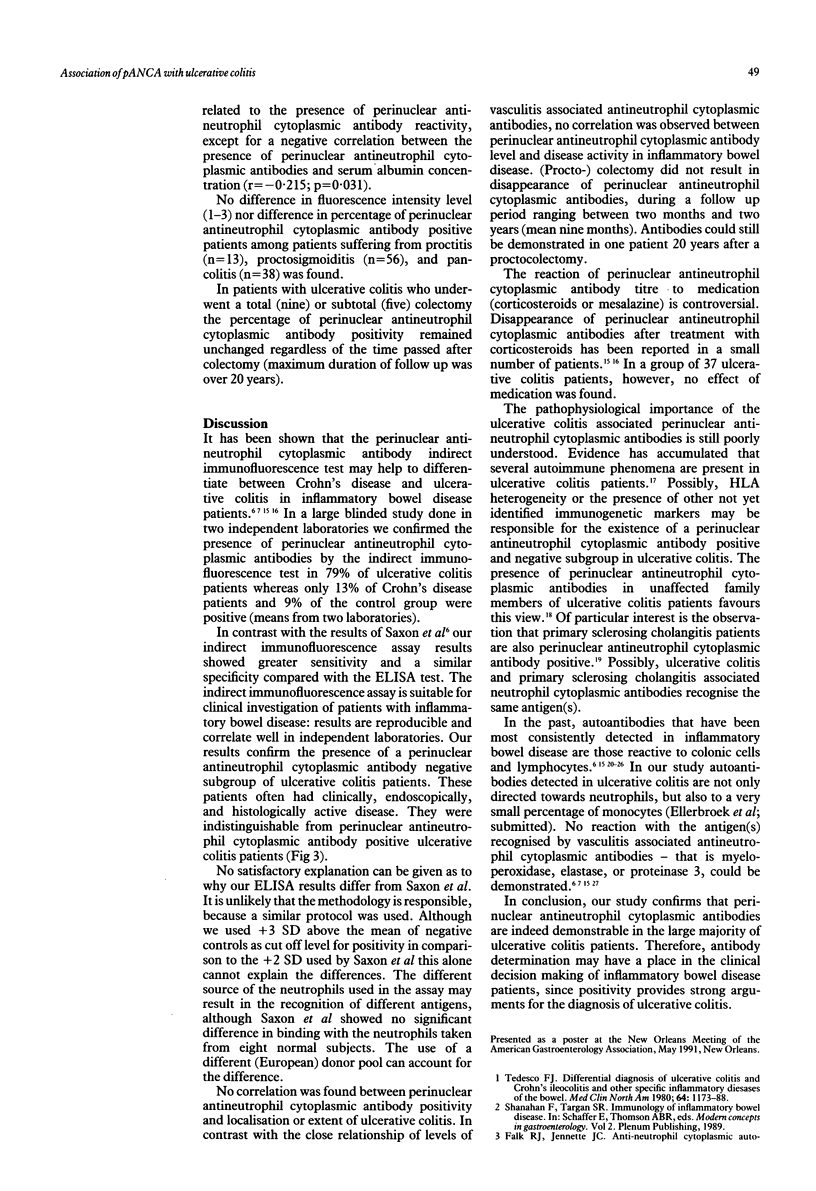
Perinuclear antineutrophil cytoplasmic antibodies have recently been demonstrated in the sera of patients with inflammatory bowel disease. Three hundred and sixty six sera obtained from 120 patients with ulcerative colitis, 105 patients suffering from Crohn's disease and 49 non-inflammatory bowel disease controls were tested in two laboratories, using an indirect immunofluorescence assay. In addition, a fixed-neutrophil enzyme linked immunoadsorbent assay (ELISA) was evaluated in one of the two laboratories. The results in the immunofluorescence test showed a high degree of correlation between the two laboratories (Kappa coefficient = 0.8). Ninety five of the 120 (79%) ulcerative colitis patients had a positive test whereas only 14 of the 105 (13%) patients with Crohn's disease were positive. Sera from four patients suffering from primary sclerosing cholangitis were positive as well as four of the 45 control sera (9%). The sensitivity of the perinuclear antineutrophil cytoplasmic antibody immunofluorescence test for the diagnosis of ulcerative colitis was 0.75 with a specificity of 0.88 and a positive predictive value of 0.88 (all sera). In the ELISA technique 37 of 94 ulcerative colitis sera and one of the 68 Crohn's disease sera were positive. In the control group only one of the patients suffering from primary sclerosing cholangitis reacted positively (32 non-inflammatory bowel disease sera tested). The ELISA technique had a high specificity (0.97), but a low sensitivity (0.39). There was no relation of perinuclear antineutrophil cytoplasmic antibodies in ulcerative colitis patients or in Crohn's disease patients with disease activity, duration of illness, localisation, extent of disease, previous bowel operations or medical treatment. The clinical significance of perinuclear antineutrophil cytoplasmic antibody positive and negative subsets in both groups of patients thus remains unexplained. Our study confirms that determination of serum antineutrophil cytoplasmatic antibodies in patients with inflammatory bowel disease may differentiate ulcerative colitis from Crohn's disease. Further immunological studies are needed to explain the absence of these antibodies in a subset of ulcerative colitis patients and their role in the pathogenesis of the disease.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BROBERGER O., PERLMANN P. Autoantibodies in human ulcerative colitis. J Exp Med. 1959 Nov 1;110:657–674. doi: 10.1084/jem.110.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best W. R., Becktel J. M., Singleton J. W. Rederived values of the eight coefficients of the Crohn's Disease Activity Index (CDAI). Gastroenterology. 1979 Oct;77(4 Pt 2):843–846. [PubMed] [Google Scholar]
- Das K. M., Vecchi M., Sakamaki S. A shared and unique epitope(s) on human colon, skin, and biliary epithelium detected by a monoclonal antibody. Gastroenterology. 1990 Feb;98(2):464–469. doi: 10.1016/0016-5085(90)90839-s. [DOI] [PubMed] [Google Scholar]
- Duerr R. H., Targan S. R., Landers C. J., LaRusso N. F., Lindsay K. L., Wiesner R. H., Shanahan F. Neutrophil cytoplasmic antibodies: a link between primary sclerosing cholangitis and ulcerative colitis. Gastroenterology. 1991 May;100(5 Pt 1):1385–1391. [PubMed] [Google Scholar]
- Duerr R. H., Targan S. R., Landers C. J., Sutherland L. R., Shanahan F. Anti-neutrophil cytoplasmic antibodies in ulcerative colitis. Comparison with other colitides/diarrheal illnesses. Gastroenterology. 1991 Jun;100(6):1590–1596. doi: 10.1016/0016-5085(91)90657-7. [DOI] [PubMed] [Google Scholar]
- Fiocchi C., Roche J. K., Michener W. M. High prevalence of antibodies to intestinal epithelial antigens in patients with inflammatory bowel disease and their relatives. Ann Intern Med. 1989 May 15;110(10):786–794. doi: 10.7326/0003-4819-110-10-786. [DOI] [PubMed] [Google Scholar]
- Goldschmeding R., van der Schoot C. E., ten Bokkel Huinink D., Hack C. E., van den Ende M. E., Kallenberg C. G., von dem Borne A. E. Wegener's granulomatosis autoantibodies identify a novel diisopropylfluorophosphate-binding protein in the lysosomes of normal human neutrophils. J Clin Invest. 1989 Nov;84(5):1577–1587. doi: 10.1172/JCI114335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korsmeyer S. J., Williams R. C., Jr, Wilson I. D., Strickland R. G. Lymphocytotoxic antibody in inflammatory bowel disease. A family study. N Engl J Med. 1975 Nov 27;293(22):1117–1120. doi: 10.1056/NEJM197511272932203. [DOI] [PubMed] [Google Scholar]
- Lennard-Jones J. E. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–19. doi: 10.3109/00365528909091339. [DOI] [PubMed] [Google Scholar]
- Lüdemann J., Utecht B., Gross W. L. Anti-neutrophil cytoplasm antibodies in Wegener's granulomatosis recognize an elastinolytic enzyme. J Exp Med. 1990 Jan 1;171(1):357–362. doi: 10.1084/jem.171.1.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldstone M. B. Molecular mimicry and autoimmune disease. Cell. 1987 Sep 11;50(6):819–820. doi: 10.1016/0092-8674(87)90507-1. [DOI] [PubMed] [Google Scholar]
- Roth M. P., Petersen G. M., McElree C., Vadheim C. M., Panish J. F., Rotter J. I. Familial empiric risk estimates of inflammatory bowel disease in Ashkenazi Jews. Gastroenterology. 1989 Apr;96(4):1016–1020. doi: 10.1016/0016-5085(89)91618-1. [DOI] [PubMed] [Google Scholar]
- Rump J. A., Schölmerich J., Gross V., Roth M., Helfesrieder R., Rautmann A., Lüdemann J., Gross W. L., Peter H. H. A new type of perinuclear anti-neutrophil cytoplasmic antibody (p-ANCA) in active ulcerative colitis but not in Crohn's disease. Immunobiology. 1990 Nov;181(4-5):406–413. doi: 10.1016/S0171-2985(11)80509-7. [DOI] [PubMed] [Google Scholar]
- Saxon A., Shanahan F., Landers C., Ganz T., Targan S. A distinct subset of antineutrophil cytoplasmic antibodies is associated with inflammatory bowel disease. J Allergy Clin Immunol. 1990 Aug;86(2):202–210. doi: 10.1016/s0091-6749(05)80067-3. [DOI] [PubMed] [Google Scholar]
- Snook J. A., Chapman R. W., Fleming K., Jewell D. P. Anti-neutrophil nuclear antibody in ulcerative colitis, Crohn's disease and primary sclerosing cholangitis. Clin Exp Immunol. 1989 Apr;76(1):30–33. [PMC free article] [PubMed] [Google Scholar]
- Sutherland L. R., Martin F., Greer S., Robinson M., Greenberger N., Saibil F., Martin T., Sparr J., Prokipchuk E., Borgen L. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology. 1987 Jun;92(6):1894–1898. doi: 10.1016/0016-5085(87)90621-4. [DOI] [PubMed] [Google Scholar]
- Takahashi F., Das K. M. Isolation and characterization of a colonic autoantigen specifically recognized by colon tissue-bound immunoglobulin G from idiopathic ulcerative colitis. J Clin Invest. 1985 Jul;76(1):311–318. doi: 10.1172/JCI111963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedesco F. J. Differential diagnosis of ulcerative colitis and Crohn's ileocolitis and other specific inflammatory disease of the bowel. Med Clin North Am. 1980 Nov;64(6):1173–1183. doi: 10.1016/s0025-7125(16)31562-0. [DOI] [PubMed] [Google Scholar]
- Wiik A. Delineation of a standard procedure for indirect immunofluorescence detection of ANCA. APMIS Suppl. 1989;6:12–13. [PubMed] [Google Scholar]
- van Hees P. A., van Elteren P. H., van Lier H. J., van Tongeren J. H. An index of inflammatory activity in patients with Crohn's disease. Gut. 1980 Apr;21(4):279–286. doi: 10.1136/gut.21.4.279. [DOI] [PMC free article] [PubMed] [Google Scholar]