Abstract
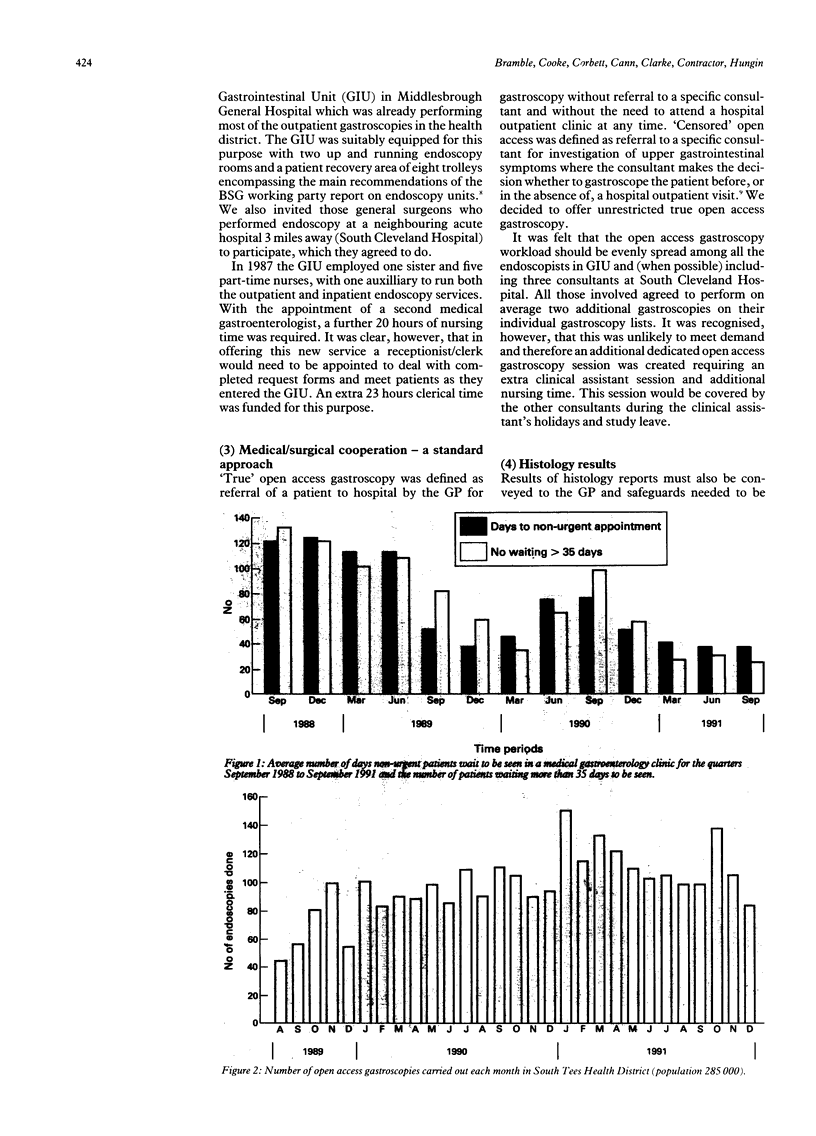
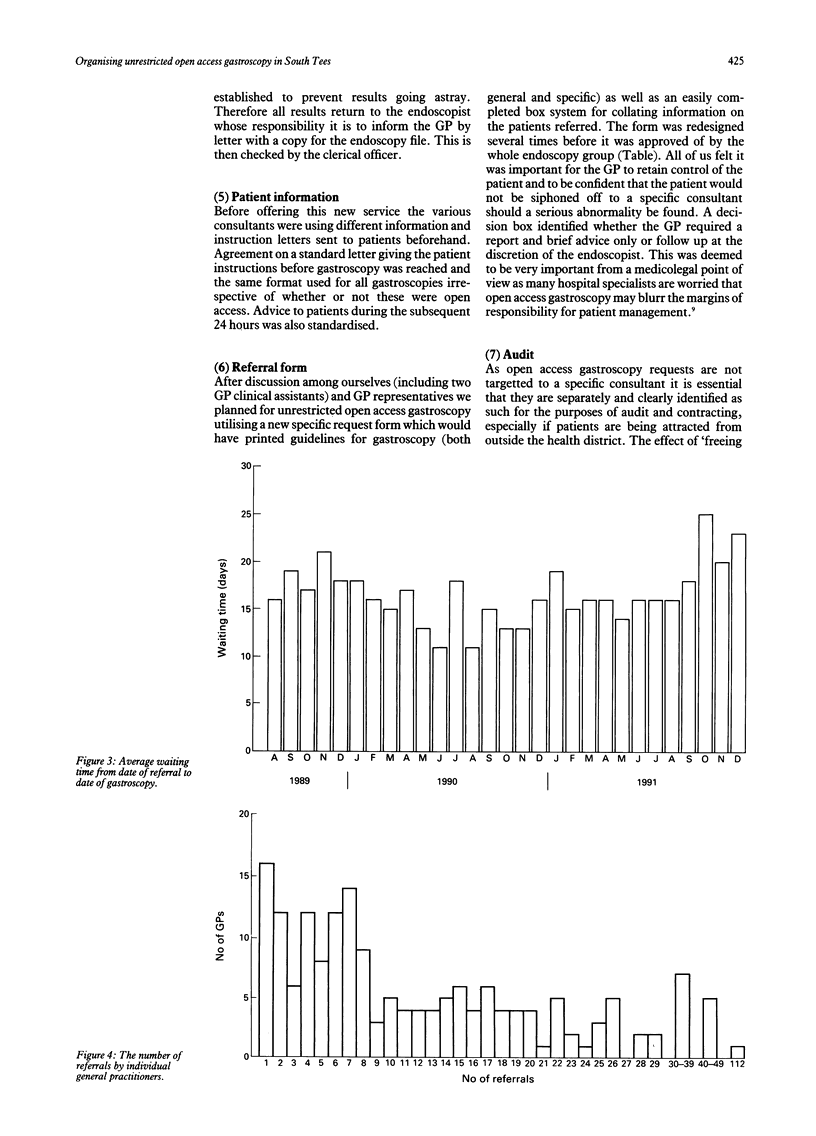
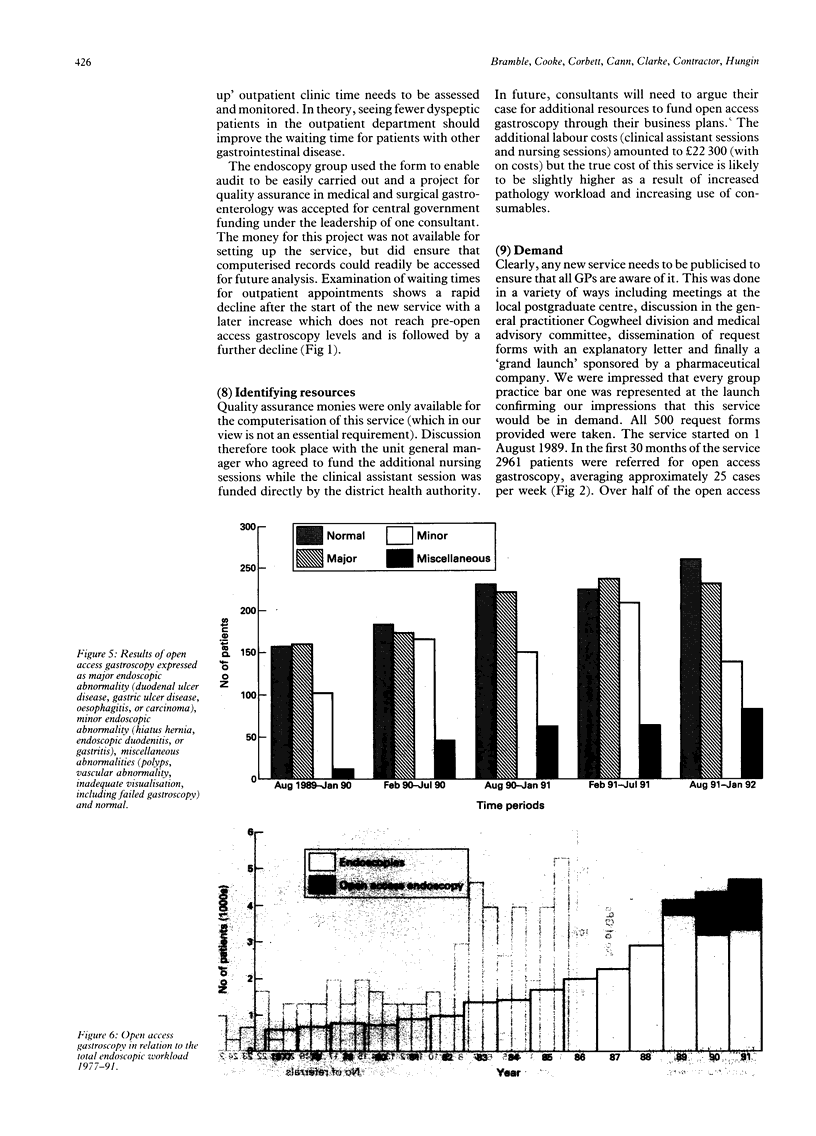
Increasing demand for upper gastrointestinal endoscopy has forced many clinicians to reconsider the policy of seeing all patients in a specialist clinic before gastroscopy. The following are considered essential in setting up an open access gastroscopy service. (1) Assessment of the need by examination of waiting times for the outpatient clinic and the proportion of patients requiring upper gastrointestinal endoscopy, and consultation with colleagues in general practice. During the first 2 years of the service the average waiting time for a medical gastrointestinal outpatient appointment has fallen from over 120 days to 37 days in this area. (2) An adequately staffed and equipped gastrointestinal unit with well motivated nurses (the workload will increase) and sufficient clinical support to allocate patients to the next available gastroscopy list is vital. A safe mechanism for relaying information back to the GP (including histology reports) is essential otherwise medicolegal problems could arise. Open access gastroscopy now accounts for 29% of the total endoscopy workload in South Tees. (3) Close cooperation between medical and surgical gastroenterologists must be achieved to ensure a uniform approach to the provision of this service and equal distribution of the endoscopy workload. This will require close examination of the potential numbers and may necessitate appointment of a clinical assistant or additional consultant. Clinical assistants perform just over 50% of the open access gastroscopies in South Tees and the waiting time has been kept short (average 17 days). (4) A comprehensive request form with guidelines for GPs and a specific box identifying whether the GP requires a report and brief advice only or follow up at the discretion of the endoscopist (often a clinical assistant) is required. (5) Management must be involved in identifying adequate resources. (6) Methods of monitoring requests and outcome measures to ensure effective audit must be established.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bramble M. G. Open access endoscopy--a nationwide survey of current practice. Gut. 1992 Feb;33(2):282–285. doi: 10.1136/gut.33.2.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J. A., Surridge J. G., Vartan C. P., Loehry C. A. Upper gastrointestinal endoscopy--a GP service. Br Med J. 1977 Nov 5;2(6096):1199–1201. doi: 10.1136/bmj.2.6096.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gear M. W., Wilkinson S. P. Open-access upper alimentary endoscopy. Br J Hosp Med. 1989 May;41(5):438, 440, 442-4. [PubMed] [Google Scholar]
- Holdstock G., Wiseman M., Loehry C. A. Open-access endoscopy service for general practitioners. Br Med J. 1979 Feb 17;1(6161):457–459. doi: 10.1136/bmj.1.6161.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrigan D. D., Brown S. R., Hutchinson G. H. Open access gastroscopy: too much to swallow? BMJ. 1990 Feb 10;300(6721):374–376. doi: 10.1136/bmj.300.6721.374. [DOI] [PMC free article] [PubMed] [Google Scholar]


