Abstract
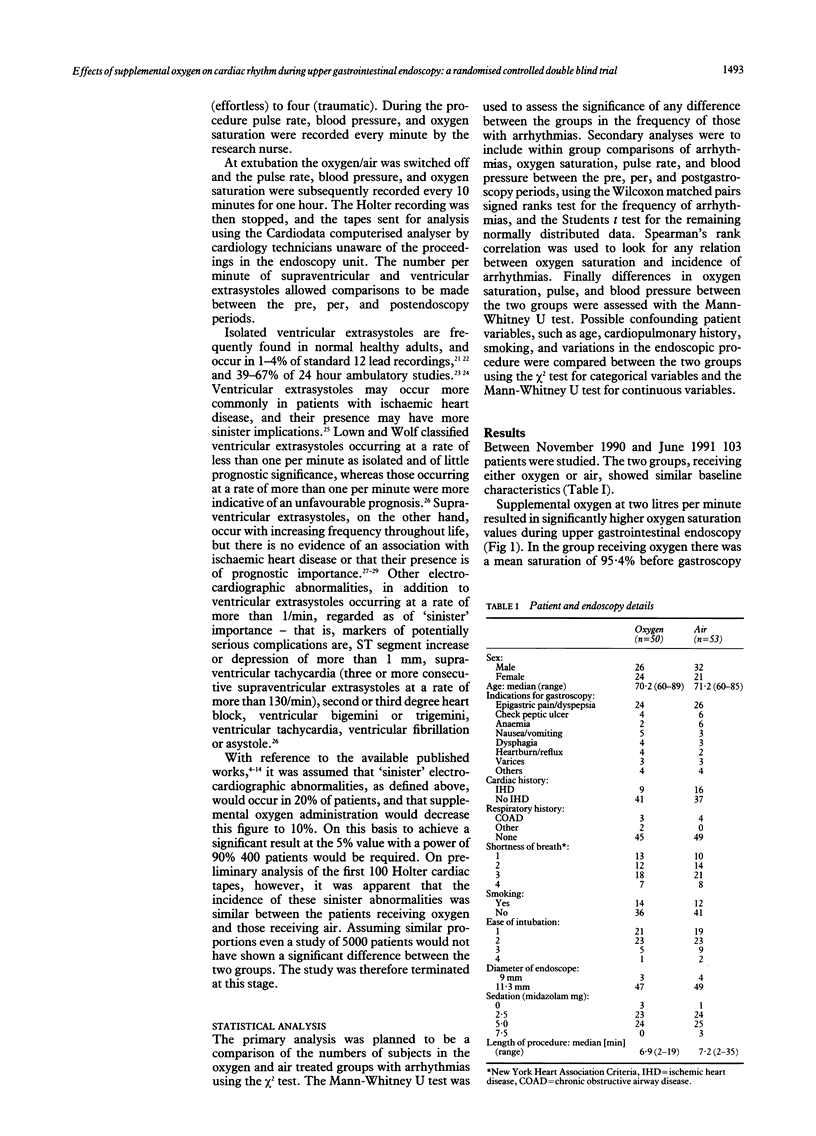
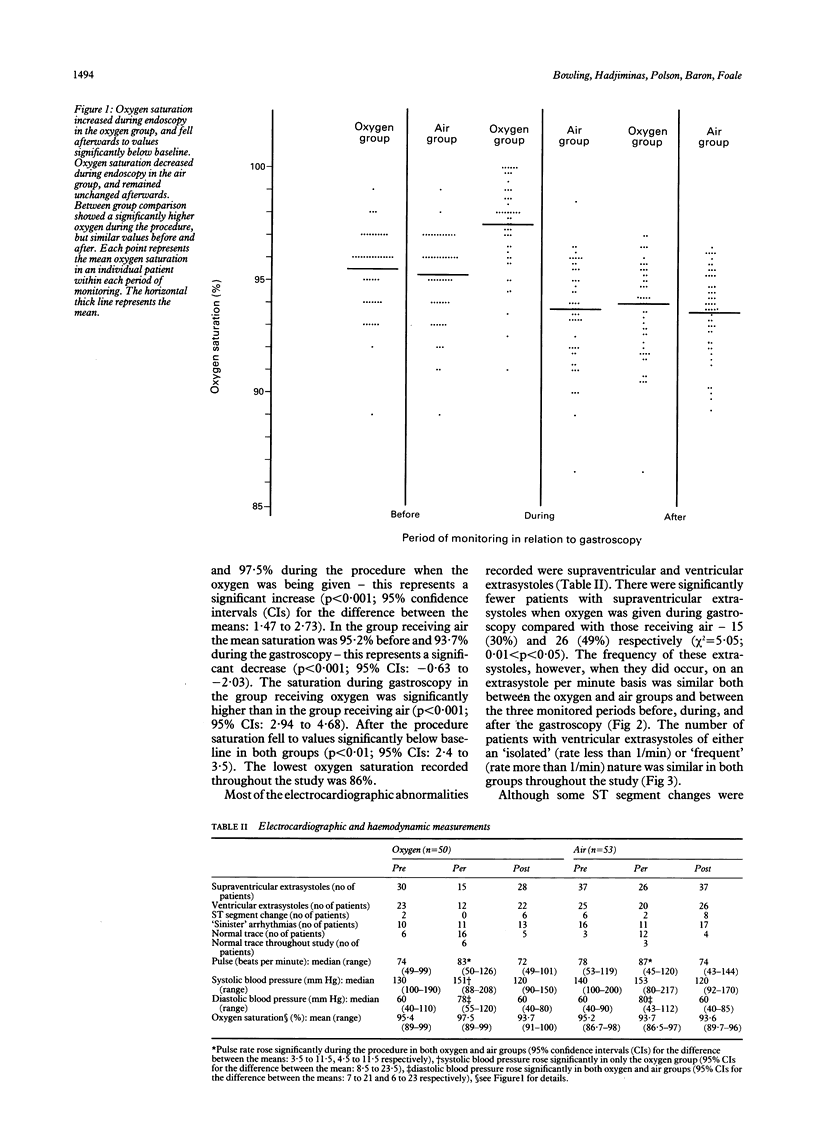
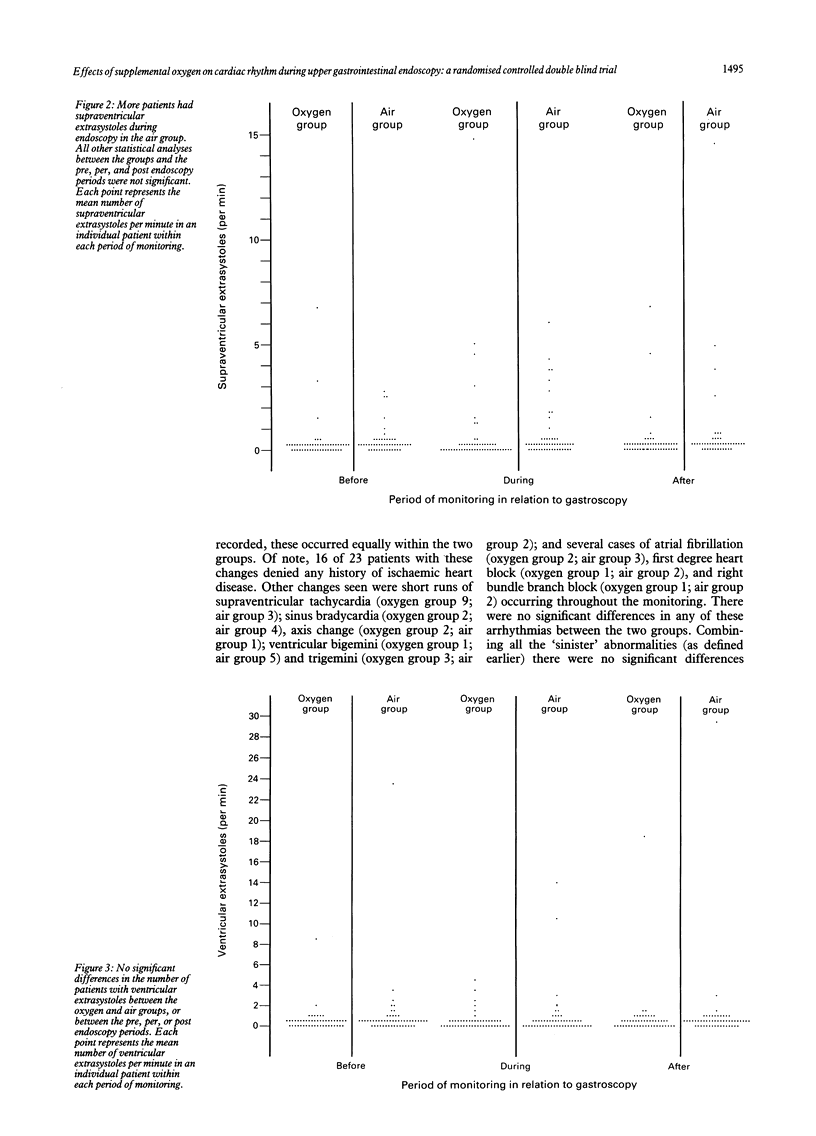
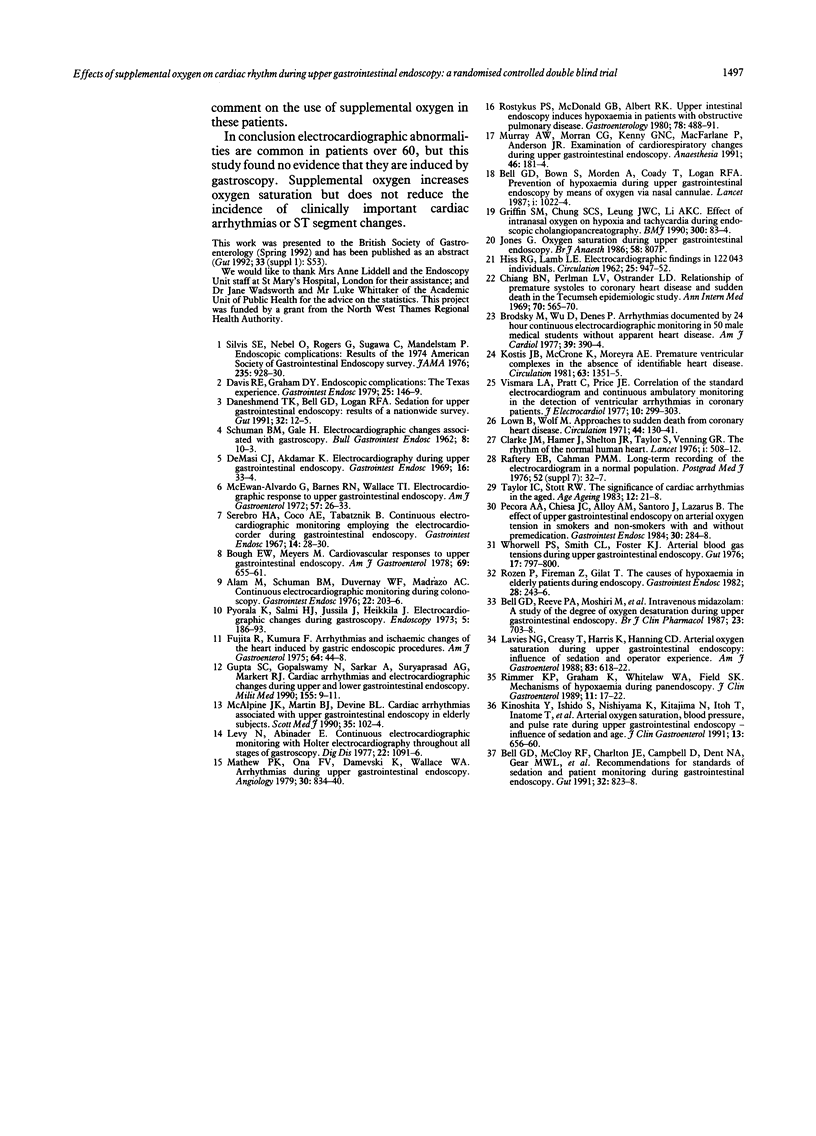
To investigate the effects of supplemental oxygen on cardiac rhythm during gastroscopy, 103 patients aged over 60 were randomised to receive either supplemental oxygen or air at 2 litres/minute during the procedure. Pulse rate, blood pressure, oxygen saturation, and a Holter cardiac trace were monitored before, during, and for one hour after the gastroscopy. A wide range of electrocardiographic abnormalities were recorded in both oxygen and air groups, of which ventricular and supraventricular ectopic beats were the most common. There were no significant differences in the rate of occurrence of any clinically important cardiac abnormality either between the oxygen and air groups or between the three monitored periods before, during, and after gastroscopy. There were significantly fewer patients, however, with supraventricular extra systoles when oxygen was given during gastroscopy (p < 0.05). Although supplemental oxygen during gastroscopy significantly improved oxygen saturation (p < 0.001; 95% confidence intervals for the difference between the means: 2.9 to 4.7), there was no correlation between oxygen saturation and any electrocardiographic changes. It is concluded that electrocardiographic abnormalities are common in patients over 60, but this study found no evidence that they are induced by gastroscopy. Supplemental oxygen increases oxygen saturation but does not reduce the incidence of clinically important cardiac arrhythmias.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alam M., Schuman B. M., Duvernoy W. F., Madrazo A. C. Continuous electrocardiographic monitoring during colonoscopy. Gastrointest Endosc. 1976 May;22(4):203–205. doi: 10.1016/s0016-5107(76)73754-4. [DOI] [PubMed] [Google Scholar]
- Bell G. D., Bown S., Morden A., Coady T., Logan R. F. Prevention of hypoxaemia during upper-gastrointestinal endoscopy by means of oxygen via nasal cannulae. Lancet. 1987 May 2;1(8540):1022–1024. doi: 10.1016/s0140-6736(87)92282-3. [DOI] [PubMed] [Google Scholar]
- Bell G. D., McCloy R. F., Charlton J. E., Campbell D., Dent N. A., Gear M. W., Logan R. F., Swan C. H. Recommendations for standards of sedation and patient monitoring during gastrointestinal endoscopy. Gut. 1991 Jul;32(7):823–827. doi: 10.1136/gut.32.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell G. D., Reeve P. A., Moshiri M., Morden A., Coady T., Stapleton P. J., Logan R. F. Intravenous midazolam: a study of the degree of oxygen desaturation occurring during upper gastrointestinal endoscopy. Br J Clin Pharmacol. 1987 Jun;23(6):703–708. doi: 10.1111/j.1365-2125.1987.tb03104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bough E. W., Meyers S. Cardiovascular responses to upper gastrointestinal endoscopy. Am J Gastroenterol. 1978 Jun;69(6):655–661. [PubMed] [Google Scholar]
- Brodsky M., Wu D., Denes P., Kanakis C., Rosen K. M. Arrhythmias documented by 24 hour continuous electrocardiographic monitoring in 50 male medical students without apparent heart disease. Am J Cardiol. 1977 Mar;39(3):390–395. doi: 10.1016/s0002-9149(77)80094-5. [DOI] [PubMed] [Google Scholar]
- Clarke J. M., Hamer J., Shelton J. R., Taylor S., Venning G. R. The rhythm of the normal human heart. Lancet. 1976 Sep 4;1(7984):508–512. doi: 10.1016/s0140-6736(76)90801-1. [DOI] [PubMed] [Google Scholar]
- Daneshmend T. K., Bell G. D., Logan R. F. Sedation for upper gastrointestinal endoscopy: results of a nationwide survey. Gut. 1991 Jan;32(1):12–15. doi: 10.1136/gut.32.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis R. E., Graham D. Y. Endoscopic complications: the Texas experience. Gastrointest Endosc. 1979 Nov;25(4):146–149. doi: 10.1016/s0016-5107(79)73405-5. [DOI] [PubMed] [Google Scholar]
- De Masi C. J., Akdamar K. Electrocardiography during upper gastrointestinal endoscopy. Gastrointest Endosc. 1969 Aug;16(1):33–34. [PubMed] [Google Scholar]
- Fujita R., Kumura F. Arrythmias and ischemic changes of the heart induced by gastric endoscopic procedures. Am J Gastroenterol. 1975 Jul;64(1):44–48. [PubMed] [Google Scholar]
- Griffin S. M., Chung S. C., Leung J. W., Li A. K. Effect of intranasal oxygen on hypoxia and tachycardia during endoscopic cholangiopancreatography. BMJ. 1990 Jan 13;300(6717):83–84. doi: 10.1136/bmj.300.6717.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S. C., Gopalswamy N., Sarkar A., Suryaprasad A. G., Markert R. J. Cardiac arrhythmias and electrocardiographic changes during upper and lower gastrointestinal endoscopy. Mil Med. 1990 Jan;155(1):9–11. [PubMed] [Google Scholar]
- HISS R. G., LAMB L. E. Electrocardiographic findings in 122,043 individuals. Circulation. 1962 Jun;25:947–961. doi: 10.1161/01.cir.25.6.947. [DOI] [PubMed] [Google Scholar]
- Kinoshita Y., Ishido S., Nishiyama K., Kitajima N., Itoh T., Inatome T., Inoh T., Fukuzaki H., Chiba T. Arterial oxygen saturation, blood pressure, and pulse rate during upper gastrointestinal endoscopy--influence of sedation and age. J Clin Gastroenterol. 1991 Dec;13(6):656–660. doi: 10.1097/00004836-199112000-00009. [DOI] [PubMed] [Google Scholar]
- Kostis J. B., McCrone K., Moreyra A. E., Gotzoyannis S., Aglitz N. M., Natarajan N., Kuo P. T. Premature ventricular complexes in the absence of identifiable heart disease. Circulation. 1981 Jun;63(6):1351–1356. doi: 10.1161/01.cir.63.6.1351. [DOI] [PubMed] [Google Scholar]
- Lavies N. G., Creasy T., Harris K., Hanning C. D. Arterial oxygen saturation during upper gastrointestinal endoscopy: influence of sedation and operator experience. Am J Gastroenterol. 1988 Jun;83(6):618–622. [PubMed] [Google Scholar]
- Levy N., Abinader E. Continuous electrocardiographic monitoring with Holter electrocardiocorder throughout all stages of gastroscopy. Am J Dig Dis. 1977 Dec;22(12):1091–1096. doi: 10.1007/BF01072863. [DOI] [PubMed] [Google Scholar]
- Lown B., Wolf M. Approaches to sudden death from coronary heart disease. Circulation. 1971 Jul;44(1):130–142. doi: 10.1161/01.cir.44.1.130. [DOI] [PubMed] [Google Scholar]
- Mathew P. K., Ona F. V., Damevski K., Wallace W. A. Arrhythmias during upper gastrointestinal endoscopy. Angiology. 1979 Dec;30(12):834–840. doi: 10.1177/000331977903001207. [DOI] [PubMed] [Google Scholar]
- McAlpine J. K., Martin B. J., Devine B. L. Cardiac arrhythmias associated with upper gastrointestinal endoscopy in elderly subjects. Scott Med J. 1990 Aug;35(4):102–104. doi: 10.1177/003693309003500403. [DOI] [PubMed] [Google Scholar]
- McEwan-Alvarado G., Barnes R. N., Wallace T. I. Electrocardiographic response to upper gastrointestinal endoscopy. Am J Gastroenterol. 1972 Jan;57(1):26–33. [PubMed] [Google Scholar]
- Murray A. W., Morran C. G., Kenny G. N., Macfarlane P., Anderson J. R. Examination of cardiorespiratory changes during upper gastrointestinal endoscopy. Comparison of monitoring of arterial oxygen saturation, arterial pressure and the electrocardiogram. Anaesthesia. 1991 Mar;46(3):181–184. doi: 10.1111/j.1365-2044.1991.tb09404.x. [DOI] [PubMed] [Google Scholar]
- Pecora A. A., Chiesa J. C., Alloy A. M., Santoro J., Lazarus B. The effect of upper gastrointestinal endoscopy on arterial O2 tension in smokers and nonsmokers with and without premedication. Gastrointest Endosc. 1984 Oct;30(5):284–288. doi: 10.1016/s0016-5107(84)72419-9. [DOI] [PubMed] [Google Scholar]
- Raftery E. B., Cashman P. M. Long-term recording of the electrocardiogram in a normal population. Postgrad Med J. 1976;52 (Suppl 7):32–38. [PubMed] [Google Scholar]
- Rimmer K. P., Graham K., Whitelaw W. A., Field S. K. Mechanisms of hypoxemia during panendoscopy. J Clin Gastroenterol. 1989 Feb;11(1):17–22. doi: 10.1097/00004836-198902000-00005. [DOI] [PubMed] [Google Scholar]
- Rostykus P. S., McDonald G. B., Albert R. K. Upper intestinal endoscopy induces hypoxemia in patients with obstructive pulmonary disease. Gastroenterology. 1980 Mar;78(3):488–491. [PubMed] [Google Scholar]
- Rozen P., Fireman Z., Gilat T. The causes of hypoxemia in elderly patients during endoscopy. Gastrointest Endosc. 1982 Nov;28(4):243–246. doi: 10.1016/s0016-5107(82)73101-3. [DOI] [PubMed] [Google Scholar]
- SCHUMAN B. M., GALE H. Electrocardiographic changes associated with gastroscopy. Bull Gastrointest Endosc. 1962 May;8:10–13. [PubMed] [Google Scholar]
- Serebro H. A., Cocco A. E., Tabatznik B. Continuous electrocardiographic monitoring employing the electrocardiocorder during gastrointestinal endoscopy. Gastrointest Endosc. 1967 Aug;14(1):28–30. [PubMed] [Google Scholar]
- Silvis S. E., Nebel O., Rogers G., Sugawa C., Mandelstam P. Endoscopic complications. Results of the 1974 American Society for Gastrointestinal Endoscopy Survey. JAMA. 1976 Mar 1;235(9):928–930. doi: 10.1001/jama.235.9.928. [DOI] [PubMed] [Google Scholar]
- Spergel G., Lustik B., Levy L. J., Ertel N. H. Studies of hypertension and carbohydrate intolerance associated with Wilms tumor. Ann Intern Med. 1969 Mar;70(3):565–570. doi: 10.7326/0003-4819-70-3-565. [DOI] [PubMed] [Google Scholar]
- Taylor I. C., Stout R. W. The significance of cardiac arrhythmias in the aged. Age Ageing. 1983 Feb;12(1):21–28. doi: 10.1093/ageing/12.1.21. [DOI] [PubMed] [Google Scholar]
- Vismara L. A., Pratt C., Price J. E., Miller R. R., Amsterdam E. A., Mason D. T. Correlation of the standard electrocardiogram and continuous ambulatory monitoring in the detection of ventricular arrhythmias in coronary patients. J Electrocardiol. 1977;10(4):299–304. doi: 10.1016/s0022-0736(77)80001-0. [DOI] [PubMed] [Google Scholar]
- Whorwell P. J., Smith C. L., Foster K. J. Arterial blood gas tensions during upper gastrointestinal endoscopy. Gut. 1976 Oct;17(10):797–800. doi: 10.1136/gut.17.10.797. [DOI] [PMC free article] [PubMed] [Google Scholar]


