Abstract
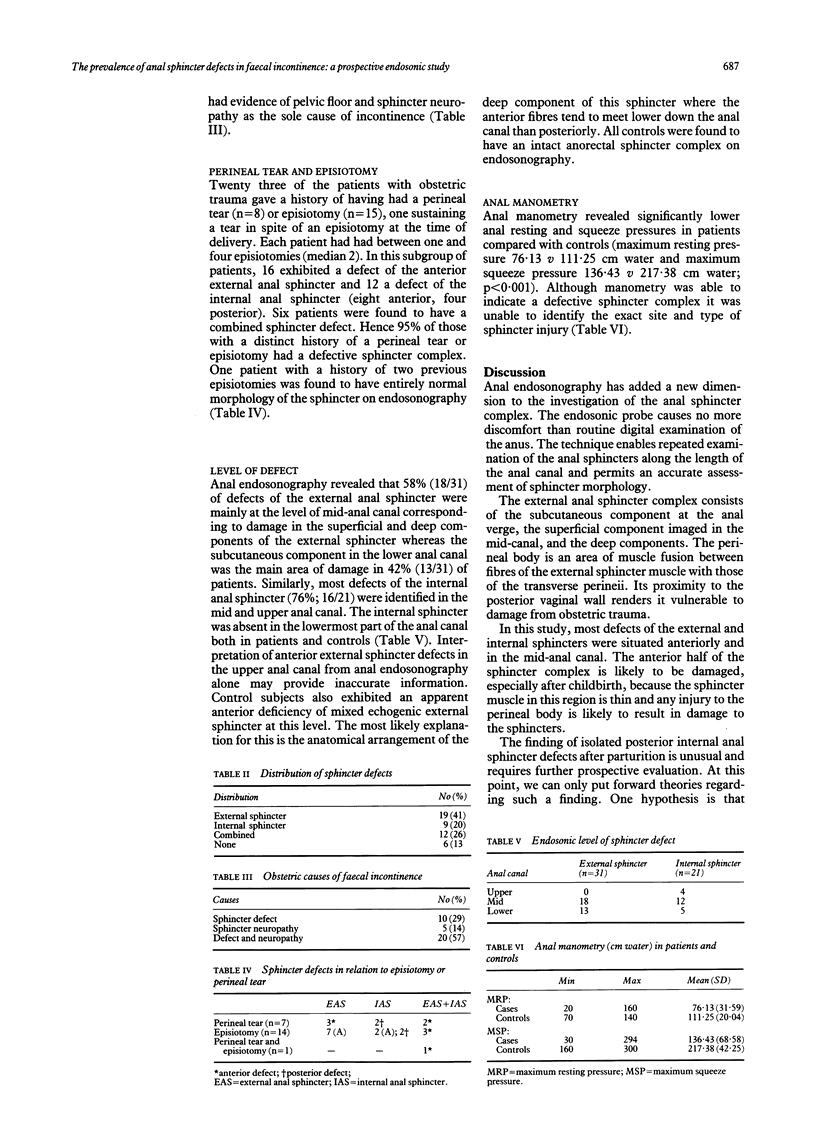
Forty six patients (median age 61 years; 42 women) with faecal incontinence and 16 age and sex matched controls undergoing a restorative proctocolectomy were assessed by clinical examination, anorectal physiology, and anal endosonography. Forty patients (87%) with faecal incontinence had a sphincter defect demonstrated on anal endosonography (31 external and 21 internal anal sphincter defects). The commonest cause of faecal incontinence was obstetric trauma. This occurred in 35 women, 30 of whom exhibited a morphological defect in the anorectal sphincter complex. In 22 of these patients with a history of a perineal tear or episiotomy, 21 (95%) had a sphincter defect. Sphincter defects were commonly located at the level of the midanal canal.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bartolo D. C., Jarratt J. A., Read N. W. The use of conventional electromyography to assess external sphincter neuropathy in man. J Neurol Neurosurg Psychiatry. 1983 Dec;46(12):1115–1118. doi: 10.1136/jnnp.46.12.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett S. J., Speakman C. T., Kamm M. A., Bartram C. I. Confirmation of endosonographic detection of external anal sphincter defects by simultaneous electromyographic mapping. Br J Surg. 1991 Apr;78(4):448–450. doi: 10.1002/bjs.1800780419. [DOI] [PubMed] [Google Scholar]
- Keighley M. R., Fielding J. W. Management of faecal incontinence and results of surgical treatment. Br J Surg. 1983 Aug;70(8):463–468. doi: 10.1002/bjs.1800700806. [DOI] [PubMed] [Google Scholar]
- Klosterhalfen B., Vogel P., Rixen H., Mittermayer C. Topography of the inferior rectal artery: a possible cause of chronic, primary anal fissure. Dis Colon Rectum. 1989 Jan;32(1):43–52. doi: 10.1007/BF02554725. [DOI] [PubMed] [Google Scholar]
- Law P. J., Bartram C. I. Anal endosonography: technique and normal anatomy. Gastrointest Radiol. 1989 Fall;14(4):349–353. doi: 10.1007/BF01889235. [DOI] [PubMed] [Google Scholar]
- Law P. J., Kamm M. A., Bartram C. I. Anal endosonography in the investigation of faecal incontinence. Br J Surg. 1991 Mar;78(3):312–314. doi: 10.1002/bjs.1800780315. [DOI] [PubMed] [Google Scholar]
- Orrom W. J., Miller R., Cornes H., Duthie G., Mortensen N. J., Bartolo D. C. Comparison of anterior sphincteroplasty and postanal repair in the treatment of idiopathic fecal incontinence. Dis Colon Rectum. 1991 Apr;34(4):305–310. doi: 10.1007/BF02050589. [DOI] [PubMed] [Google Scholar]
- Parks A. G., Swash M., Urich H. Sphincter denervation in anorectal incontinence and rectal prolapse. Gut. 1977 Aug;18(8):656–665. doi: 10.1136/gut.18.8.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wexner S. D., Marchetti F., Jagelman D. G. The role of sphincteroplasty for fecal incontinence reevaluated: a prospective physiologic and functional review. Dis Colon Rectum. 1991 Jan;34(1):22–30. doi: 10.1007/BF02050202. [DOI] [PubMed] [Google Scholar]
- Yoshioka K., Keighley M. R. Critical assessment of the quality of continence after postanal repair for faecal incontinence. Br J Surg. 1989 Oct;76(10):1054–1057. doi: 10.1002/bjs.1800761023. [DOI] [PubMed] [Google Scholar]
- Yoshioka K., Keighley M. R. Sphincter repair for fecal incontinence. Dis Colon Rectum. 1989 Jan;32(1):39–42. doi: 10.1007/BF02554724. [DOI] [PubMed] [Google Scholar]